Pupillary Block Glaucomas
TERMINOLOGY
Primary versus Secondary Angle-Closure Glaucomas
Angle closure is characterized by apposition of the peripheral iris against the trabecular meshwork, resulting in obstruction of aqueous outflow (see Chapter 7). The term glaucoma is used if there is evidence of glaucomatous optic nerve damage. Traditionally, some forms of angle-closure glaucoma have been referred to as primary angle-closure glaucoma because the mechanisms of angle closure were not thought to be associated with other ocular or systemic abnormalities or because the mechanisms were not well understood. Conditions that have been included in this group are pupillary block glaucoma, plateau iris, and combined-mechanism glaucoma. Other forms of angle-closure glaucoma have been called secondary angle-closure glaucoma because of associated ocular or systemic abnormalities or because of more apparent mechanisms of angle closure, such as contracting membranes or inflammatory precipitates that pull the angle closed or space-occupying lesions that push it closed. As continued research has expanded our knowledge of the associated abnormalities and mechanisms of primary angle-closure glaucomas, the distinction between the primary and secondary forms has become increasingly artificial, and the concept should probably be abandoned.
One example of how increased knowledge has progressively blurred the distinction between primary and secondary glaucomas is seen in the condition called plateau iris (1–3). This condition has traditionally been included with the primary angle-closure glaucomas. However, because of information regarding the mechanism of plateau iris, it is now considered to belong with the glaucomas associated with disorders of the iris and ciliary body (see Chapter 17).
In this chapter, we consider several forms of glaucoma that share the common mechanism of pupillary block and that have traditionally been grouped as primary angle-closure glaucomas. The conditions that have been called secondary angle-closure glaucomas are considered in subsequent chapters in this section.
Pupillary Block Glaucoma
Pupillary block glaucoma is the most common form of angle-closure glaucoma. The initiating event is thought to result from increased resistance to flow of aqueous humor between the pupillary portion of the iris and the anterior lens surface (4), which is associated with mid-dilatation of the pupil (5). The functional block produces increased fluid pressure in the posterior chamber, causing a forward shift of the iris. Anterior movement of the peripheral iris can result in closure of the anterior chamber angle (4–6) (Fig. 12.1). Four forms of pupillary block glaucoma may be distinguished on the basis of symptoms and clinical findings (7): acute angle-closure glaucoma, subacute angle-closure glaucoma, chronic angle-closure glaucoma, and combined-mechanism glaucoma.
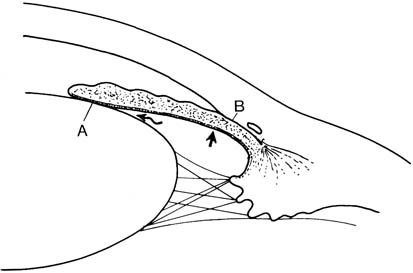
Figure 12.1 Pupillary block glaucoma. A functional block between the lens and iris (A) leads to increased pressure in the posterior chamber (arrows) with forward shift of the peripheral iris and closure of the anterior chamber angle (B).
Acute Angle-Closure Glaucoma
In acute angle-closure glaucoma, the symptoms are sudden and severe, with marked pain, blurred vision, and a red eye. The patient may also have nausea and vomiting.
Subacute Angle-Closure Glaucoma
Subacute angle-closure glaucoma is thought to have the same pupillary block mechanism as the acute form, but symptoms are mild or absent (8). The condition has also been called intermittent, prodromal, or subclinical (9). Patients with subacute angle-closure glaucoma may have repeated subacute or subclinical attacks before finally having an acute attack or developing peripheral anterior synechiae with chronic pressure elevation (8).
Chronic Angle-Closure Glaucoma
In chronic angle-closure glaucoma, portions of the anterior chamber angle are permanently closed by peripheral anterior synechiae, and the intraocular pressure (IOP) is chronically elevated (9,10). The synechial closure may result from a prolonged acute attack or repeated subacute attacks of angle-closure glaucoma. A variation of this condition has been called shortening of the angle or creeping angle-closure glaucoma (11,12). It is important to look carefully for evidence of exfoliation syndrome, because exfoliation can predispose to pupillary block in some patient populations (see Chapter 15).
Combined-Mechanism Glaucoma
In some eyes, the glaucoma appears to have open-angle and angle-closure mechanisms. The diagnosis is usually made after an acute angle-closure glaucoma attack in which the IOP remains elevated after a peripheral iridotomy, despite an open, normal-appearing angle.
EPIDEMIOLOGY
In most populations, pupillary block glaucoma is considerably less common than chronic open-angle glaucoma. However, there is a reversal in the ratio of angle-closure and open-angle glaucoma cases among Canadian, Alaskan, and Greenland Eskimos, with the former disorder occurring in approximately 0.5% of the general population and in 2% to 3% of those older than 40 years of age, with a predilection for women (13–16). A similar observation was made in population studies from China, Singapore, Mongolia, and South India and a mixed ethnic group in South Africa, in which the prevalence of angle-closure glaucoma was 2.3%, compared with 1.5% for chronic open-angle glaucoma (17–20). This prevalence of angle-closure glaucoma may be caused by a smaller corneal diameter and anterior chamber depth and a thicker, more anteriorly placed lens in affected individuals (21–23). A study among Alaskan Eskimos also showed a rapid increase in hyperopia after age 50, reaching 71.5% in persons older than 80 years (24).
Studies of the anterior chamber angle in various populations provide an impression of the prevalence of those at increased risk for pupillary block glaucoma. In two large studies, 5% to 6% of those screened had suspicious anterior chamber angles, but only 0.64% to 1.1% were considered to have critically narrow angles (25,26). In a Vietnamese population residing in the United States, 8.5% had critically narrow angles and were considered to be at high risk for occlusion (27).
CLINICAL FEATURES
The diagnosis of pupillary block glaucoma has several facets. During the course of every ocular examination, the physician must consider general risk factors in the medical history and look for anatomic features that may predispose to angle closure. The gold standard examination is gonioscopy, which is essential in identifying eyes with some form of angle closure or those at increased risk for angle-closure glaucoma (i.e., occludable angles). In other situations, the patient may present with signs and symptoms suggesting angle-closure glaucoma, and the correct diagnosis will depend on an understanding of the symptoms, predisposing circumstances, physical findings of the disease, and the differential diagnosis (Fig. 12.2). The various aspects of diagnosing potential or manifest pupillary block glaucoma are considered in this chapter.
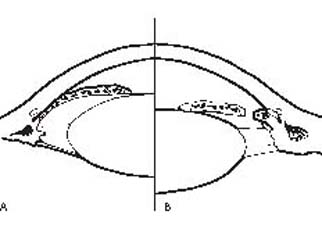
Figure 12.2 Pupillary block glaucoma (A) contrasted with the plateau iris syndrome (B). In the latter situation, notice the relatively deeper central anterior chamber, the flat iris plane, patent iridectomy, and bunching up of peripheral iris in the anterior chamber angle.
Risk Factors
General Features of Patients
Several factors influence the configuration of the anterior chamber angle and the risk for pupillary block glaucoma.
Age
The depth and volume of the anterior chamber diminish with age (28), which may result from thickening and forward displacement of the lens (29,30). Consequently, the percentage of individuals with critically narrow angles is higher in older age-groups. The prevalence of pupillary block glaucoma also increases with age, although it may peak earlier in life, compared with chronic open-angle glaucoma. One study found a bimodal pattern, with the first peak at ages 53 to 58 years and the second at 63 to 70 years (29). However, it can occur at any age, including rare cases in childhood (31).
Race
The relative prevalence of pupillary block glaucoma among all the glaucomas is increased in various populations of Inuit and individuals with Far Eastern Asian extraction (13–18). Acute angle-closure glaucoma is less common among blacks, but subacute or chronic angle-closure glaucoma is not uncommon and appears to be a regularly missed diagnosis (32–34). The explanation for this difference is uncertain. One study suggested that it might be caused by a thinner average lens thickness (33), although another investigation revealed the anterior chamber depth in Nigerian blacks to be equivalent to that of whites (35). The weaker response to mydriatics observed among African blacks could indicate that darker irides are less able to exert the force that may lead to acute pupillary block (36). Angle-closure glaucoma also has a reduced prevalence among American Indians and is often caused by a swollen lens when it does occur in this group (34).
Sex
There is a statistically significant predominance of females in populations with pupillary block glaucoma, which is probably because of the shallower anterior chamber among women in general (13,14,16,28).
Refractive Error
The depth and volume of the anterior chamber are related to the degree of ametropia, with smaller dimensions occurring in those with hyperopia (28). However, the presence of myopia does not eliminate the possibility of angle-closure glaucoma because rare cases have been reported in such patients (37), possibly indicting a spherical or anteriorly displaced lens or an increase in corneal curvature (38).
Family History
The potential for pupillary block glaucoma is generally believed to be inherited (see Chapter 8). In one study, 20% of 95 relatives of patients with angle-closure glaucoma were thought to have potentially occludable angles (39). However, aside from a few reported families in which many members developed angle-closure glaucoma, the family history is not very useful in predicting a future angle-closure attack (40).
Systemic Disorders
Researchers in one study found an inverse correlation between type 2 diabetes or an abnormal result on a glucose tolerance test and the anterior chamber depth (41). The same investigators also suggested that angle-closure glaucoma may be associated with an increased prevalence of denervation supersensitivity to autonomic agonists (42).
Findings on Routine Examination
Certain observations during the course of a routine ocular examination can help to establish the potential for angle closure.
Intraocular Pressure
Unless the patient has angle closure at the time of the examination, the IOP is usually normal. One study, however, found a larger-than-normal amplitude in the diurnal IOP curve, which the investigators thought might have prognostic value (43). Tonography also characteristically reveals normal outflow facility before or between attacks, unless peripheral anterior synechiae are present (5).
Evaluation of Peripheral Anterior Chamber
Photogrammetric studies of all forms of angle-closure glaucoma have revealed anterior chamber depths, volumes, and diameters that are smaller than those of matched controls (44). Anterior chamber depth and volume have also been shown to have diurnal variation, with lower values in the evening (45), although a correlation between diurnal variations of chamber depth and IOP is not clear. In any case, the most important step in the diagnosis of potential or manifest angle-closure glaucoma is to evaluate the anterior chamber depth and especially the configuration of the anterior chamber angle. Although this is best accomplished by gonioscopy, there are preliminary screening measures that may be useful in some situations and techniques of quantifying the anterior chamber depth.
Penlight Examination
When a slitlamp and goniolens are not available, the anterior chamber depth can be estimated with oblique penlight illumination across the surface of the iris. With the light coming from the temporal side of the eye, a relatively flat iris is illuminated on the temporal and nasal sides of the pupil, whereas an iris that is bowed forward has a shadow on the nasal side (46) (Fig. 12.3).
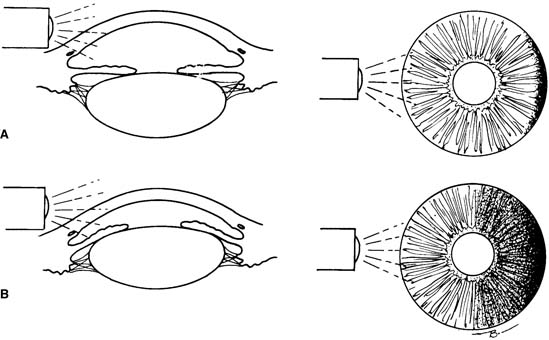
Figure 12.3 Oblique flashlight illumination as a screening measure for estimating the anterior chamber depth. A: With a deep chamber, nearly the entire iris is illuminated. B: When the iris is bowed forward, only the proximal portion is illuminated, and a shadow is seen in the distal half.
Slitlamp Examination
The central anterior chamber depth may be estimated during examination with the slitlamp, and several techniques for quantitating this parameter have been proposed (47–49). However, the central anterior chamber depth only weakly correlates with the angle width (50), and the parameter of greater diagnostic value in the context of angle-closure glaucoma is the peripheral anterior chamber depth. van Herick and colleagues (51) developed a technique for making this estimation with the slitlamp by comparing the peripheral anterior chamber depth to the thickness of the adjacent cornea (Figs. 12.4 and 12.5). This is commonly referred to as the van Herick technique. When the peripheral anterior chamber depth is less than one fourth of the corneal thickness, the anterior chamber angle may be potentially occludable.
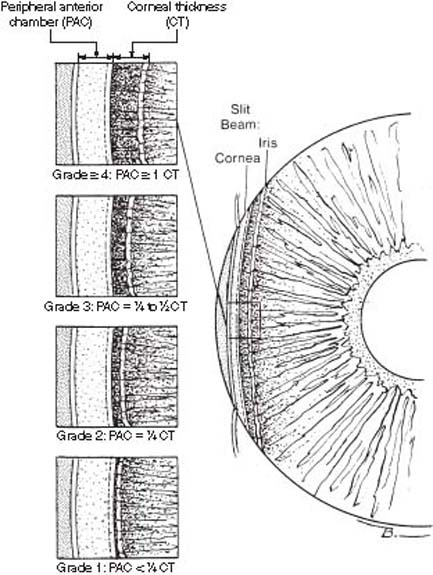
Figure 12.4 The slitlamp technique of van Herick and colleagues (51) is used for estimating the depth of the peripheral anterior chamber (PAC) by comparing it with the adjacent corneal thickness (CT). The PAC here is about 1 CT.

Figure 12.5 Slitlamp photograph of the van Herick technique for estimation of peripheral anterior chamber depth, showing the slit-beam on the cornea and iris.
Gonioscopy
When the peripheral anterior chamber depth is thought to be shallow (i.e., less than one fourth of the corneal thickness by van Herick slitlamp examination), careful gonioscopic examination of the angle is required. This is best accomplished with a Zeiss four-mirror lens or similar goniolens. A 180-or-more–degree closure of the angle (i.e., trabecular meshwork is not visible) constitutes an occludable angle, and it is important to use compression gonioscopy to determine whether the closure is appositional or synechial. The patient should be examined in a dark room and with the use of a short, narrow slit-beam to avoid constricting the pupil and artifactually opening the angle. The examiner also should take care to avoid extra pressure on the cornea so that the angle does not deepen artifactually. If necessary, the goniomirror on the Goldmann three-mirror lens can be used to avoid artifactual deepening of the chamber angle. If the peripheral iris is prominent, or the iris is very convex and it is difficult to see angle structures, it is often helpful to have the patient look in the direction of the mirror being viewed so that a more accurate assessment of what angle structures are visible can be made.
Numerous grading systems have been proposed to correlate gonioscopic appearance with the potential for angle closure. Scheie (52) proposed a system based on the extent of the anterior chamber angle structures that can be visualized (Fig. 12.6). He observed a high risk of angle closure in eyes with grade III or IV angles. Shaffer (1) suggested using the angular width of the angle recess as the criterion for grading the angle and attempted to correlate this with the potential for angle closure (Fig. 12.7).
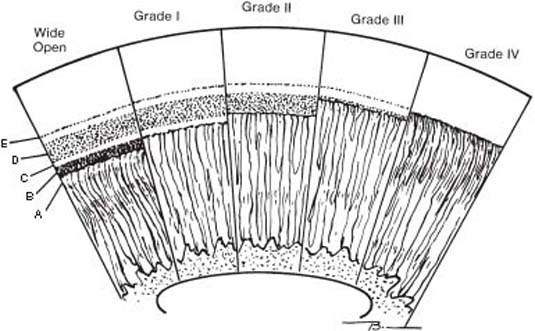
Figure 12.6 The Scheie gonioscopic classification of the anterior chamber angle, based on the extent of visible angle structures (52). A: Root of the iris. B: Ciliary body band. C: Scleral spur. D: Trabecular meshwork. E: Schwalbe line.
| Classification | Gonioscopic Appearance |
| Wide open | All structures visible |
| Grade I narrow | Hard to see over iris root into recess |
| Grade II narrow | Ciliary body band obscured |
| Grade III narrow | Posterior trabecula obscured |
| Grade IV narrow (closed) | Only Schwalbe line visible |
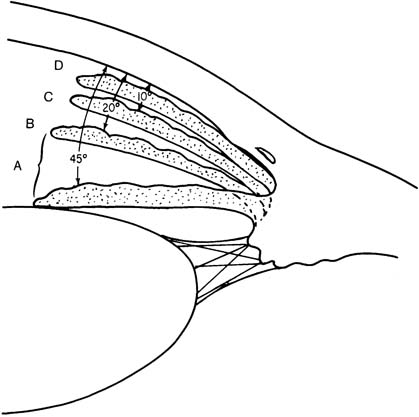
Figure 12.7 The Shaffer gonioscopic classification of the anterior chamber angle is based on the angular width of the angle recess (1). The angular width and clinical interpretation are given for each of the examples. A: Wide open (20 to 45 degrees): closure improbable. B: Moderately narrow (10 to 20 degrees): closure possible. C: Extremely narrow: closure possible. D: Partially or totally closed: closure present.
Other investigators think that any single criterion cannot fully describe the anterior chamber angle. Becker (53) proposed combining an estimation of the anterior chamber angle width and the height of the iris insertion, whereas Spaeth (26) suggested an evaluation of three variables: angular width of the angle recess, configuration of the peripheral iris, and apparent insertion of the iris root (Fig. 12.8). Whatever system the clinician prefers to use to document the appearance of the anterior chamber angle, it is important to pay close attention to these three aspects of the angle. One study proposed a relatively simple method for measurement of the distance from the iris insertion to the Schwalbe line using a reticule based in the slitlamp ocular during gonioscopy (54). The investigators called this technique biometric gonioscopy and found that it correlated well with other measures of anterior chamber angle, showing a higher degree of interobserver reliability than conventional gonioscopy. Additional features of the angle should also be studied and documented, such as peripheral anterior synechiae and degrees or abnormalities in pigmentation. One study found that patients with narrow angles may have a predominance of trabecular meshwork pigmentation in the superior quadrant, rather than the more common inferior location, which the investigators thought might be caused by rubbing between the peripheral iris and the meshwork (55).
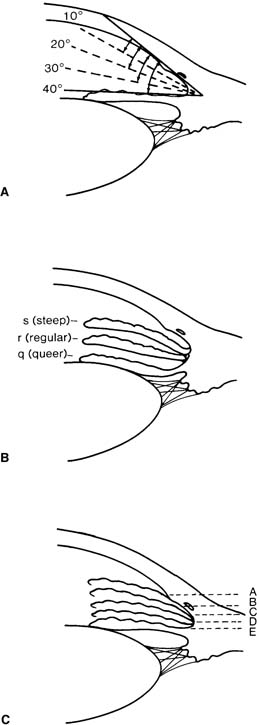
Figure 12.8 The Spaeth gonioscopic classification of the anterior chamber angle, based on three variables (26). A: Angular width of the angle recess. B: Configuration of the peripheral iris. C: Apparent insertion of the iris root.
Newer Techniques
Several newer forms of technology are being applied to evaluation of the anterior segment of the eye to more accurately quantify the anterior chamber depth and related dimensions. The use of high-frequency ultrasonography, referred to as ultrasound biomicroscopy, allows definition of the relationships of the iris, posterior chamber, lens, zonules, and ciliary body (see Chapter 3). This technique has potential value in understanding the mechanisms of glaucoma and in aiding the diagnosis of pupillary block glaucoma, especially when the media is not clear (56). It may also be of value in identifying eyes with potentially occludable anterior chamber angles. It has been suggested that anterior chamber depth measurement and the biometric calculation of the ratio of lens thickness to axial length can be used as a prognostic indicator of pupillary block glaucoma (57,58). Ultrasound biomicroscopy has also been used to image the dynamic changes in anterior ocular structures during provocative testing in a dark room (59,60).
Another technique that appears to be useful for assessing the relationship of the anterior chamber angle structures is optical coherence tomography (61) (see Chapter 3). Like ultrasound biomicroscopy, this technique is noninvasive and can provide a reasonable image of the anterior chamber angle. The main advantage is that it does not require the patient to have a probe with or without a gel or bath present on the eye; one drawback at present is that it does not appear to image structures posterior to the iris (e.g., ciliary body area) as well as ultrasound biomicroscopy does.
Specialized photographic techniques are also being used to better understand the anterior segment structures in angle-closure glaucomas. With one of these techniques, Scheimpflug video imaging, the iridocorneal angle can be quantitatively assessed and observed longitudinally (61).
When to Perform a Prophylactic Peripheral Iridotomy
Having decided that a patient has suspiciously narrow anterior chamber angles, the physician is faced with a difficult decision. If it could be predicted that the patient would eventually have an attack of angle-closure glaucoma, the appropriate course in most cases would be prophylactic peripheral iridotomies. The results of one study suggest that optic nerve damage occurs in the early period after IOP increases, supporting the value of detecting potentially occludable angles and performing prophylactic surgery before an attack (62).
If the angle is deemed occludable (i.e., 180 degrees or more of appositional angle closure), prophylactic peripheral iridotomy is warranted (see Chapter 35). The fellow eye should also be examined, and if deemed occludable, our recommendation is to proceed with iridotomy on both eyes at the same sitting.
Provocative Tests
Historically, some surgeons used tests to provoke pupillary block glaucoma when attempting to identify patients for whom treatment should be recommended. These tests included the prone test, the darkroom test, the prone darkroom test, and pharmacologic dilation of the pupil. The fourth edition of this textbook provides additional details on these tests.
Most ophthalmologists question the clinical value of any provocative test for angle-closure glaucoma because the false-positive and false-negative rates of such tests are high. In one study of 129 persons with suspected angle-closure glaucoma who underwent gonioscopy, refraction, anterior chamber pachymetry, ultrasound biomicroscopy, and an angle-closure provocative test, it was concluded that none of the test factors studied showed a high sensitivity or positive predictive accuracy in detecting eyes that later developed angle closure (63). Careful gonioscopic examination put into the context of available historical and clinical information has largely replaced the use of provocative tests to make management decisions about the development of angle-closure glaucoma (64).
Precipitating Factors
In an eye that is anatomically predisposed to develop angle closure, several factors may precipitate an attack.
Factors That Produce Mydriasis
Dim Illumination
A common history for the development of pupillary block glaucoma is the onset of an acute attack when the patient is in a dark room, such as a theater or restaurant. The incidence of angle closure is reported to increase in winter and autumn (65,66). In one study, however, there was a direct association with hours of sunshine and an inverse association with degree of cloudiness, which the investigators thought might be related to the contrast between day and evening levels of illumination (65).
Emotional Stress
Occasionally, an acute angle-closure attack follows severe emotional stress. This may be related to the mydriasis of increased sympathetic tone, although the exact mechanism is not understood.
Drugs
Use of mydriatic agents may precipitate an angle-closure attack in an anatomically predisposed eye. Use of anticholinergics (e.g., atropine, cyclopentolate, tropicamide) increases the risk for angle closure when administered topically (67). In one study, use of cyclopentolate, 0.5%, precipitated attacks in 9 (43%) of 21 high-risk eyes, and use of tropicamide, 0.5%, did the same in 19 (33%) of 58 eyes (68). However, in a population-based screening study of 4870 participants whose eyes were dilated with tropicamide, 1%, and phenylephrine, 2.5%, after penlight examination of the anterior chamber depth, none had an acute angle-closure attack (69). In another population-based study of 6760 persons, tropicamide, 0.5%, and phenylephrine, 5%, were used for diagnostic mydriasis (70). No persons were excluded on the basis of narrow angles, and only two participants (0.03%) experienced an attack of acute angle-closure glaucoma. Systemic atropine and other mydriatics can also create a hazard, especially when large doses are used in conjunction with spinal or general anesthesia during surgery (71). It has been suggested that high-risk eyes should be protected with topical pilocarpine before, during, and after surgery (72). However, miosis can also precipitate angle-closure attacks, and an alternative approach to managing the high-risk eye is close observation during the postoperative period or prophylactic peripheral iridotomy, depending on the degree of risk.
Other systemic drugs with weaker anticholinergic properties (e.g., antihistaminic, antiparkinsonian, antipsychotic, and gastrointestinal spasmolytic drugs) also present a risk proportional to their pupillary effect (68,73,74). The tricyclic antidepressants have the greatest anticholinergic properties of the various psychoactive drugs, and use of imipramine was believed to trigger pupillary block glaucoma in four reported cases (74). Botulinum toxin, used in the treatment of strabismus and blepharospasm, inhibits acetylcholine release with subsequent mydriasis, and it has been reported to cause acute angle-closure glaucoma (75).
Adrenergic agents (e.g., topical epinephrine) may precipitate an angle-closure attack in the predisposed eye. Phenylephrine can also precipitate an attack, although it was found to be safer than cyclopentolate or tropicamide for dilating high-risk eyes (71). Systemic drugs with adrenergic properties (e.g., vasoconstrictors, central nervous system stimulants, appetite depressants, bronchodilators, and hallucinogenic agents) may present a risk in the predisposed eye (67).
Factors That Produce Miosis
Miotic therapy may occasionally lead to an acute attack of pupillary block glaucoma. This has also been observed after the miosis induced by reading or bright lights. Possible mechanisms include an increase in the relative pupillary block due to a wider zone of contact between iris and lens and relaxation of the lens zonules, allowing a forward shift of the iris–lens diaphragm. With strong miotics, such as the cholinesterase inhibitors (e.g., di-isopropyl fluorophosphate, echothiophate iodide), the mechanism of angle closure may be the miosis or congestion of the uveal tract. Chandler (5) favored the former theory, because he observed that an acute increase in IOP after the use of a miotic did not occur in an eye with a peripheral iridectomy.
Symptoms of Angle-Closure Attack
Angle-closure glaucoma, in marked contrast to chronic open-angle glaucoma, is characterized by profound symptoms, although the severity of these symptoms varies considerably in different forms of the disorder.
Acute Angle-Closure Glaucoma
Acute angle-closure glaucoma is characterized by pain, redness, and blurred vision. The pain is typically a severe, deep ache that follows the trigeminal distribution and may be associated with nausea, vomiting, bradycardia, and profuse sweating. The marked conjunctival hyperemia usually consists of a ciliary flush and peripheral conjunctival congestion. The blurred vision, which is typically marked, may be caused by stretching of the corneal lamellae initially and later edema of the cornea, as well as a direct effect of the IOP on the optic nerve head. Rarely, the corneal decompensation may persist, requiring penetrating keratoplasty (76).
Subacute Angle-Closure Glaucoma
Subacute angle-closure glaucoma, a form of pupillary block glaucoma, may have no recognizable symptoms. In other cases, the patient may notice a dull ache behind the eye or slight blurring of vision. A symptom that is especially typical of the subacute attack is colored halos around lights. This is thought to result from corneal epithelial edema, which causes it to act as a diffraction grating, producing a blue–green central and yellow–red peripheral halo. These symptoms, which more often occur at night after the patient has been in a dark room, often spontaneously clear by the next morning, presumably because of the miosis of sleep.
Chronic Angle-Closure Glaucoma
Another form of pupillary block glaucoma, chronic angle-closure glaucoma, is typically asymptomatic until advanced visual field loss develops, although the patient may give a history suggestive of one or more episodes of subacute or acute angle-closure glaucoma.
Clinical Findings during an Acute Attack
The patient who presents during an acute angle-closure attack will typically have marked IOP elevation in the range of 40 mm Hg to greater than 60 mm Hg, with a profound reduction in central visual acuity. In the emergency room, digital palpation of the affected eye through a closed eyelid can be a helpful screening test, especially if a tonometer is not easily available. Digital palpation can reveal a very firm (i.e., rock-hard consistency) eye compared with the fellow eye, which feels much softer. The following additional findings help to confirm the diagnosis.
External Examination
Characteristic findings include conjunctival hyperemia, a cloudy cornea, and an irregular (usually vertically oval), mid-dilated, fixed pupil (Fig. 12.9). The pupillary change is thought to result from paralysis of the sphincter, which apparently is caused by a reduction in circulation induced by the elevated IOP and possibly by degeneration of the ciliary ganglion (77–80).
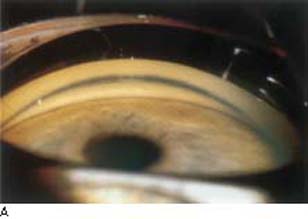

Figure 12.9 In these eyes with narrow angles, the iris is bowed forward in the periphery, as is typical of eyes with pupillary block. In (A), the anterior portion of the trabecular meshwork (dark band) is visible. In (B), the angle is even narrower, and only the Schwalbe line is visible, except for a possible thin rim of trabecular meshwork to the left of the view.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


