4 General Principles of Trauma Wounds are caused by external force and vary depending on the type and direction of the forces involved. They can be divided into: Abrasions are generally superficial mechanical injuries that for the most part involve the avascular epidermis. If the capillary loops in the dermal papillae are broken open in dot-like form, the wound will bleed and exudate heavily; exposure of the nerve endings in the corium makes these wounds very painful. They are also usually very dirty, with particles of dirt (from the road or dirt path) embedded in the skin. These wounds heal by epithelization without scarring, as the formation of replacement tissue is not necessary. Traumatic tattoos often remain. Puncture wounds are relatively small, superficial wounds which often exhibit minimal external blood loss. However, puncture wounds can penetrate very deeply and primary assessment is difficult. Depending on the object causing injury, wound edges may be smooth (knife, nail) or irregular (e. g., wood splinters). Puncture wounds are generally associated with a high risk of infection. Primary healing of puncture wounds occurs after surgery; otherwise healing is secondary. Cuts are caused by smooth, sharp objects (knife, glass, etc.) often leaving gaping wounds that can penetrate to deeper tissue layers. The wound edges are smooth and usually bleed heavily. There is generally no remarkable loss of tissue. Primary healing of cuts occurs after closure.
Cutaneous Wounds
Pathomechanism and Classification
 wounds caused by mechanical forces (Table 4.1).
wounds caused by mechanical forces (Table 4.1).
 thermally or chemically induced wounds.
thermally or chemically induced wounds.
Wounds Caused by Mechanical Forces
Abrasions
 Treatment, see Chapter 15: Principles of Wound Management—Abrasions, p. 130.
Treatment, see Chapter 15: Principles of Wound Management—Abrasions, p. 130.
Puncture Wounds
 Treatment, see Chapter 15: Principles of Wound Management—Puncture Wounds, p. 131.
Treatment, see Chapter 15: Principles of Wound Management—Puncture Wounds, p. 131.
Cuts
 Treatment, see Chapter 15: Principles of Wound Management—Cut Wounds, p. 131.
Treatment, see Chapter 15: Principles of Wound Management—Cut Wounds, p. 131.
Type of force | Direction of force | Wound form |
Sharp/cutting | Perpendicular, angled, flat/angled | Cut, flap wound, tissue defect |
Sharp/pointed | Perpendicular or angled | Penetrating wound |
Blunt, crushing | Perpendicular or angled | Crush wound, laceration |
Blunt, tearing | Flat or angled | Laceration |
Combined | Perpendicular or angled, tangential | Laceration/contusion, scratch, missile wound |
Bite Wounds
 Bites from small animals with pointy teeth (e. g., dogs, cats) resemble lacerations or puncture wounds. A small, often barely recognizable puncture on the surface and a large cavern deeper down are typical. Bleeding is often minimal or absent.
Bites from small animals with pointy teeth (e. g., dogs, cats) resemble lacerations or puncture wounds. A small, often barely recognizable puncture on the surface and a large cavern deeper down are typical. Bleeding is often minimal or absent.
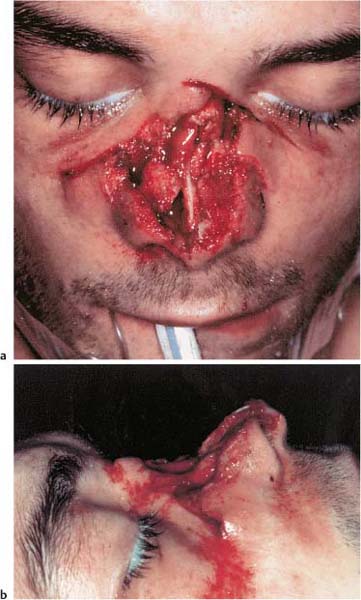
 Bites from animals with large molars (e. g., horses), on the other hand, cause crush wounds with jagged edges and heavy bleeding (cf. Fig. 4.1). Hematomas can usually be found in the surrounding area and the forces involved may also damage underlying structures such as bones.
Bites from animals with large molars (e. g., horses), on the other hand, cause crush wounds with jagged edges and heavy bleeding (cf. Fig. 4.1). Hematomas can usually be found in the surrounding area and the forces involved may also damage underlying structures such as bones.
 Human bite wounds can be recognized by the characteristic shape of the dental arcade formed by the individual teeth.
Human bite wounds can be recognized by the characteristic shape of the dental arcade formed by the individual teeth.
In general, bite wounds (whether from a human being or an animal) involve a high risk of infection as the wound is contaminated by bacteria found in saliva.
 Therapy, see Chapter 15: Principles of Wound Management—Bite Wounds, p. 131.
Therapy, see Chapter 15: Principles of Wound Management—Bite Wounds, p. 131.
Missile Wounds
Missile wounds are injuries caused by high velocity objects set in motion by explosive forces or under high local pressure.
Graze Wounds
In graze wounds the projectile does not penetrate the body, but creates a superficial furrow. Injury usually is limited to soft tissues, but can also involve larger vessels and nerves. Foreign bodies (particles of clothing, dirt) are often forced into the wound with the projectile, increasing the risk of contamination.
Through-and-Through Wounds
The projectile passes through the body or body part, injuring soft tissues and usually other important structures as well. Organ involvement can be determined by the missile tract.
In smooth-bordered missiles, such as pistol or rifle projectiles, the entry wound is generally small and circular, with only minimal bleeding. Tissue debris following in the projectile’s wake, however, causes a large, often heavily bleeding, exit wound with jagged edges.
Explosive or fragment projectiles, as well as flying debris (e. g., grenades, bomb shrapnel, mines, captive bolt guns, fragments from explosions as well as manipulated smoothly bordered bullets—dum dum bullets—and ricocheting projectiles) tear extensive, deep wound tracts and mangle large areas of tissue.
The actual extent of injury of through-and-through wounds can only be determined with diagnostic imaging or surgery. The energy released on impact can also damage neighboring, though not directly involved, structures (nerves, vessels). Risk of contamination is elevated by the foreign bodies entering the body with the force of the projectile.
Fig. 4.1 Bite wound to the nose from a dog.
a Frontal view. The skin, bone, and cartilage of the nose are missing.
b Lateral view. Marked depression of the nose due to the absence of nasal bone and cartilage.
Fig. 4.2 Retained missile underneath the left ear.
Retained Missile
In retained missile injury, projectile force is not sufficient to exit the body, and the projectile remains inside. Depending on type and caliber of the missile as well as the area of the body involved, severity of injury is more or less severe (Fig. 4.2).
Explosives containing small metal objects also belong to this category. The closer the range, the more devastating is their effect. Injury characteristically involves numerous, closely spaced, entry wounds and massive soft tissue injury.
Paintball Injury
High local pressure in a paintball gun causes fluids (e. g., dyes) or small particles to be injected deep into the tissues. Depending on type and composition of the penetrating substance, reactions to the foreign body and chronic inflammation with necrosis can be expected. These are usually delayed sequelae. The point of penetration (entry wound) is often initially unremarkable and the extent of damage is not readily observable.
 Treatment, see Chapter 15: Principles of Wound Management—Missile Wounds, p. 133.
Treatment, see Chapter 15: Principles of Wound Management—Missile Wounds, p. 133.
Thermal and Chemical Wounds
Burns
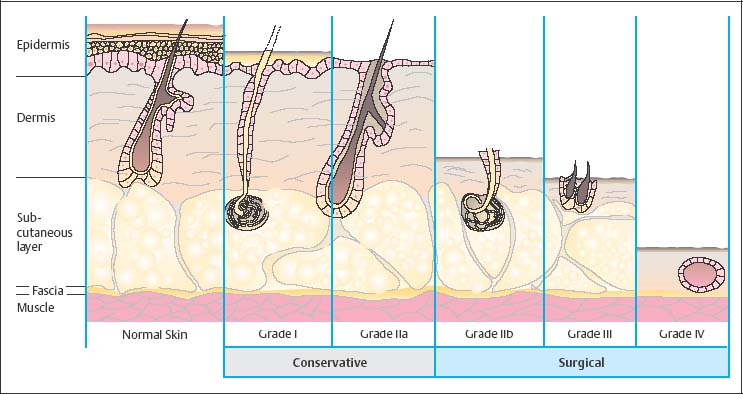
Poor heat transfer in soft tissue causes strong temperature gradients in tissue layers, even with only brief exposure to thermal action. In general, temperatures of 50– 60 C cause permanent tissue damage. With sufficiently long exposure, coagulation necrosis occurs in the uppermost layers of the skin. In the underlying regions, brief exposure leads to reversible damage and longer exposure to permanent damage. The depth of damage determines classification in varying degrees of severity (Table. 4.2 and Fig. 4.3).
Prognosis is based on the degree of severity as well as the extent of the burn injury over the body’s surface area. This can be calculated using the so-called “rule of nines”: a rule of thumb stating that the surface of the hand is about 1 % of the body’s surface area and that the head corresponds to about 9 % of the body’s surface area (see Fig.15.2).
 Treatment, see Chapter 15: Principles of Wound Management—Burn Injury, p. 133.
Treatment, see Chapter 15: Principles of Wound Management—Burn Injury, p. 133.
Burn degree | Description |
First degree | Damage is limited to the uppermost layers of the epidermis. The result is redness, swelling, tautness, and pain. Spontaneous wound healing through epidermal regeneration and without scar formation. |
Second degree | Thermal damage (coagulation, scabbing) extending into the dermis. Serous exudate elevates the upper layer of skin, causing the formation of burn blisters. Wounds are highly painful as nerve endings are intact. The moist wound basis are a high risk of contamination. Healing may occur spontaneously, from uninjured cutaneous appendages. |
Third degree | Full-thickness necrosis, wound base is dry, charred black or with white eschar. Sensation is completely lost. These wounds do not bleed, as vessels have been destroyed. |
Fourth degree | Injury of muscle and bone tissue as well. |
Fig. 4.3 Burn depth and skin layer involvement (modified from Bruck et al. 2002).
Chemical/Alkali Burns
Depending on concentration or pH value, as well as mode and duration of skin contact, acid or alkali substances can cause tissue injuries varying in severity and strongly resembling thermal burns. Because damaging chemical reactions—especially of alkalis—can potentially continue for hours until neutralized, the resulting wounds are necessarily deep, very painful, and heal poorly. Similar to thermal wounds, chemical burns are categorized in three grades (Table. 4.3).
Alkali burns cause a type of colliquation necrosis, whereby tissue liquefies with maceration. Wounds usually penetrate very deeply and have a greasy, white coating.
First degree | Redness |
Second degree | Blistering |
Third degree | Eschar |
Contact with acids, on the other hand, with resulting denaturation of tissue elements, causes firm, dry eschar (coagulation necrosis). Color depends on the acidic substance (e. g., hydrochloric acid causes white coloration, sulfuric acid causes black, nitric acid yellow, etc).
 Treatment, see Chapter 15: Principles of Wound Management—Chemical/Alkali Burns, p. 134.
Treatment, see Chapter 15: Principles of Wound Management—Chemical/Alkali Burns, p. 134.
Skin Healing
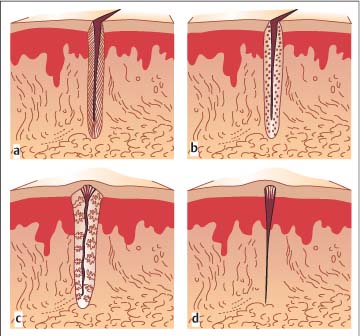
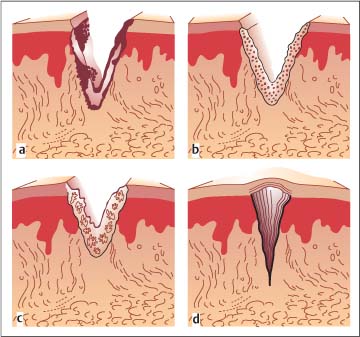
All of the above-mentioned injuries involve similar processes of skin regeneration (Figs. 4.4 and 4.5).
Fig. 4.4 Primary wound healing illustrated with the example of a surgical incision in the skin (from Schwenzer and Ehrenfeld, Vol. 1, 2000).
a Wound edges glued with fibrin sealant.
b Sprouting of vessels.
c Formation of granulation tissue with parallel epithelization.
d Transformation (organization) into narrow connective tissue scar.
Osseous Injuries
Pathomechanism and Classification
Osseous injuries can be divided in terms of pathomechanism into:
 direct fractures (the bone breaks at the site of the impacting force);
direct fractures (the bone breaks at the site of the impacting force);
 indirect fractures (break in the bone caused by bending, shearing, rotation, or compression forces or from avulsion at a distance from the site of impact).
indirect fractures (break in the bone caused by bending, shearing, rotation, or compression forces or from avulsion at a distance from the site of impact).
From a clinical standpoint, fractures can be divided into:
 closed fractures (i. e., soft tissue cover remains intact);
closed fractures (i. e., soft tissue cover remains intact);
 open fractures, which are further differentiated as shown in Table 4.4.
open fractures, which are further differentiated as shown in Table 4.4.
Depending on the course of the fracture line relative to the bone’s axis, one can distinguish between transverse, oblique, and longitudinal fractures as well as comminuted fractures (see Fig. 11.7, p. 111).
Defect fractures occur mainly in association with missile wounds.
In greenstick fractures the intact periosteal covering of the bone prevents displacement of bone fragments.
Fig. 4.5 Secondary wound healing (from Schwenzer and Ehrenfeld, Vol. 1, 2000).
a Covering of the tissue defect with protective fibrin coating and isolation from foreign bodies or necrosis, some sloughing.
b Initial vascularization of the lateral wound edges.
c Gradual filling of the defect with granulation tissue.
d Epithelization arising from the wound edges and organization in the replacement scar tissue.
Fracture Signs
 Direct, certain fracture signs are dislocation, abnormal mobility, and crepitation.
Direct, certain fracture signs are dislocation, abnormal mobility, and crepitation.
 Indirect, uncertain fracture signs are pain, swelling, hematomas, and functional limitation.
Indirect, uncertain fracture signs are pain, swelling, hematomas, and functional limitation.
Bone Healing
In principle, fracture healing involves the same processes as wound healing.
Grade I | Protruding through the skin from the inside out (small skin wound) |
Grade II | Injuries from external to internal with skin and muscle contusion (large skin wound) |
Grade III | Extensive skin, soft tissue, nerve, and vascular injuries |
Direct (Primary) Fracture Healing
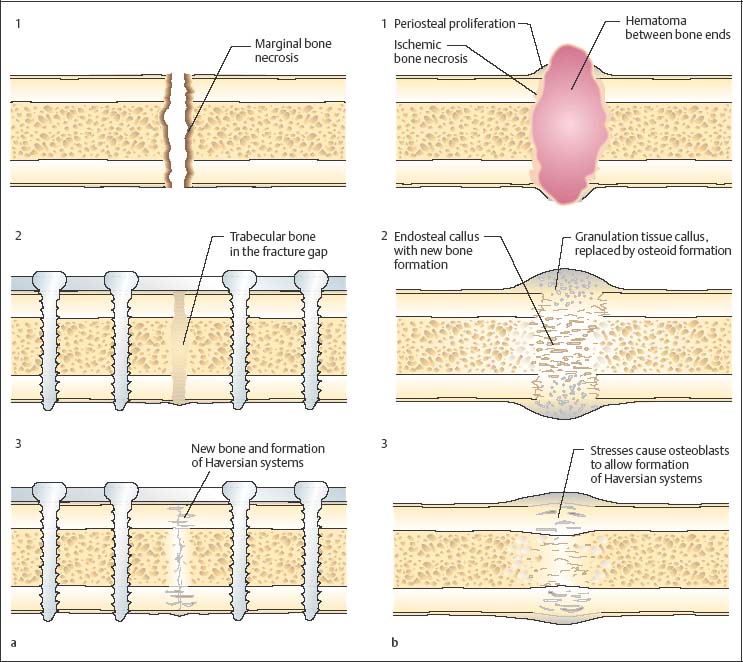
Primary fracture healing is only possible if the fractured ends of the bone can connect with each other following exact reduction and if the possibility of interfragmentary movement is completely eliminated by means of stable osteosynthesis. There are two types of fracture healing (Fig. 4.6a):
 contact healing;
contact healing;
 gap healing.
gap healing.
Contact Healing
In contact healing, the fracture ends, which are in direct apposition, become connected by means of proliferation of the Haversian systems. With complete stabilization, the osteones are able to reach one fracture end from the other.
Fig. 4.6 Fracture healing (modified from David and Simpson 1995).
a Gap healing.
1 Gap between the bones.
2 After immobilizing the fracture with a plate, the gap is filled with lamellar bone.
3 Reconstitution of the Haversian systems.
b Secondary fracture healing.
1 Hematoma between the fracture ends.
2 Callus formation fills the defect.
3 Remodeling of the callus under stress into lamellar bone.
Gap Healing
Inexact reduction of the fracture ends results in a gap. Narrow gaps are filled in with lamellar bone, while wider gaps are divided into small chambers by fibrous trabecular bone, which in turn are also filled by lamellar bone.
Indirect (Secondary) Fracture Healing
The least amount of instability will result in secondary fracture healing.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree