Voice rehabilitation after transoral laser microsurgery to the larynx is challenging. We wait at least 6 months before surgical intervention. Only a few patients after total or extended cordectomy requested voice restoration. Subjective perception of voice using the Voice Handicap Index in medialization thyroplasty was significantly better. Medialization thyroplasty with elevation of the fibrous tissue from the inner surface of the thyroid cartilage is critical in achieving success. We preferred the Montgomery Thyroplasty Implant System. Transoral larynx anterior commissure stent placement after laser-assisted sectioning of anterior synechiae with application of mitomycin C is an effective procedure for anterior synechiae.
Key points
- •
Voice degradation is commonly seen after ELS types III to VI cordectomies.
- •
Anterior synechiae and glottic gap after cord resection are the commonest causes of postoperative dysphonia.
- •
Lichtenberger’s technique is useful in treating anterior synechiae.
- •
Medialization thyroplasty using the Montgomery implant helps reduce the glottic gap and improve voice.
Early laryngeal cancer treatment is primarily concerned with establishing cure while preserving voice and swallow function. Treatment options include radiotherapy or surgery – open or endoscopic with similar oncologic effectiveness and identical survival rates (cause-specific survival rate ≥90%). The last 20 years has demonstrated a shift in practice away from open surgical procedures to transoral surgery with satisfactory oncological outcomes. Comparisons made between endoscopic laser microsurgery of early laryngeal cancer, open surgery and radiotherapy have also shown little difference in voice outcomes.
Local control is similar between radiotherapy and surgery and the functional disadvantages after surgery are moderate and counterbalanced by a significantly higher rate of long-term laryngeal preservation (90.1% after radiotherapy vs 97.4% after surgery). Other advantages of the endoscopic approach include its cost-effectiveness and less limitation for future treatment options in case of failure.
Patients undergoing less extensive microsurgery for early glottic cancer (European Laryngological Society [ELS] types I and II) are found to have mild dysphonia, which rarely requires further surgery and responds well to voice therapy. Full voice recovery is seen in subepithelial cordectomy (ELS type I) and is near complete in type II subligamental cordectomy. Supraglottic postoperative voice compensation is rarely if ever seen in these 2 cohorts. However, this is not the case in more extensive cordectomies, in which, although voice compensation does take place albeit at a reduced level, supraglottic contraction becomes more evident, as does compensation from part or the whole of the contralateral cord, the resulting fibrotic operated cord remnant (the neocord), or the ventricular folds.
Voice degradation is seen usually after more extensive levels of cordectomy (ELS types III–V). Patients routinely undergo a minimum 6 months of voice rehabilitation with speech therapy before consideration of surgical management of dysphonia. Endoscopic and open laryngeal surgical options (thyrotomy/laryngofissure approach) are available depending on the sequelae from the primary surgical resection. We propose a step-by-step management algorithm to voice rehabilitation after endoscopic surgery (our experience) and discuss the pros and cons of the more established procedures based on experience gained in this challenging area. Open procedures and voice restoration thereafter are discussed.
Voice quality after laser microsurgery is predominantly affected by the presence of synechiae at the anterior commissure. However, the quantity of vocal cord removed and the ensuing glottic gap play significant roles in postoperative dysphonia.
Several phonosurgical procedures have been developed to deal with the resulting glottic gap and anterior commissure synechiae and in so doing aim to improve phonation. We describe our experience in this regard and also take the opportunity to mention other procedures performed for these sequelae of early laryngeal surgery.
Materials and methods
Patients
Two hundred and fifty-one patients underwent a total of 311 CO 2 laser-assisted endoscopic cordectomies in our department between 1998 and 2012. The data of the performed procedures according to each type of cordectomy are reported in Table 1 . Fifty-eight patients (23.1%) had more than 1 cordectomy during this period, all of whom had 2 procedures, with the exception of 1, who underwent 4. The cordectomies were classified using the revised terminology proposed in 2007 by the ELS. The revision includes a new endoscopic cordectomy (type VI) for cancers of the anterior commissure, extended to one or both of the vocal folds, without infiltration of the thyroid cartilage.
| Type of Cordectomy | No. of Procedures (Total = 311) (%) | No. of Patients (Total = 251) (%) |
|---|---|---|
| I | 138 (44.4) | 64 (25.5) |
| II | 42 (13.5) | 21 (8.4) |
| III | 42 (13.5) | 32 (12.7) |
| IV | 27 (8.7) | 21 (8.4) |
| V | 55 (17.7) | 49 (19.5) |
| VI | 7 (2.3) | 6 (2.4) |
| Combination | — | 58 (23.1) |
All patients underwent speech therapy after establishment of the scarring process to the operated cord (ie, full development of the neocord). Total or near-total voice recovery was almost always the rule after subepithelial (type I) or subligamental (type II) cordectomies. Supraglottic contraction, although often observed after transmuscular (type III) cordectomy, did respond well to voice rehabilitation, assuming no anterior synechiae were present as well. More extended cordectomy rendered the ipsilateral cord nonfunctional, and voice compensation was obtained from the contralateral healthy cord or the false (ventricular) folds.
Fourteen patients (5.6%) self-assessed their postoperative voice quality as insufficient, complaining of persistent dysphonia and breathiness. There were 12 men and 2 women (9 with T1 cancer and 5 with T2), with a mean age of 53.7 years (range 25–82 years) who underwent a total or extended total (13 patients) cordectomy. One patient with an anterior commissure cancer extending up to the anterior third of both cords underwent a type VI cordectomy. A type V cordectomy was performed on the 5 patients with T2 cancer as well as 3 others with T1b disease.
In addition, 10 patients developed anterior synechiae after total and extended total cordectomy or type VI cordectomy.
Voice Assessment Tools
Voice assessment was performed preoperatively and at regular intervals according to the recommendations of the Committee on Phoniatrics of the ELS. We obtained complete preoperative and postoperative data on 13 of the 14 patients who underwent medialization thyroplasty and all patients who had surgery for anterior synechiae.
Self-evaluation of voice by our patients included the Voice Handicap Index (VHI) questionnaire, which includes the physical, functional and emotional impact of the voice disorder and consists of 30 questions, each rated from 0 to 4, in increasing order of the severity of symptoms. Perceptual voice quality was evaluated with the GRBAS (Grade Roughness Breathiness Asthenia Strain) scale by Hirano. G (overall grade) and R (roughness) (for anterior synechiae) were singled out and rated by a speech therapist with experience in voice assessment.
Aerodynamic measurements included maximum phonation time (MPT; normal range 20–25 seconds) and the phonation quotient (PQ; mL/s) (ie, the quotient obtained by dividing vital capacity with the MPT). We used the best score from 3 successive attempts of the sound “a” for the MPT at a comfortable loudness level.
Maximum fundamental frequency (Fo-high, Hz), as well as lower intensity (I-low, dB) were also calculated in medialization thyroplasty cases and the frequency range (FR, Hz) and fundamental frequency (F0) were analyzed in anterior synechiae surgery. Voice analysis was performed using the Multi Dimensional Voice Program (MDVP) (Kay Elemetrics, Lincoln Park, NJ; KayPENTAX).
Medialization Thyroplasty
Medialization thyroplasty is performed at least 6 months after cordectomy. This is considered the minimum safe period before attempted voice restoration allowing for complete healing of the larynx after laser microsurgery, formation of the neocord, assurance of no residual or recurrent disease, and voice rehabilitation accomplished with adequate voice therapy alone. The procedure is performed under general anesthesia using a laryngeal mask airway (LMA). Transnasal flexible videoendoscopy is carried out to evaluate the degree of glottic gap reduction, and this is feasible through a small valve in the joint that connects the LMA to the ventilation tube. We can assess surgical progress and completion of the thyroplasty by observing the video image captured by the camera attached to the scope without hampering the patient’s ventilation.
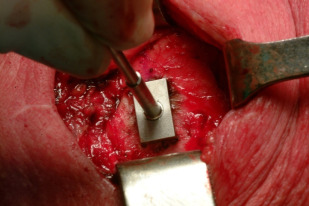
The landmarks for creating the window in the thyroid cartilage have been slightly modified according to the different implants used over the period that the procedure has been performed. Meticulous care is taken in dissecting the inner wall of the thyroid cartilage from the fibrous neocord, ensuring close contact with the cartilage at all times, especially when the inner perichondrium was unidentifiable. Furthermore, the dissection has to be extensive enough to facilitate insertion of the implant without fibrous tissue resistance or tear. The technical difficulty of this dissection distinguishes it from medialization procedures for cord immobility, which are easier and therefore more amenable to be performed under local anesthesia ( Figs. 1 and 2 ).

Three types of implants have been successfully used. The preformed Vocom hydroxyapatite implant (Smith-Nephew, Memphis, TN), the Gore-Tex implant (Gore Thyroplasty Device, WL Gore and Associates, Flagstaff, AZ), and the Montgomery Thyroplasty Implant System (MTIS, Boston Medical Products, Westborough, MA). The Vocom implant was used primarily in 2 (14.2%) patients, the Gore-Tex in 1 (7.1%) patient, and the MTIS in 11 (78.6%) patients. A revision thyroplasty was required in only 1 case in which a Vocom implant was replaced by an MTIS.
We use quick-setting Tissucol fibrin glue (Baxter, Vienna, Austria) to cover the medialization thyroplasty window and leave a small suction drain in the wound for 24 hours before skin closure. We have found that the routine use of fibrin glue is useful in closing any potential defects between the neck and glottis. All patients are placed on postoperative broad-spectrum antibiotics (eg, co-amoxiclav) for 5 days. Voicing at a low intensity is recommended routinely after, and patients are allowed to eat the same evening of the procedure and discharged after drain removal.
Surgery for Anterior Synechiae (Lichtenberger Technique)
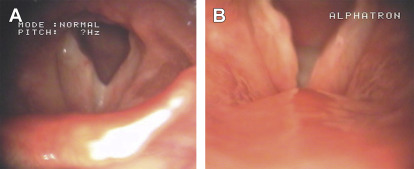
Our favored method to deal with anterior glottic webs is that described by Lichtenberger and Toohill. The procedure is performed endoscopically under general anesthesia using suspension laryngoscopy and subglottic jet ventilation ( Fig. 3 ). The laryngoscope is carefully placed at 3 to 4 mm above the anterior commissure to allow for easy placement of the silastic stent. The web is cut using a CO 2 laser with scanning facilities (Acublade system, Lumenis, Santa Clara, CA) at 10 W power in superpulse mode. The Acublade laser scanning system allows the traveling of the laser wave on a straight line. Depending on the length of the line and the type of mode selected (continuous or superpulse), the system calculates the appropriate power. The cut is made in the middle of the web and care taken to extend the section up to the anterior angle of the thyroid cartilage. A cottonoid soaked with mitomycin C (2 mg/mL) is then applied twice at the surgical site for 2 minutes per application.

The stent used initially was handmade and consisted of a 0.25-mm-thick silastic sheet, which was folded on itself and glued with silicone glue (Dow Corning, Midland, MI). A small tract allowing the passage of a Dermalon 2/0 thread was created by inserting a pediatric epidural needle when folding the silastic sheet. We now use a preshaped stent, the larynx anterior commissure stent (LACS, Boston Medical, Westborough, MA), which we tailor according to dimensions of the web and larynx.
Under direct endoscopic vision using a 30° rigid scope and a Lichtenberger needle holder ( Fig. 4 ) (R Wolf 826750; M 954790), the LACS is fixed at the anterior commissure after sizing of the anteroposterior and superoinferior dimensions described earlier. The stent is rectangular and spans the commissure for 2 to 3 mm above and below it. The nonresorbable 00 sutures are passed through the larynx to the skin. The inferior puncture is performed first and lies below the anterior commissure and passes through the cricothyroid membrane. The superior puncture site is usually at the median of the thyroid cartilage but may vary depending on the calcification of the cartilage and may therefore be higher (eg, the base of the epiglottis) (this does not change the size of the splint). The suture is passed through a button or a silastic sheet that separates it from the skin of the neck ( Fig. 5 ).

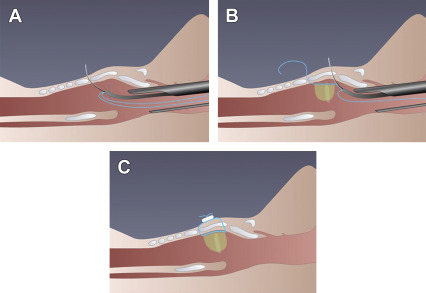
All patients are given a week’s course of a broad-spectrum antibiotic (eg, co-amoxiclav), 6 weeks of twice daily proton pump inhibitors, and inhaled corticosteroids twice daily for a week. They are encouraged to rest their voice for a week postoperatively and are reviewed weekly to assess the position of the stent, which is then removed 3 weeks after the procedure ( Figs. 6 and 7 ).

Materials and methods
Patients
Two hundred and fifty-one patients underwent a total of 311 CO 2 laser-assisted endoscopic cordectomies in our department between 1998 and 2012. The data of the performed procedures according to each type of cordectomy are reported in Table 1 . Fifty-eight patients (23.1%) had more than 1 cordectomy during this period, all of whom had 2 procedures, with the exception of 1, who underwent 4. The cordectomies were classified using the revised terminology proposed in 2007 by the ELS. The revision includes a new endoscopic cordectomy (type VI) for cancers of the anterior commissure, extended to one or both of the vocal folds, without infiltration of the thyroid cartilage.
| Type of Cordectomy | No. of Procedures (Total = 311) (%) | No. of Patients (Total = 251) (%) |
|---|---|---|
| I | 138 (44.4) | 64 (25.5) |
| II | 42 (13.5) | 21 (8.4) |
| III | 42 (13.5) | 32 (12.7) |
| IV | 27 (8.7) | 21 (8.4) |
| V | 55 (17.7) | 49 (19.5) |
| VI | 7 (2.3) | 6 (2.4) |
| Combination | — | 58 (23.1) |
All patients underwent speech therapy after establishment of the scarring process to the operated cord (ie, full development of the neocord). Total or near-total voice recovery was almost always the rule after subepithelial (type I) or subligamental (type II) cordectomies. Supraglottic contraction, although often observed after transmuscular (type III) cordectomy, did respond well to voice rehabilitation, assuming no anterior synechiae were present as well. More extended cordectomy rendered the ipsilateral cord nonfunctional, and voice compensation was obtained from the contralateral healthy cord or the false (ventricular) folds.
Fourteen patients (5.6%) self-assessed their postoperative voice quality as insufficient, complaining of persistent dysphonia and breathiness. There were 12 men and 2 women (9 with T1 cancer and 5 with T2), with a mean age of 53.7 years (range 25–82 years) who underwent a total or extended total (13 patients) cordectomy. One patient with an anterior commissure cancer extending up to the anterior third of both cords underwent a type VI cordectomy. A type V cordectomy was performed on the 5 patients with T2 cancer as well as 3 others with T1b disease.
In addition, 10 patients developed anterior synechiae after total and extended total cordectomy or type VI cordectomy.
Voice Assessment Tools
Voice assessment was performed preoperatively and at regular intervals according to the recommendations of the Committee on Phoniatrics of the ELS. We obtained complete preoperative and postoperative data on 13 of the 14 patients who underwent medialization thyroplasty and all patients who had surgery for anterior synechiae.
Self-evaluation of voice by our patients included the Voice Handicap Index (VHI) questionnaire, which includes the physical, functional and emotional impact of the voice disorder and consists of 30 questions, each rated from 0 to 4, in increasing order of the severity of symptoms. Perceptual voice quality was evaluated with the GRBAS (Grade Roughness Breathiness Asthenia Strain) scale by Hirano. G (overall grade) and R (roughness) (for anterior synechiae) were singled out and rated by a speech therapist with experience in voice assessment.
Aerodynamic measurements included maximum phonation time (MPT; normal range 20–25 seconds) and the phonation quotient (PQ; mL/s) (ie, the quotient obtained by dividing vital capacity with the MPT). We used the best score from 3 successive attempts of the sound “a” for the MPT at a comfortable loudness level.
Maximum fundamental frequency (Fo-high, Hz), as well as lower intensity (I-low, dB) were also calculated in medialization thyroplasty cases and the frequency range (FR, Hz) and fundamental frequency (F0) were analyzed in anterior synechiae surgery. Voice analysis was performed using the Multi Dimensional Voice Program (MDVP) (Kay Elemetrics, Lincoln Park, NJ; KayPENTAX).
Medialization Thyroplasty
Medialization thyroplasty is performed at least 6 months after cordectomy. This is considered the minimum safe period before attempted voice restoration allowing for complete healing of the larynx after laser microsurgery, formation of the neocord, assurance of no residual or recurrent disease, and voice rehabilitation accomplished with adequate voice therapy alone. The procedure is performed under general anesthesia using a laryngeal mask airway (LMA). Transnasal flexible videoendoscopy is carried out to evaluate the degree of glottic gap reduction, and this is feasible through a small valve in the joint that connects the LMA to the ventilation tube. We can assess surgical progress and completion of the thyroplasty by observing the video image captured by the camera attached to the scope without hampering the patient’s ventilation.
The landmarks for creating the window in the thyroid cartilage have been slightly modified according to the different implants used over the period that the procedure has been performed. Meticulous care is taken in dissecting the inner wall of the thyroid cartilage from the fibrous neocord, ensuring close contact with the cartilage at all times, especially when the inner perichondrium was unidentifiable. Furthermore, the dissection has to be extensive enough to facilitate insertion of the implant without fibrous tissue resistance or tear. The technical difficulty of this dissection distinguishes it from medialization procedures for cord immobility, which are easier and therefore more amenable to be performed under local anesthesia ( Figs. 1 and 2 ).




