Purpose
To assess the impact of visual impairment and blindness on the incident use of community support services in the Blue Mountains Eye Study.
Design
Population-based cohort.
Methods
Of 3654 baseline participants (1992-1994), 2334, 1952, and 1149 were re-examined after 5, 10, and 15 years, respectively. Incident visual impairment was defined as subsequent development of visual impairment (visual acuity <20/40) in the better eye of subjects with best-corrected visual acuity ≥20/40 at baseline. Community support service use included regular use of Meals on Wheels, Home Care, or community nurse services. Informal support included assistance from family or friends. Discrete logistic regression models with time-dependent study and outcome variables were used to assess associations between visual impairment and subsequent use of support, adjusted for potential confounders.
Results
Among participants with bilateral visual impairment at baseline, incident use of community services over 5-15 years was 41.7% compared to 19.4% in those without visual impairment at baseline (odds ratio, 1.39; 95% confidence interval, 0.54-3.60). Persons with incident bilateral visual impairment were more likely to subsequently need community support (odds ratio, 3.32; confidence interval 1.96-5.59) in 5 years, compared to persons without visual impairment during the entire follow-up period. Baseline older age, walking disability, receiving pension, and having 2+ hospital admissions within 12 months were also significantly associated with incident use of support services.
Conclusions
Development of bilateral visual impairment in this cohort was associated with greater likelihood of subsequent use of community or informal support services in 5 years, independent of physical comorbidities.
Visual impairment affects between 2% and 27% of the population, while blindness affects up to 2% of people worldwide and is more frequent in older persons. Visual impairment has previously been found to impact negatively on emotional well-being, physical functioning, and independent living. Visual impairment has also consistently been found to be associated with depression, reduced quality of life, premature nursing home placement, and an increased risk of death in a number of population-based studies among older persons.
Government-funded community support services such as the Home and Community Care program in Australia and the Home and Community-Based Services in the United States are designed to assist older people with disabilities living at home. These programs support and preserve these older people’s ability to live independently, maintain their quality of life, and minimize the number of people being admitted to long-term residential care. Some of the services provided under the Home and Community Care program include Home Care (personal care, domestic assistance, home maintenance), nursing care, meal delivery (Meals on Wheels), and transport. This is becoming increasingly important given the aging population.
Previously documented significant associations between the presence of visual impairment and the use of community support services have principally been observed in cross-sectional studies. There has been no evidence from longitudinal data supporting such associations. In this report, we aimed to determine the impact of visual impairment (including its severity and duration) on the subsequent use of community support services over a period of 15 years in a population-based cohort of older Australians, the Blue Mountains Eye Study (BMES).
Methods
Study Population
The BMES is a population-based study of vision and common eye diseases in a suburban Australian population aged 49+ years, residing in the Blue Mountains area, west of Sydney. All baseline and follow-up visits of the BMES were approved by the Human Research Ethics Committees of the University of Sydney and the Western Sydney Area Health Service, and were conducted in adherence to the tenets of the Declaration of Helsinki. Signed informed consent was obtained from all participants at each examination visit.
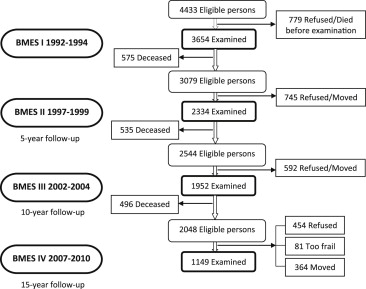
Detailed methods of the baseline survey were reported previously. In summary, at baseline (1992-1994), we recruited and examined 3654 participants. Surviving baseline participants were invited to participate in 5-, 10-, and 15-year follow-up examinations. Of these, 2334 returned after 5 years (75.8% of survivors), 1952 after 10 years (76.7% of survivors), and 1149 after 15 years (56.1% of survivors). Of the 2544 eligible participants between the 10- and 15-year visits, 364 had moved, 81 were admitted to a nursing home and were too frail to participate, 454 refused re-examination, and 496 had died ( Figure ).
Measures
Best-corrected visual acuity (VA) was measured after subjective refraction, using a logarithm of the minimal angle of resolution (logMAR) chart and Early Treatment Diabetic Retinopathy Study (ETDRS) methods at each examination. Visual impairment was defined as VA <20/40 (39 letters or less read) and blindness (severe visual impairment) as VA <20/200 (4 letters or less read). An eye was considered at risk of developing any visual impairment if VA was 20/40 or better at baseline, or at risk of developing severe visual impairment if VA was 20/200 or better at baseline. Incident bilateral visual impairment was defined as the development of visual impairment in 1 or both eyes (the better eye of the two) when at least 1 eye was at risk of developing visual impairment at baseline. The severity of bilateral visual impairment was defined according to VA in the better eye at the latest follow-up visit. Incident unilateral visual impairment was defined as the development of visual impairment in 1 eye when both eyes were at risk of developing visual impairment at baseline. Severity of unilateral visual impairment was defined according to the VA level in the worse eye at the latest follow-up visit. Incident any visual impairment was defined as having either bilateral or unilateral visual impairment at any follow-up visit among subjects who did not have visual impairment in either eye at baseline.
Participants were asked the following questions to determine the use of community and informal support services:
- •
Do you get regular help from Meals on Wheels?
- •
Do you get regular home visits from a community nurse?
- •
Do you get regular visits from Home Care?
- •
Who usually cleans your house?
- •
Who usually does your shopping?
- •
Are you able to go out alone?
The use of community support services (formal support services) was defined as the regular use of 1 or more of the 3 services: Meals on Wheels, Home Care, or regular home visits by a community nurse. The use of informal support was defined as receiving assistance from either family members or friends for house cleaning or shopping. Persons using community support services and those using informal support were mutually excluded from the other category. The ability to go out alone was assessed separately. Incidence of the use of these support services was defined as occurring in participants who did not report using such services in the previous examination but did so at a later follow-up visit.
A comprehensive interviewer-administered questionnaire was conducted detailing sociodemographic characteristics, past history of angina, acute myocardial infarct, stroke, arthritis, hypertension, diabetes, the presence of a walking disability (the use of a cane, crutches, walking frame, or wheelchair), and any hospital admissions (at least overnight) in the 12-month period prior to each visit.
Statistical Analysis
SAS 9.2 software (SAS Institute, Cary, North Carolina, USA) was used for statistical analyses. Discrete logistic regression models (PROC PHREG) with time-dependent study (visual impairment) and outcome (formal or informal support use) variables were used to assess associations between visual impairment and subsequent use of support services. Persons with incident visual impairment detected at the 5- and 10-year follow-up visits were assessed for subsequent uptake of support services at the next follow-up visit with a 5-year interval.
Logistic regression models (PROC LOGISTIC) were used to assess the associations between incident visual impairment detected at the 5-year follow-up and subsequent uptake of support services after 10 years (at the 15-year follow-up). All reported longitudinal associations were adjusted for baseline age and sex. These associations were also adjusted for the presence of a walking disability, home ownership, living arrangements, holding a pension, self-rated health, having ≥2 comorbidities (angina, acute myocardial infarct, stroke, arthritis, hypertension, and/or diabetes) at the time when visual impairment was detected, and having hospital admissions in the 12-month period prior to the visit when visual impairment was detected. Odds ratios (OR) and 95% confidence intervals (CI) are presented.
Results
Incidence of Taking Up Formal and Informal Support Services in the Blue Mountains Eye Study Cohort
Of 3022 participants not already using formal support services at baseline, the incidence of new community support service use over the 5- to 15-year period was 12.8%. Of 2239 participants not already using informal support at baseline, the incidence of new reliance on support from family members and friends over the 5- to 15-year period was 53.6%. Older persons were more likely to use any support service regardless of visual impairment status. Overall, the cumulative incidence of reporting inability to go out alone over the 5- to 15-year period was 6.9% (252/3654).
Baseline Visual Impairment and Subsequent Use of Support Services
Of 3654 participants at baseline, 131 (4%) were found to have bilateral visual impairment at baseline. Among persons with bilateral visual impairment who had not used support services at baseline, the incidence of new use of community support services over the 5- to 15-year period was 41.7% (10/24), compared to 19.4% (456/2350) in those without visual impairment at baseline (adjusted OR 1.39, 95% CI 0.54-3.60). Among persons with bilateral visual impairment who did not rely on informal support at baseline, the incidence of new use of informal support over the 5- to 15-year period was 61.9% (13/21) in persons with bilateral visual impairment compared to 31.6% (504/1594) in those without visual impairment at baseline (adjusted OR 2.96, 95% CI 1.16-7.59). However, the new use of formal or informal support services was not significantly associated with unilateral visual impairment, any visual impairment, or any blindness (data not shown).
Incident Visual Impairment and Subsequent Use of Support Services
Of the 3523 persons without visual impairment at baseline, 73 developed bilateral visual impairment and 294 developed unilateral visual impairment at any follow-up visit (after 5, 10, or 15 years). Because of the small number of persons with incident bilateral blindness at follow-up visits, bilateral and unilateral blindness were grouped together as any blindness, and occurred in 69 persons over the 15-year period. Table 1 shows baseline characteristics of persons with incident unilateral and bilateral visual impairment detected at any follow-up visit and persons without visual impairment over the entire follow-up period. Persons with any incident visual impairment were more likely to be older, to receive a pension, to live alone, to have a walking disability, to have 2+ chronic conditions at baseline, and also to have had 2+ hospital admissions in the 12-month period prior to the baseline examination.
| Characteristic | No Visual Impairment (%) N = 3179 | Unilateral Visual Impairment (%) N = 328 | Adjusted P Value a | Bilateral Visual Impairment (%) N = 131 | Adjusted P Value a |
|---|---|---|---|---|---|
| Age at baseline (y) ± SD | 64.8 ± 9.0 | 73.7 ± 9.4 | <.01 | 80.8 ± 9.1 | <.01 |
| Male | 43.7 | 44.2 | .87 | 29.8 | <.01 |
| Home ownership | 89.1 | 86.6 | .18 | 82.4 | .02 |
| Receiving pension | 55.1 | 80.9 | <.01 | 89.8 | <.01 |
| Living alone | 25.8 | 36.1 | <.01 | 47.3 | <.01 |
| Walking disability | 5.3 | 15.6 | <.01 | 33.9 | <.01 |
| Chronic conditions (≥2) | 16.3 | 25.6 | <.01 | 30.0 | <.01 |
| Hospital admissions (≥2) b | 21.3 | 30.5 | <.01 | 38.2 | <.01 |
a Adjusted for age, sex, home ownership, pension, living status, walking disability, chronic conditions (diabetes, hypertension, arthritis, history of stroke, or heart disease), and hospital admissions.
Of 442 persons who became new (incident) regular users of community support services over the follow-up period, bilateral visual impairment was present in 5.7% (25). Of 1303 persons who became newly reliant on informal support over the follow-up period, bilateral visual impairment was present in 2.4% (31). These proportions compare to 1.3% (14/3148) and 1.4% (42/2880), among those who did not use any formal or informal support, respectively.
Of those with incident bilateral visual impairment, 46.0% (34/74) became new regular users of community support services and 25.9% (7/27) became reliant on informal support. These compare to 9.1% (192/2114) and 29.2% (365/1249) for formal and informal support, respectively, among subjects who did not have any visual impairment over the follow-up period. Persons with incident bilateral (OR 3.32, 95% CI 1.96-5.59) or unilateral (OR 1.77, 95% CI 1.21-2.60) visual impairment during the follow-up period were subsequently more likely to become regular users of community support services within 5 years, compared to people without any visual impairment over the entire follow-up period, after adjustment for age, sex, home ownership, and whether they lived alone, received a pension, had a walking disability, self-rated health, had a hospital admission in the last 12 months, or had 2 or more comorbidities (diabetes, hypertension, arthritis, history of stroke, or heart disease). However, those with incident visual impairment were not significantly more likely to rely on family or friends for informal help in daily tasks within 5 years (OR 1.79, 95% CI 0.70-4.55 for bilateral and OR 1.60, 95% CI 0.92-2.80 for unilateral incident visual impairment). Incidence of any (bilateral or unilateral) blindness was significantly associated with an increased risk of subsequently taking up community support services (OR 2.68, 95% CI 1.48-4.87) and informal support (OR 2.46, 95% CI 0.97-6.27) within 5 years ( Table 2 ).
| Support Service | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Community | Informal | Community or Informal | ||||||||||
| N (%) | OR a | 95% CI | P Value | N (%) | OR a | 95% CI | P Value | N (%) | OR a | 95% CI | P Value | |
| Visual impairment | ||||||||||||
| Bilateral | 73 (46.0) | 3.32 | 1.96-5.59 | <.01 | 27 (25.9) | 1.79 | 0.70-4.55 | .22 | 50 (60.0) | 3.10 | 1.67-5.78 | <.01 |
| Unilateral | 194 (25.8) | 1.77 | 1.21-2.60 | <.01 | 97 (21.7) | 1.60 | 0.92-2.80 | .10 | 133 (42.9) | 1.92 | 1.30-2.83 | <.01 |
| Any (bilateral or unilateral) | 228 (32.5) | 2.39 | 1.70-3.35 | <.01 | 105 (25.7) | 1.78 | 1.07-2.97 | .03 | 158 (50.6) | 2.35 | 1.64-3.37 | <.01 |
| Blindness | ||||||||||||
| Any (bilateral or unilateral) | 59 (39.0) | 2.68 | 1.48-4.87 | <.01 | 23 (34.8) | 2.46 | 0.97-6.27 | .06 | 41 (63.4) | 3.71 | 1.88-7.31 | <.01 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


