Purpose
To evaluate the changes in vision-related quality of life in patients with lacrimal passage obstructions undergoing silicone tube intubations.
Design
Prospective, consecutive, comparative, interventional case series.
Methods
Forty-five patients with the chief complaint of epiphora diagnosed with complete and unilateral lacrimal passage obstructions were enrolled. Exclusion criteria included history of congenital nasolacrimal stenosis; lacrimal passage obstructions resulting from trauma, tumor, or chemotherapy; previous lacrimal passage surgery; and partial and functional nasolacrimal duct obstructions. Silicone tube intubation using a Nunchaku-style tube was performed under direct visualization with dacryoendoscope in all patients. Operations were considered as successful when the irrigating fluid could pass through the lacrimal passage and the disappearance of dye was observed in dye disappearance test and the patients’ epiphora symptoms improved 3 months postoperatively. The 25-item National Eye Institute Visual Function Questionnaire (NEI VFQ-25) was self-administered in all patients preoperatively and 3 months postoperatively. Patients’ preoperative and 3-months-postoperative NEI VFQ-25 scores were compared.
Results
Operations were successful in 40 patients (89%). Fully completed questionnaires were received from 32 patients (80%). Silicone tube intubation using a Nunchaku-style tube was associated with a significant improvement of the NEI VFQ-25 composite score ( P = .0001), ocular pain score ( P < .0001), and mental health score ( P = .0003).
Conclusion
Relief of epiphora by silicone tube intubation using a Nunchaku-style tube treatment significantly improved the vision-related quality of life in patients with lacrimal passage obstructions.
Lacrimal passage obstructions are commonly encountered in ophthalmic practice. Epiphora is the main complaint of patients with lacrimal passage obstructions; patients feel discomfort or annoyance at a constantly bothersome level that negatively affects their vision-related quality of life (QOL). There have been increasing efforts recently to assess the impact of ophthalmic disease on patients’ QOL. The effect of lacrimal passage obstruction treatment on improvement in patients’ QOL should be evaluated. External dacryocystorhinostomy (external-DCR) is the current mainstay treatment for lacrimal passage obstructions. However, patients often do not wish to undergo external-DCR because it is invasive and involves skin incision, bone resection, and nasal packing. Kurihashi has developed direct silicone tube intubation using a Nunchaku-style tube; silicone tubes have been used for years in Japan. Inatani has reported that silicone tube intubation using a Nunchaku-style tube is a less invasive treatment for lacrimal passage obstructions than external-DCR and the success rate of silicone tube intubation using a Nunchaku-style tube for complete lacrimal obstructions is 72.2%. Moreover, we can intubate silicone tubes under direct visualization using a dacryoendoscope.
The purpose of this study was to evaluate the changes in vision-related QOL in patients with lacrimal passage obstructions undergoing silicone tube intubation using a Nunchaku-style tube. We used the 25-item National Eye Institute Visual Function Questionnaire (NEI VFQ-25) to compare patients’ preoperative QOL with their 3-months-postoperative QOL.
Methods
Selection of Patients
Patients with epiphora who presented consecutively to Jikei Aoto Hospital Department of Ophthalmology from April 1, 2009 to March 31, 2010 were recruited in this prospective study. Patients were diagnosed as having unilateral lacrimal passage obstructions based on the following examinations: 1) Probing: A Bowman probe was advanced into the canaliculus. If an obstruction was encountered, measurement of the distance from the forceps to the end of the probe gave information about the location of the obstruction. 2) Dye disappearance test: A moist fluorescein strip was applied to the lower conjunctiva, and the tear lake over the punctum was examined 5 minutes later with a cobalt blue filtered light. The diagnosis of lacrimal passage obstruction was based on the presence of residual dye over the lacrimal punctum. 3) Lacrimal irrigation: We irrigated the lacrimal passage through the upper and lower puncta with sterile physiological saline. If the irrigating fluid could not pass through the patient’s lacrimal passage or if there was no flow of fluid into the posterior pharynx, the patient was diagnosed with complete lacrimal passage obstructions. 4) Imaging: Computed tomography was used to diagnose sinusitis and lacrimal passage obstructions attributable to tumor. Exclusion criteria were: presence of congenital nasolacrimal stenosis; lacrimal passage obstructions attributable to trauma, tumor, or chemotherapy; or previous lacrimal passage surgery. Partial and functional lacrimal duct obstructions were excluded in this study. After receiving informed consent about treatment of lacrimal passage obstructions and exclusion criteria, 45 patients chose the silicone tube intubation using a Nunchaku-style tube treatment and were enrolled in this study. All examinations and operations were performed by a single surgeon (S.G.).
Surgical Technique
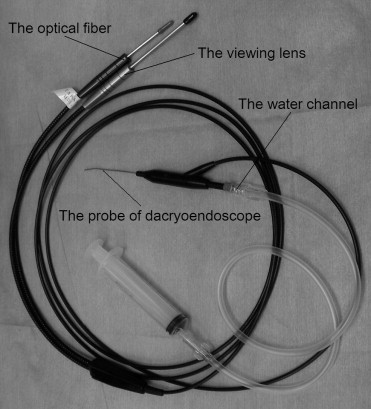
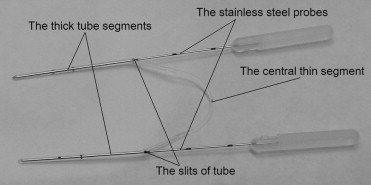
After anesthetizing the upper and lower puncta and performing an infratrochlear nerve block with 2% lidocaine, both puncta were enlarged using a punctal dilator. We inserted the probe of the dacryoendoscope (FT-2000E; Fibertech Co, Tokyo, Japan; Figure 1 ) through the upper canaliculus. Upon reaching the lacrimal sac, the probe was thrust forward into the nasolacrimal duct to relieve the obstructions under direct visualization. During this procedure, saline was injected through the water channel to remove hemorrhage and to create space. After relieving the obstruction by the dacryoendoscopy probe, one end of the Nunchaku-style tube (Kaneka Co, Tokyo, Japan; Figure 2 ) was inserted into the upper puncta. When it reached the medial wall of the nasolacrimal sac through the canaliculus, it was turned vertically, and then inserted into the nasolacrimal duct and nasal cavity. The stainless steel probe inside the tube was then pulled out. After insertion of the tube into the upper puncta, the other side of the Nunchaku-style tube was inserted through the lower puncta in the same way. Finally, we confirmed that the silicone tube had been intubated correctly using the dacryoendoscope. The colors of apical parts of the Nunchaku-style tube are different—either blue or transparent; hence, we could recognize the appropriate intubation from the upper or lower puncta.
After intubation using the Nunchaku-style tube, all patients were treated with topical antibiotic and steroid eye drops, and the eyes were irrigated regularly until the tube was removed 2 months later. Patients were asked to quantify their symptoms as follows: (A), epiphora is worse; (B), epiphora is the same; (C), epiphora is decreased from preoperative; (D), no symptom of epiphora. Patients self-reported as A or B were defined “no improvement,” C or D as “improvement.” The operation was considered successful if the irrigating fluid passed through the lacrimal passage, if the disappearance of dye was observed over the lacrimal punctum in a dye disappearance test, and if the patient’s symptoms of epiphora improved.
NEI VFQ-25
NEI VFQ-25 was self-administered by 45 patients, both preoperatively and 3 months postoperatively. In this study, the Japanese version of the NEI VFQ-25, which had been modified to suit the Japanese culture and lifestyle, was used. This modified NEI VFQ-25 has been assessed for its reliability and validity, and has been proven to measure vision-related QOL accurately in Japanese individuals. NEI VFQ-25 comprises 12 vision-targeted scales: general health, general vision, ocular pain, near activities, distance activities, social functioning, mental health, role difficulties, dependency, driving, color vision, and peripheral vision. Each scale consists of a minimum of 1 and a maximum of 4 items. Subscales were scored on a scale of 0 (worst) to 100 points (best). Scores were calculated using the recommendations of the developers of the questionnaire and according to published guidelines for NEI VFQ-25. The mean scores and standard deviation (SD) were calculated for each subscale, and the composite score was calculated by averaging the scores of 11 subscales; the general health subscale was excluded.
Statistical Analysis
The Wilcoxon signed rank test was used to compare preoperative and postoperative results. Comparisons were considered as statistically significant if the P value was less than .05. The analyses were carried out using JMP version 8 (SAS Inc, Cary, North Carolina, USA).
Results
Out of the 45 patients, the operations were successful in 40 (89%). Operations were unsuccessful in 5 cases: in 1 case we could not intubate the silicone tube correctly because of presence of a solid adhesion in the nasolacrimal duct, in 2 cases the irrigating fluid could not pass through the patient’s lacrimal passage, and 2 cases showed no improvement of the patient’s symptoms of epiphora. Among the 40 patients with successful operations, fully completed questionnaires were received from 32 patients (80%). Two patients with incomplete questionnaires were excluded and 6 patients’ questionnaire forms could not be received. The data from these 32 patients were collected and used for the analysis. The study population consisted of 7 male and 25 female subjects and mean (SD, range) age was 71 (11, 40-89).The mean (SD, range) duration of silicone tube insertion was 69 (7, 52-81) days. Obstruction sites were observed using dacryoendoscope: canaliculus, 12 (38%); nasolacrimal duct, 17 (53%); canaliculus and nasolacrimal duct, 3 (9%).
The Table shows the preoperative and postoperative mean subscale scores and composite score from NEI VFQ-25. Successful silicone tube intubation using a Nunchaku-style tube improved the composite score ( P = .0001), ocular pain score ( P < .0001), and mental health score ( P = .0003). In particular, the score for ocular pain was 46.5 (SD, 22.3) preoperatively and 84.8 (SD, 13.7) postoperatively, indicating a considerable improvement with intubation.



