(1)
Alo Eye Care, Kolkata, India
Keywords
Eyelid reconstructionLid margin defectsLateral canthotomyRotational flapSwitch flapTarso conjunctival flapMyocutaneous flapCutler-Beard (Bridge) flap12.1 Small Central Eyelid Margin Defects (Direct Closure)
12.1.1 Indications
Defects involving up to 30 % of the upper eyelid in young patients and up to 45 % in elderly patients
Cases in which the two cut edges can be brought together without creating undue tension
12.1.2 Technique
The surgeon must ensure that all margins are tumor-free.
If the excised tissue defect does not extend beyond the superior edge of the tarsal plate, the cuts are extended across the superior margin of the tarsal Plate.
A triangle is cut superior to the defect. The base of the triangle should start above the superior extent of the tarsal plate. (This is done to prevent notching and an irregular contour of the newly formed lid margin.)
The wound should look like a pentagon.
The orbicularis muscle is separated from the tarsal plate at the edges. This allows better placement of sutures.
The lid defect is repaired in two layers, as described in Chap. 11.
12.1.3 Other Variations/Options
Try pulling the cut ends of the lid defect towards each other with two tooth forceps, and see if the cut margin can be apposed without undue tension. This will provide a good estimate of the feasibility of this approach.
If the surgeon anticipates undue tension on the suture line, a lateral canthotomy should be planned. The details of this procedure are discussed in the next section.
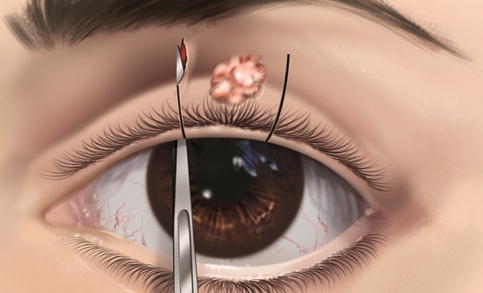
Fig. 12.1
Direct closure. An incision is made along the marked lines, about 3 mm beyond the visible extent of the lesion
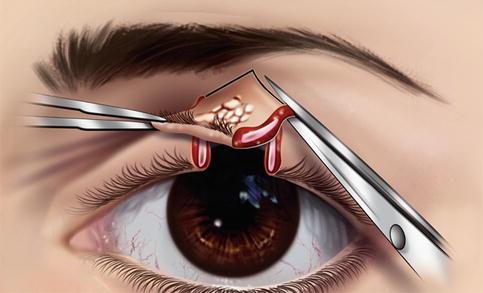
Fig. 12.2
Direct closure. A triangle superior to the defect is excised
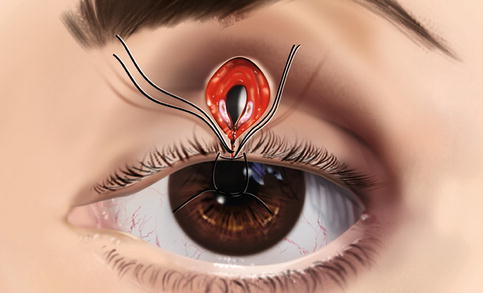
Fig. 12.3
Direct closure. Interrupted sutures applied through the gray line and tarsus
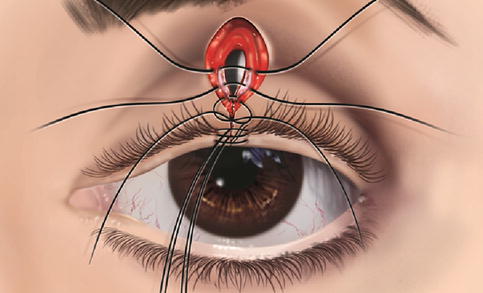
Fig. 12.4
Direct closure. More interrupted sutures are applied

Fig. 12.5
Direct closure. Skin suturing is complete

Fig. 12.6
Direct closure. A small acquired hemangioma in the lid margin

Fig. 12.7
Direct closure. The tumor has been excised with the full-thickness eyelid defect

Fig. 12.8
Direct closure. Six weeks after direct lid closure
12.2 Small to Medium Central Eyelid Margin Defects That Cannot Be Closed by Direct Apposition (Lateral Canthotomy)
12.2.1 Indications
Indications are similar to those for direct closure but include cases in which there seems to be undue stress on the apposition line.
12.2.2 Technique
If undue tension on the suture line is anticipated, a lateral canthotomy should be planned.
An artery forceps is applied over the lateral canthus horizontally.
The clamp is crushed so that on removal, the serrated indentations of the arterial forceps are visible over the lateral canthus.
Westcott scissors are applied through the crushed tissue (curved slightly upward to cut the upper limb of the lateral canthal ligament). Cutting of the lateral canthal ligament can be felt as a sensation of something giving way. This may be confirmed by the sudden increase in mobility of the lower lid.
A skin incision is made over the lateral canthus, angled slightly inferior in case a rotational flap is necessary.
Reapproximation of the defect is attempted with a pair of skin hooks; they now should be able to be apposed easily.
The lid defect is sutured in two layers, as discussed earlier.
A few interrupted sutures may be applied between the conjunctiva and the skin at the lateral canthus, which will give a good contour to the lateral angle.
12.2.3 Other Variations/Options
The lateral canthus may be left to granulate by itself.
If undue tension still exists on the lid margin, the skin must be mobilized from the inferolateral aspect of the orbit by a rotational flap.
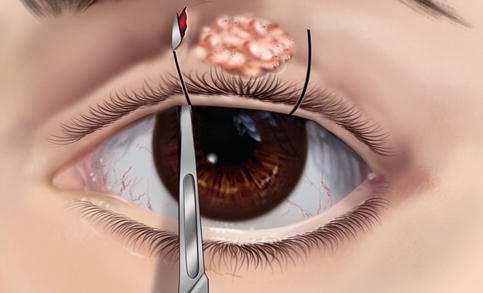
Fig. 12.9
Lateral canthotomy. Vertical incisions being made 3 mm beyond the visible tumor margin
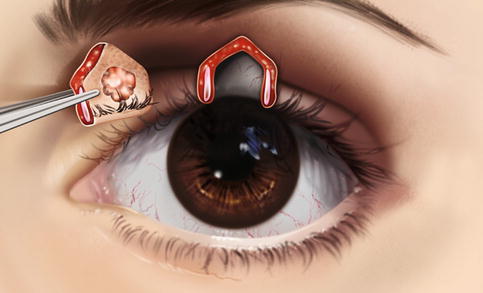
Fig. 12.10
Lateral canthotomy. The tumor, along with surrounding healthy lid tissue, has been excised
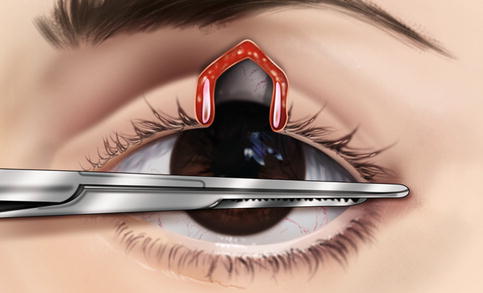
Fig. 12.11
Lateral canthotomy. The lateral canthus is crushed with artery forceps

Fig. 12.12
Lateral canthotomy. The lateral canthal ligament is cut
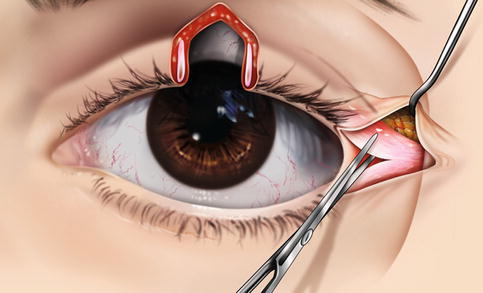
Fig. 12.13
Lateral canthotomy. The upper crush of the lateral canthal ligament is cut and released
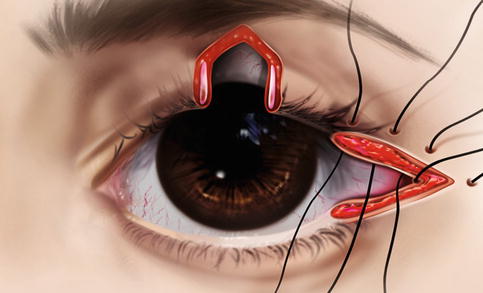
Fig. 12.14
Lateral canthotomy. Interrupted sutures are applied to form a V at the canthal angle
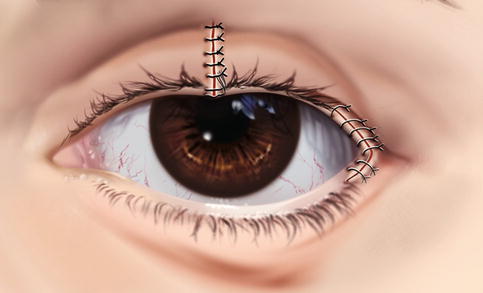
Fig. 12.15
Lateral canthotomy. Mobilization helps approximate the cut ends of the lid. It is closed as is done in direct closure
12.3 Medium to Large Upper Eyelid Defects (Rotational Flap)
12.3.1 Indications
Full-thickness lid margin defects in which the lid cannot be apposed despite lateral canthotomy
Defects involving 50–60 % of the upper lid, situated in the central portion, where the cut end of the tarsal plate is available on both sides.
12.3.2 Technique
A semicircular skin incision is marked from the lateral angle. The incision line is arched downward to cross the inferolateral periorbital skin.
Lateral cantholysis is done, as described earlier.
A myocutaneous flap is mobilized along the skin marking. The skin incision is not done all at once; mobilization and undermining are performed in segments. An attempt then is made to pull the skin flap to see whether the primary central tissue defect can be apposed. If not, the skin incision is extended slightly and the flap is mobilized a little more. (This will prevent an unwanted large semicircular flap.)
The underlying conjunctiva is mobilized along with the skin flap, as this also must be brought to the apposition line.
The lid margin defect is apposed as in direct closure (described earlier).
The lateral angle is formed by passing a few absorbable 6/0 Vicryl interrupted (or interlocking continuous) sutures between the skin and underlying conjunctiva at the lateral canthus.
The semicircular skin incision then is closed over the lateral aspect of the periorbital region with 6/0 nonabsorbable Nylon or silk sutures.
The skin sutures are removed at 5–7 days. The gray line suture is left in place and may be removed in 10–14 days.
12.3.3 Other Variations/Options
While the tarsal edges are sutured, the patient is asked to open his or her eyes so that the surgeon can check for any ptosis caused by an insufficient upper lid. If ptosis is present, the lateral canthal tendon is weakened further by relaxation and better mobilization of the advancement flap until the patient can open his or her eye without residual ptosis.
If after the tarsal edges are approximated there appears to be a wider palpebral fissure on the operated side, the canthal tendon is tightened until the upper lid height is equal to that of the opposite side.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


