8 Core Messages • Papillary thyroid cancer (PTC) variants that are more aggressive than typical papillary cancer include tall-cell and diffuse sclerosing variants. • Follicular variant of PTC is similar in prognosis to PTC overall. • Cribriform-morular variant may occur in association with familial adenomatous polyposis and requires adenomatous polyposis coli mutational analysis. • Insular and squamous carcinomas of the thyroid are high-grade lesions with poorer prognosis than typical differentiated thyroid carcinomas. Tall-cell variant (TCV) of papillary thyroid carcinoma (PTC) was initially characterized by Hawk and Hazard in 1976.1 Overall, TCV accounts for approximately 10% of PTCs (Table 8.1). Histologically, TVC is diagnosed by the presence of a papillary tumor whose cells are at least two to three times as high as they are wide.1–3 Other cytologic features associated with this tumor include distinctive intracytoplasmic borders and eosinophilic cytoplasm (Fig. 8.1). As a group, patients with TCV have both a higher recurrence rate and overall mortality rate than do patients with classical papillary thyroid cancer.4,5 This finding was initially attributed to the fact that these patients tended to be older and more frequently presented with extrathyroidal extension.5 Ghossein et al, however, demonstrated that in their series of patients, patients with TCV without extracapsular extension had a higher nodal metastatic rate than did patients with classical PTC independent of age, gender, and tumor size.6 In their study, 3 of the 47 patients with TCV without extrathyroidal extension developed distant metastasis, while none of the 62 patients with classical PTC presented with distant metastasis. Morris et al retrospectively reviewed 278 patients with TCV and 2522 patients with classical PTC at Memorial Sloan Kettering Cancer Center. As in Ghossein et al’s study, when compared with patients with classical PTC, patients with TCV presented at an older age, had a higher rate of extracapsular extension, and had a worse 5-year disease-specific survival rate. They concluded that when the major prognostic factors for thyroid cancer were controlled for, tall-cell histology alone remained a significant independent prognostic factor for disease-specific death.7 On a molecular level, several studies have shown that TCV tumors have a higher rate of BRAF mutations than do classical PTC tumors.8 Clinical trials are currently under way investigating the use of chemotherapeutic agents targeting BRAF. Currently, there are no studies that have addressed the prognostic implications of cervical lymph node metastasis in patients with TVC. Given the aggressive nature of TVC, a comprehensive surgical approach is reasonable including total thyroidectomy, elective central nodal exploration, and directed dissection followed by radioactive iodine therapy. Table 8.1 PTC Variants with Clinical Correlations
Unusual Tumors of the Thyroid Gland
Variants of Papillary Thyroid Carcinoma
Tall-Cell Variant
PTC Variant | Surgical Treatment | Prognosis Relative to Classical PTC |
Tall-cell | More aggressive—total thyroid and nodal | Worse than PTC |
Diffuse sclerosing | More aggressive—total thyroid and nodal | Worse than PTC |
Cribriform-morular | Intermediate | Variable |
Follicular | As for classical PTC | Equal to PTC |
Columnar cell | Intermediate | Variable |
PTC, papillary thyroid carcinoma.
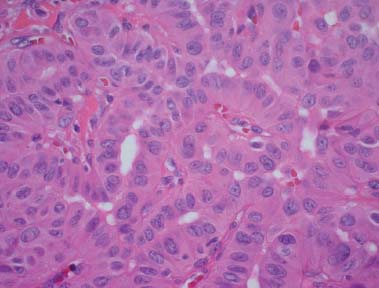
Figure 8.1 Image demonstrating the characteristic features of tall-cell variant of papillary carcinoma. The cells have a tall shape, with the height at least twice the width. The cells also have eosinophilic cytoplasm and distinctive cell borders. Hematoxylin and eosin stain, ×20 original magnification.
Follicular Variant
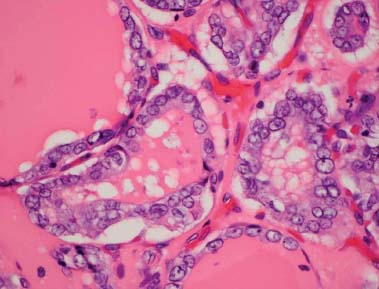
Follicular variant (FV) of papillary thyroid cancer, first described in 1977 by Chen and Rosai, is diagnosed histologically by the formation of follicles lined by cells containing nuclear features of papillary carcinoma (Fig. 8.2).9 In 2010, Lin and Bhattacharyya reported an analysis of the national cancer database in the United States reviewing the prevalence and extent of disease characteristics of FV.10 They found that compared with classical papillary thyroid cancer, age at presentation and sex distribution were similar for FV, the prevalence of lymph node metastasis was lower in FV (14.8 vs. 27.8%), and the mean overall survival of patients with FV was not statistically different from that of patients with classical PTC. These findings have been further supported in other studies.11,12
In 1991, Albores-Saavedra et al reported on an unusual entity, the “macrofollicular variant” of PTC, characterized as a well-differentiated carcinoma with large, follicular architecture with nuclear appearance similar to that of PTC.13 This entity was originally noted to have a low incidence of regional and distant metastasis and an overall good prognosis; however, Cardenas et al reported on two patients with a highly aggressive macrofollicular variant of papillary thyroid cancer.14
Given similar survival outcome between FV and PTC, the current recommendations for the management of FV are the same as that for PTC.
Figure 8.2 Image showing the features of follicular variant of papillary carcinoma. The tumor is growing with a pure follicular architecture and demonstrates the nuclear features of papillary carcinoma. Hematoxylin and eosin stain, ×40 original magnification.
Columnar-Cell Variant
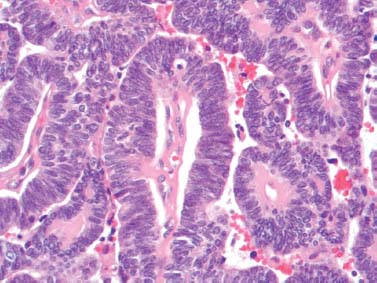
Initially described by Evans in 1986, columnar-cell variant (CCV) of PTC is characterized by tall cells with elongated hyperchromatic pseudostratified nuclei (Fig. 8.3).15 To make the diagnosis, a requirement of at least 30% columnar cells is needed. CCV accounts for 0.15 to 0.2% of all papillary carcinomas.16
CCV is often associated with an uncertain clinical course. Histologically, small size and encapsulation have been associated with a more favorable prognosis, while large size and extrathyroidal extension have been associated with a worse prognosis.17 In an analysis of the literature by Chen et al, there were 48 reported cases, 15 men and 33 women with age ranging from 16 to 50 years. In 20 cases, the tumors were clinically indolent, while in 23 cases, the tumors were aggressive. Indolent tumors tended to be smaller (mean 3.6 cm, median 3.8 cm), while clinically aggressive tumors were larger (mean 6.0 cm, median 6.3 cm).17
Vickery et al reported on 41 cases of CCV, with 27% having extracapsular spread and 50% having cervical metastasis at presentation.18 In this study, with a mean follow-up of 43 months, 33% had locoregional recurrence, 36% developed distant metastasis, and there was a 29% disease-specific mortality rate. The authors concluded that prognosis was poor if the tumor showed extracapsular extension; however, CCV itself did not predict a poor outcome. Chen et al reported similar results in nine patients with CCV.17 The four indolent neoplasms in this study were small (mean 2.1 cm), encapsulated, well circumscribed, and affected younger and predominantly female patients. The five aggressive neoplasms were large (mean 6.7 cm), diffusely infiltrative with extrathyroidal extension, and affected older and predominantly male patients.
Figure 8.3 Image showing the features of columnar-cell variant of papillary carcinoma. The cells show nuclei with condensed, dark chromatin that are pseudostratified. Hematoxylin and eosin stain, ×20 original magnification.
The treatment for CCV, therefore, should be based on clinical and histologic evaluation. Appropriately aggressive therapy, total thyroidectomy, central neck dissection, and adjuvant radioactive iodine should be considered in patients demonstrating extracapsular extension. External beam radiation may be considered in patients in whom complete surgical resection has not been achieved.
Diffuse Sclerosing Variant
Diffuse sclerosing variant (DSV) of PTC is uncommon. To date, approximately 150 cases have been reported in the literature.18–53 Vickery et al was the first to describe this new variant of PTC in 1985.18 Histologically, DSV is characterized by diffuse involvement of both lobes of the thyroid gland with dense fibrosis, lymphatic infiltrate, multiple foci of squamous metaplastic changes, and numerous psammoma bodies.18
Clinically, patients with DSV tend to be younger than patients with classical papillary thyroid cancer.18–53 The mean age of patients with DSV ranges from 19.5 to 34.7 years. In a 35-year comparative study by Lam and Lo of 15 patients with DSV, the mean age of patients with DSV was 29 versus 46 years for patients with classical PTC.53 Furthermore, compared with patients with classical papillary thyroid cancer, patients with DSV had larger tumors (mean diameter, 3.6 vs. 2.2 cm), had a higher incidence of lymph node metastasis (80 vs. 43%), and frequent disease recurrence.
Because survival data for DSV are derived from case reports and small series, the overall clinical behavior remains controversial.18–54 In the previously mentioned study by Lam and Lo, the 10-year survival rate of patients with classical papillary thyroid cancer was 92% while the 10-year survival rate of patients with DSV was 93%.53 However, in this study, the treatment protocol for patients with DSV was more aggressive. This included initial “radical surgery” followed by radioactive treatment. An active search for suspicious lymph nodes at the initial operation is recommended because of the higher risk of nodal metastasis.
Cribriform-Morular Variant
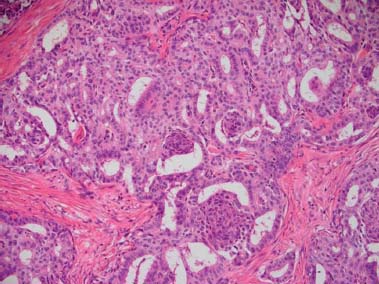
First described by Harach et al in 1994, cribriform-morular variant (CMV) of papillary thyroid cancer is characterized by the papillary growth of tall columnar cells, cribriform pattern, solid and spindle cells, squamoid morules, and peculiar nuclear clearing (Fig. 8.4).55 CMV can be either sporadic or familial. Familial CMV is associated with familial adenomatous polyposis where adenomatous polyposis coli (APC) mutations may play an important role.56–58 Familial CMV is usually multifocal and occurs more often in women.59 Sporadic tumors, on the other hand, usually present as solitary nodules and are not associated with colonic polyps.56,57,60,61 Because of these distinct characteristics, total thyroidectomy is generally recommended for familial CMV while a lobectomy may be considered in the sporadic form. Interestingly, Plail et al reported that because up to 30% of thyroid carcinomas may be diagnosed 4 to 12 years before the development of colonic polyps, colonoscopy and APC gene analysis are recommended in these patients.62
Insular Carcinoma
Insular carcinoma was described by Carcangiu et al in 1984 as the presence of histologically well-defined nests of tumor cells with round, dark, and monomorphic nuclei and scant cytoplasm (see Table 8.2).63 Insular cell carcinomas tend to be large, greater than 4 cm, and often exhibit extracapsular spread. Sywak et al evaluated 213 patients with insular thyroid cancer, reporting a predominance of female patients and mean tumor size of 5.5 cm, with 44% exhibiting extracapsular extension and 51% with clinically apparent cervical metastasis.64 Locoregional recurrence or distant metastasis was seen in 64% with a disease-specific mortality of 32%. The insular variant meets many of the criteria of poorly differentiated carcinoma, and many experts believe that it may be a precursor to anaplastic thyroid carcinoma.65
Figure 8.4 Image demonstrating a cribriform-morular variant of papillary carcinoma. There are papillary formations, cribriform growth, and one morular formation. Hematoxylin and eosin stain, ×10 original magnification.
Table 8.2 Unusual Thyroid Tumors and Their Prognosis
Tumor Type | Key Point | Prognosis |
Cribriform-morular variant | Total if familial, APC mutation testing required | Fair-poor |
Insular carcinoma | High-grade lesion | Poor |
Metastases to the thyroid gland | May be PET+, generally with known history of primary tumor | Poor |
Squamous cell carcinoma of the thyroid | High-grade lesion, rule out nonthyroid squamous lesion and squamoid anaplastic | Poor |
Mucoepidermoid carcinoma (and SMECE) | Solitary lesion arising from ultimobranchial/lateral thyroid anlagen | Poor |
CASTLE | Solitary lesion, arising from ultimobranchial/lateral thyroid anlagen | Fair |
SETTLE | Solitary lesion, thymic differentiation, rule out sarcoma | Good |
PET, positron emission tomography; SMECE, sclerosing mucoepidermoid carcinoma with eosinophilia; CASTLE, carcinoma showing thymic-like differentiation; APC, adenomatous polyposis coli; SETTLE, spindle epithelial tumor with thymic-like differentiation.
Aggressive surgical management, total thyroidectomy, and central neck dissection followed by radioactive iodine or external beam radiation in the setting of incomplete resection is recommended.
Metastases to the Thyroid Gland
It is uncommon for tumors from other organ systems to metastasize to the thyroid gland. The most common tumor to demonstrate metastases to the thyroid is renal cell carcinoma.66–68 Other tumors in the literature that have been reported as metastatic disease appear in isolated case reports and include breast carcinoma, Merkel cell carcinoma, pancreatic adenocarcinoma, lung and colon carcinoma, and other rare tumors.66,69–72
The clinical presentation of metastases to the thyroid gland varies, depending on the site of origin from the tumor. An extensive literature about the radiologic presentation does not exist, but case reports have identified that renal cell carcinoma (RCC) may be positive on positron emission tomography scanning.73 In many of these cases of metastasis to the thyroid gland, the patient will present with a clinical history of the tumor and with widespread metastatic disease. But with RCC in particular, patients may have only a distant history of thveir primary tumor.74,75 Some patients will present with their thyroid lesion as a first manifestation of their primary malignancy.70
Diagnosing metastatic disease preoperatively may be nearly impossible, as fine-needle aspiration cytology will rarely be definitive. There are several case reports of the cytopathologic features of metastatic tumors in thyroid, from which it is clear that metastatic tumors will often mimic primary thyroid tumorson on cytology.70 On occasion, a tumor from another organ may also metastasize to a primary thyroid tumor, such as a follicular adenoma or a papillary carcinoma.66 In this scenario, it becomes even more challenging to make a preoperative diagnosis from the cytologic features.
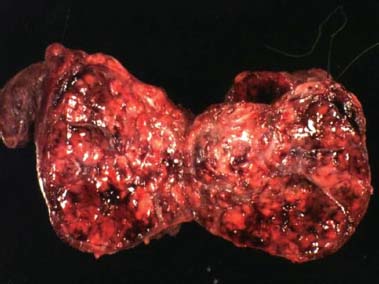
Grossly, these tumors are usually clinical, somewhat nonspecific, and present as mass lesions or diffuse infiltration of the thyroid gland. The exception is metastatic RCC, which almost always has a striking yellow appearance, due to the lipid content within the cytoplasm of the tumor cells (Fig. 8.5).
Histologically, the metastatic tumor may have specific or nonspecific cellular features. Again, RCC is one of the most striking, with characteristic nested growth and an extensive vascular network in the background. In RCC, the metastatic tumor cells often have low-grade, monomorphic nuclei with clear, vacuolated cytoplasm. At the immunohistochemistry level, metastases are invariably negative for thyroglobulin and for thyroid transcription factor 1 (TTF-1) markers.68 Other markers that are associated with the organ of the primary tumor may be used to further subclassify these tumors. For example, metastatic RCC will commonly be positive for vimentin, PAX8, CD10, EMA, and RCC antigen. Some caution is required in using isolated immunohistochemical stains without the panel approach. This can easily be illustrated by the fact that PAX8 also can stain primary thyroid tumors.68
Figure 8.5 A gross image of a metastatic renal cell carcinoma of the thyroid. The tumor has a yellow appearance and has massive hemorrhage, which are characteristic gross features of metastatic renal cell carcinoma.