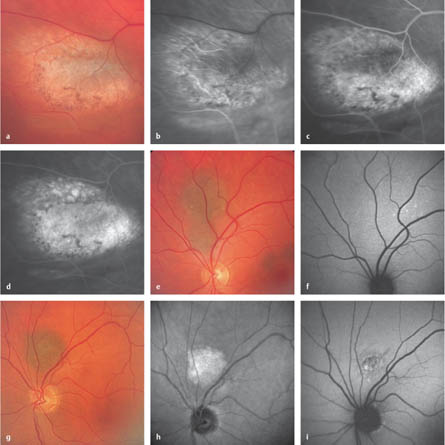
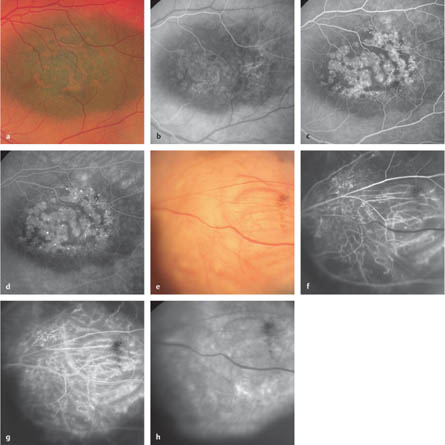
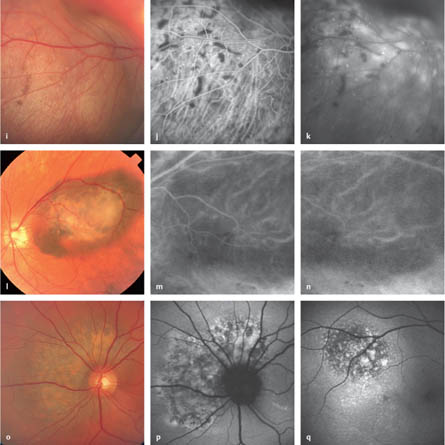
5.1 Choroidal Nevi Parodi MB, Boscia F, Piermarocchi S, et al. Variable outcome of photodynamic therapy for choroidal neovascularization associated with choroidal nevus. Retina 2005;25:438–42. Shields CL, Cater J, Shields JA, Singh AD, Santos MC, Carvalho C. Combination of clinical factors predictive of growth of small choroidal melanocytic tumors. Arch Ophthalmol 2000;118:360–4. Shields JA, Mashayekhi A, Ra S, Shields CL. Pseudomelanomas of the posterior uveal tract: the 2006 Taylor R. Smith Lecture. Retina 2005;25:767–71. Shields CL, Mashayekhi A, Materin MA, et al. Optical coherence tomography of choroidal nevus in 120 patients. Retina 2005;25: 243–52. Singh AD, Kalyani P, Topham A. Estimating the risk of malignant transformation of a choroidal nevus. Ophthalmology 2005;112: 1784–9. Fig. 5.1a–i Choroidal nevi a Color photograph. Amelanotic choroidal nevus with drusen, discrete atrophies, and accumulation of pigment in the overlying retinal pigment epithelium. b Early phase. “Normal” choroidal vessels and slight hyperfluorescence of the nevus are visible. c Arteriovenous phase. There is an increase in the hyperfluorescence, with blockage in the region of the pigment accumulation. d Late phase. There is a further increase in the hyperfluorescence, including the clinically visible drusen. e Color photograph. Choroidal nevi near the fovea and superior to the optic disc. f Fundus autofluorescence. Neither the nevus superior to the optic disc nor the central nevi can be detected. The autofluorescence pattern within the lesions is unremarkable. A few drusen outside are outlined superior to the vascular arcade. g Color photograph. Small choroidal nevi with a few drusen superior to the optic disc. h With infrared imaging, the borders of the nevus are more distinct. i Fundus autofluorescence. In the area of the lesion, spot-like increases in autofluorescence indicate drusen, and some pigment epithelial alterations can be observed. Fig. 5.2a–h Choroidal melanoma a Color photograph. A pigmented flat choroidal melanoma with “orange pigment.” b Early phase. Filling of the tumor vessels under the retinal vessels (“double circulation”). c Arteriovenous phase. Hyperfluorescence on the tumor surface, with dot-like “hot spots” and a geographic blockage in the area of the orange pigment. d Late phase. Further blockage in the area of the orange pigment, and an increase in fluorescence in the hot spots. e Color photograph. Minimally pigmented large choroidal melanoma with visible large and deep tumor vessels. f Early phase. Parallel to the arterial filling phase of the retinal vessels, complex microcirculation patterns within the tumor are seen, as well as large tumor vessels. g Middle phase. Simultaneous depiction of retinal and tumor vessels (“double circulation”). A focal blockage (hypofluorescence) is visible in the region of the tumor surface pigmentation. h Late phase. An area of diffuse deep hyperfluorescence, as well as several “hot spots,” are visible. The large tumor vessels appear hypofluorescent. Edwards WC, Layden WE, Macdonald R Jr. Fluorescein angiography of malignant melanoma of the choroid. Am J Ophthalmol 1969;68:797–808. Hayreh SS. Choroidal melanomata: fluorescence angiographic and histopathological study. Br J Ophthalmol 1970;54:145–60. Krause L, Bechrakis NE, Heinrich S, Kreusel KM, Foerster MH. Indocyanine green angiography and fluorescein angiography of malignant choroidal melanomas following proton beam irradiation. Graefes Arch Clin Exp Ophthalmol 2005:243:545–50. Mueller AJ, Freeman WR, Schaller UC, Kampik A, Folberg R. Complex microcirculation patterns detected by confocal indocyanine green angiography predict time to growth of small choroidal melanocytic tumors: MuSIC Report II. Ophthalmology 2002;109:2207–14. Sallet G, Amoaku WM, Lafaut BA, Brabant P, De Laey JJ. Indocyanine green angiography of choroidal tumors. Graefes Arch Clin Exp Ophthalmol 1995;233:677–89. Fig. 5.2i–q Choroidal melanoma i Color photograph. A moderately pigmented large choroidal melanoma, with orange pigment on the surface. j Middle phase. Geographic blockages in areas with orange pigment and dot-like hot spots. k Late phase. The deep diffuse focal hyperfluorescence in the tumor makes the retinal and tumor vessels appear hypofluores-cent. l Color photograph. Malignant melanoma of the choroid, with orange pigment on the tumor surface. The tumor has variably strong pigmentation. m
Epidemiology, Pathophysiology, and Clinical Presentation
 Nevi of the choroid are the most common type of intraocular benign tumor, with a prevalence of between 11% and 20%.
Nevi of the choroid are the most common type of intraocular benign tumor, with a prevalence of between 11% and 20%.
 Approximately 90% of choroidal nevi can be found posterior to the equator. They are generally first diagnosed after puberty, once the pigment content has increased.
Approximately 90% of choroidal nevi can be found posterior to the equator. They are generally first diagnosed after puberty, once the pigment content has increased.
 The majority of nevi are asymptomatic. Occasionally, however, they can cause functional deficits in the visual field of the overlying retina. In some cases, nevi may show associated serous exudation.
The majority of nevi are asymptomatic. Occasionally, however, they can cause functional deficits in the visual field of the overlying retina. In some cases, nevi may show associated serous exudation.
 Drusen often (in approximately 50% of cases) appear on the surface of the nevi, along with chronic degenerative changes in the retinal pigment epithelium, and occasionally (but rarely) choroidal neovascularizations.
Drusen often (in approximately 50% of cases) appear on the surface of the nevi, along with chronic degenerative changes in the retinal pigment epithelium, and occasionally (but rarely) choroidal neovascularizations.
 A relatively rare variant of choroidal nevus is melanocytoma, which has very dark to black pigmentation. The most common site of presentation of this type of lesion is on the optic nerve head.
A relatively rare variant of choroidal nevus is melanocytoma, which has very dark to black pigmentation. The most common site of presentation of this type of lesion is on the optic nerve head.
Fluorescein Angiography
 There are no specific angiographic patterns in choroidal nevi. Darkly pigmented nevi generally show a hypofluorescence due to a blockage of the choroidal background fluorescence in all phases of angiography.
There are no specific angiographic patterns in choroidal nevi. Darkly pigmented nevi generally show a hypofluorescence due to a blockage of the choroidal background fluorescence in all phases of angiography.
 Associated drusen usually show hyperfluorescence. Atrophy of the retinal pigment epithelium appears as a window defect, and accumulations of pigment cause areas of hypofluorescence. Less pigmented or amelanotic nevi may be completely hyperfluorescent. Generally, no visible angiographic microcirculation can be documented in choroidal nevi.
Associated drusen usually show hyperfluorescence. Atrophy of the retinal pigment epithelium appears as a window defect, and accumulations of pigment cause areas of hypofluorescence. Less pigmented or amelanotic nevi may be completely hyperfluorescent. Generally, no visible angiographic microcirculation can be documented in choroidal nevi.
Fundus Autofluorescence
 On fundus autofluorescence, drusen show increased autofluorescence, whereas the other regions of the nevi may either be undetectable by autofluorescence or show spot-like increased autofluorescence. An existing or regressed exudative reaction may be detectable due to increased autofluorescence, typically below the nevi.
On fundus autofluorescence, drusen show increased autofluorescence, whereas the other regions of the nevi may either be undetectable by autofluorescence or show spot-like increased autofluorescence. An existing or regressed exudative reaction may be detectable due to increased autofluorescence, typically below the nevi.
Diagnosis and Treatment
 Nevi do not require treatment. The importance of recognizing nevi is the differential diagnosis of small uveal melanocytic lesions.
Nevi do not require treatment. The importance of recognizing nevi is the differential diagnosis of small uveal melanocytic lesions.
 Risk factors possibly suggesting growth of a nevus are: tumor width of more than 2.0 mm; juxtapapillary position; symptoms reported by the patient; and the existence of either “orange pigment,” subretinal fluid, or complex microcirculation patterns. Fluorescein angiography or indocyanine green angiography are very useful for examining the latter two risk factors and can therefore be informative for assessing or treating small melanocytic lesions.
Risk factors possibly suggesting growth of a nevus are: tumor width of more than 2.0 mm; juxtapapillary position; symptoms reported by the patient; and the existence of either “orange pigment,” subretinal fluid, or complex microcirculation patterns. Fluorescein angiography or indocyanine green angiography are very useful for examining the latter two risk factors and can therefore be informative for assessing or treating small melanocytic lesions.
 Fundus autofluorescence adds further information for differentiating between small choroidal melanoma and nevi. It is always abnormal in choroidal melanoma, often with geographically increased autofluorescence, whereas in choroidal nevi it is often unremarkable or shows more limited alterations.
Fundus autofluorescence adds further information for differentiating between small choroidal melanoma and nevi. It is always abnormal in choroidal melanoma, often with geographically increased autofluorescence, whereas in choroidal nevi it is often unremarkable or shows more limited alterations.
 Infrared imaging may be helpful for defining the lesion size, which can be difficult to assess with color photography.
Infrared imaging may be helpful for defining the lesion size, which can be difficult to assess with color photography.
 Examination of nevi using optical coherence tomography has revealed a higher incidence of serous exudation (26%) in comparison with ophthalmoscopy. In addition, retinal thinning, retinal edema, retinal pigment epithelial detachment, and photoreceptor attenuation have been noted in association with some nevi.
Examination of nevi using optical coherence tomography has revealed a higher incidence of serous exudation (26%) in comparison with ophthalmoscopy. In addition, retinal thinning, retinal edema, retinal pigment epithelial detachment, and photoreceptor attenuation have been noted in association with some nevi.
 Photodynamic therapy has been administered in choroidal neovascularization associated with choroidal nevi, but the results are variable.
Photodynamic therapy has been administered in choroidal neovascularization associated with choroidal nevi, but the results are variable.
References
5.2 Choroidal Melanoma
Epidemiology, Pathophysiology, and Clinical Presentation
 Choroidal melanoma is the most common type of primary malignant intraocular tumor, with an incidence of seven to eight new cases per 1 000 000 in Caucasian populations.
Choroidal melanoma is the most common type of primary malignant intraocular tumor, with an incidence of seven to eight new cases per 1 000 000 in Caucasian populations.
 The 5-year mortality rate averages between 10–50%, depending on the prognostic characteristics of the tumor. Because choroidal melanoma is generally a slow-growing tumor, it is first noticed by the patient when either the tumor directly, or the resultant accompanying exudative detachment, interfere with the fovea or the optic nerve, causing a decrease in visual acuity.
The 5-year mortality rate averages between 10–50%, depending on the prognostic characteristics of the tumor. Because choroidal melanoma is generally a slow-growing tumor, it is first noticed by the patient when either the tumor directly, or the resultant accompanying exudative detachment, interfere with the fovea or the optic nerve, causing a decrease in visual acuity.
 The more anterior a choroidal melanoma is located, the later the tumor is generally diagnosed.
The more anterior a choroidal melanoma is located, the later the tumor is generally diagnosed.
 Typical diagnostic characteristics of choroidal melanomas are their pigment content, the presence of orange pigment on the surface, an accompanying exudative detachment, and low reflectivity on ultrasonography.
Typical diagnostic characteristics of choroidal melanomas are their pigment content, the presence of orange pigment on the surface, an accompanying exudative detachment, and low reflectivity on ultrasonography.
Fluorescein Angiography
 Although choroidal melanomas can have a variety of fluorescein-angiographic characteristics, there are some characteristic patterns that can be indicative of the diagnosis.
Although choroidal melanomas can have a variety of fluorescein-angiographic characteristics, there are some characteristic patterns that can be indicative of the diagnosis.
 The fluorescein-angiographic image of a choroidal melanoma depends on the size of the tumor, its pigment content, and its interaction with adjacent tissue layers, particularly on the retinal pigment epithelium (RPE) and the retina.
The fluorescein-angiographic image of a choroidal melanoma depends on the size of the tumor, its pigment content, and its interaction with adjacent tissue layers, particularly on the retinal pigment epithelium (RPE) and the retina.
 Generally, early hypofluorescence is seen in pigmented choroidal melanomas, which can change to hyper-fluorescence in the later phases of the angiography, depending on the size of the tumor. Flat and less vascularized melanomas can also remain hypofluorescent in the late phase, as long as the RPE has no secondary changes (e. g., through chronic exudation).
Generally, early hypofluorescence is seen in pigmented choroidal melanomas, which can change to hyper-fluorescence in the later phases of the angiography, depending on the size of the tumor. Flat and less vascularized melanomas can also remain hypofluorescent in the late phase, as long as the RPE has no secondary changes (e. g., through chronic exudation).
 A typical ophthalmoscopic characteristic of choroidal melanomas of any size is the presence of orange pigment on the tumor surface; this consists of lipofuscin accumulation, which, fluorescein angiographically, leads to an earlier, “geographic” blockage of the choroid or tumor hyperfluorescence. In the later phases, these areas can appear hypofluorescent as well as hyper-fluorescent; generally, however, the blockage diminishes and produces an image of slowly increasing hyperfluorescence.
A typical ophthalmoscopic characteristic of choroidal melanomas of any size is the presence of orange pigment on the tumor surface; this consists of lipofuscin accumulation, which, fluorescein angiographically, leads to an earlier, “geographic” blockage of the choroid or tumor hyperfluorescence. In the later phases, these areas can appear hypofluorescent as well as hyper-fluorescent; generally, however, the blockage diminishes and produces an image of slowly increasing hyperfluorescence.
 With changes in the RPE, early dot-like areas of hyper-fluorescence are typical, which noticeably increase in intensity in the latter phases.
With changes in the RPE, early dot-like areas of hyper-fluorescence are typical, which noticeably increase in intensity in the latter phases.
 Occasionally, hemorrhages can be found either on the ophthalmoscopically visible superficial tumor layers between the tumor surface and the intact retina, or epiretinally; depending on length, these lead to different blockages of the underlying fluorescence.
Occasionally, hemorrhages can be found either on the ophthalmoscopically visible superficial tumor layers between the tumor surface and the intact retina, or epiretinally; depending on length, these lead to different blockages of the underlying fluorescence.
 A typical characteristic in large choroidal melanomas is penetration of the tumors through Bruch membrane, resulting in a mushroom-shaped growth. In these tumors, a characteristic image of “double circulation” can be seen in fluorescein angiography, caused by simultaneously visible retinal and tumor circulations in the early phase, or alternatively in the earlier arteriovenous phase. Hypofluorescence of the larger tumor vessels, with diffuse hyperfluorescence of the surrounding tumor tissue, can be seen during recirculation of the fluorescein in the later phases of the angiography.
A typical characteristic in large choroidal melanomas is penetration of the tumors through Bruch membrane, resulting in a mushroom-shaped growth. In these tumors, a characteristic image of “double circulation” can be seen in fluorescein angiography, caused by simultaneously visible retinal and tumor circulations in the early phase, or alternatively in the earlier arteriovenous phase. Hypofluorescence of the larger tumor vessels, with diffuse hyperfluorescence of the surrounding tumor tissue, can be seen during recirculation of the fluorescein in the later phases of the angiography.
Indocyanine Green Angiography
 The anticipated differential-diagnostic relevance of indocyanine green angiography in choroidal tumors has still not been confirmed.
The anticipated differential-diagnostic relevance of indocyanine green angiography in choroidal tumors has still not been confirmed.
 Early phase. There is hypofluorescence in the melanoma region resulting from the blockage of the choroidal filling through the tumor. Fine vessels can often be seen within the tumor—“double circulation.”
Early phase. There is hypofluorescence in the melanoma region resulting from the blockage of the choroidal filling through the tumor. Fine vessels can often be seen within the tumor—“double circulation.”
 Arteriovenous phase. There is continued blockage of choroidal filling and an appearance of hyperfluorescence in the tumor, as a sign of a leakage from the tumor vessels.
Arteriovenous phase. There is continued blockage of choroidal filling and an appearance of hyperfluorescence in the tumor, as a sign of a leakage from the tumor vessels.
 Late phase. Hyperfluorescence in the tumor increases—a leakage phenomenon.
Late phase. Hyperfluorescence in the tumor increases—a leakage phenomenon.
Fundus Autofluorescence
 Fundus autofluorescence is not useful in large melanomas. In small tumors, which are difficult to differentiate from choroidal nevi, fundus autofluorescence may reveal increased autofluorescence in regions with orange pigment and show flecked alterations in the area of the tumor, in contrast to choroidal nevi. An existing or regressed exudative reaction may be detectable through increased autofluorescence, typically below the small melanoma.
Fundus autofluorescence is not useful in large melanomas. In small tumors, which are difficult to differentiate from choroidal nevi, fundus autofluorescence may reveal increased autofluorescence in regions with orange pigment and show flecked alterations in the area of the tumor, in contrast to choroidal nevi. An existing or regressed exudative reaction may be detectable through increased autofluorescence, typically below the small melanoma.
Diagnosis and Treatment
 In general, fluorescein angiography is not of critical importance in the diagnosis of choroidal melanoma and must not be carried out for every intraocular tumor. However, it can provide important information in diagnostically difficult cases, and its contribution is particularly helpful in sparsely pigmented tumors in order to visualize the extent of the tumor and allow treatment planning. It is also helpful for differentiating between nevi and small melanomas (see section 5.1). In addition, it is a useful diagnostic tool for assessing radiation retinopathy (see section 7.11).
In general, fluorescein angiography is not of critical importance in the diagnosis of choroidal melanoma and must not be carried out for every intraocular tumor. However, it can provide important information in diagnostically difficult cases, and its contribution is particularly helpful in sparsely pigmented tumors in order to visualize the extent of the tumor and allow treatment planning. It is also helpful for differentiating between nevi and small melanomas (see section 5.1). In addition, it is a useful diagnostic tool for assessing radiation retinopathy (see section 7.11).
 A wide variety of radiotherapy and surgical treatment modalities are available for choroidal melanomas. More detailed articles and textbooks should be consulted for the appropriate treatments.
A wide variety of radiotherapy and surgical treatment modalities are available for choroidal melanomas. More detailed articles and textbooks should be consulted for the appropriate treatments.
 Recently, attempts have been made to achieve angio-graphic imaging of histologically defined and prognostically relevant microcirculation patterns in choroidal melanomas, in order to obtain an additional clinically prognostic parameter. It is not yet clear whether such imaging patterns will have prognostic relevance in everyday practice.
Recently, attempts have been made to achieve angio-graphic imaging of histologically defined and prognostically relevant microcirculation patterns in choroidal melanomas, in order to obtain an additional clinically prognostic parameter. It is not yet clear whether such imaging patterns will have prognostic relevance in everyday practice.
References
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree