, Rudolf Leuwer2, Konrad Schwager3 and Sören Wenzel4
(1)
Otology and Neurotology Division, University of Arkansas for Medical Sciences, Little Rock, Arkansas, USA
(2)
Otorhinolaryngology Head and Neck Surgery, HELIOS Hospital, Krefeld, Germany
(3)
Otorhinolaryngology Head and Neck Surgery, Klinikum Fulda, Fulda, Germany
(4)
Otorhinolaryngology Head and Neck Surgery, Pinneberg, Germany
Middle ear aeration: role of mucosa and ET
Chronic middle ear disease
Preoperative assessment
Therapy of ET obstruction: balloon dilatation
Principles of tympanoplasty
Prognosis of surgery
4.1 Eustachian Tube and Middle Ear Mucosa: Two Players that Are Not Well Understood
Good aeration of the middle ear space is a necessity for a well-functioning middle ear with regard to both infections and audiological function. Middle ear aeration is a result of a complex system involving at least two major contributors: the middle ear mucosa and the Eustachian tube [193]. Proper diagnoses of severe aeration problems and tube dysfunction are difficult because the system, its parts and their complex interaction are not fully understood.
Sadé and Ar [163] ascribe the major role of maintaining good aeration in the middle ear space to the middle ear mucosa. Examination of the middle ear reveals that those with good aeration have a well-aerated mastoid process whereas those with little aeration are characterized by contracted or poorly developed mastoids. The theory of the mucosa’s contribution is supported by studies of total blockage of the Eustachian tube, which showed that continuous gas exchange in the middle ear space [192] is responsible for the continuous support of middle ear pressure. However, because the mucosa is too slow in following atmospheric pressure changes, this falls to the role of the Eustachian tube. In cases of acute and dramatic pressure changes, such as those that occur in diving or during an airplane flight, the Eustachian tube plays the additional role of an emergency valve. The Eustachian tube opens during procedures like swallowing, masticating and yawning, which help to in- or desufflate the middle ear space according to actual needs.
Classical tympanoplasty techniques solve mechanical problems, such as disrupted and fixed ossicular chains and perforated eardrums, but have little effect upon tubal dysfunction. There has been a trend towards surgical procedures that preserve the mucosa of the mastoid and antrum, with the concept that disruption of the mucosa is as counterproductive in temporal bone surgery as it is in sinus surgery. Thus, the surgical principle when treating chronic middle ear diseases is to support mucosal healing while restoring a closed middle ear space. In contrast to other surgical fields, it is not always possible to work in a noninfected environment in chronic otitis media as the surgery itself is conducted to achieve a dry, noninfected ear [212].
When dealing with the complex functional situation of the Eustachian tube and the middle ear mucosa, surgical solutions must deviate from pure mechanical manipulations, such as tympanoplasty. However, convincing results of the direct procedures suggested for Eustachian tube dysfunction are lacking. It is no wonder, then, that regardless of the large number of patients who experience Eustachian tube dysfunction and middle ear mucosa disorders, the number of patients in studies of direct Eustachian tube treatment is amazingly low.
4.1.1 General Assessment Prior to Middle Ear Surgery
Preoperative assessment includes a complete ENT examination. Of major interest is the situation in the nasopharynx, the soft palate, the lymphatic tissue, the adenoids and the tubal orifice and its surroundings. The extent of required imaging depends on the need for visualization of the disturbance. Although a plain radiograph (Schüller’s view) can be obtained to get information on the middle ear space aeration status, CT scanning of the temporal bone affords more precise visualization. If information about the Eustachian tube’s soft tissue is needed, MRI scanning is necessary. A complete audiometric evaluation, including pure tone and speech audiometry and speech discrimination, should be performed on all patients prior to middle ear surgery. The tuning fork examination according to Weber and Rinne is also necessary to confirm findings obtained in the audiogram.
4.1.2 Eustachian Tube: Preoperative Testing and Evaluation
Preoperative testing of Eustachian tube function is limited. The major clinical test for the Eustachian tube is Valsalva’s manoeuvre [115,200,201]. The preoperative assessment before any ear surgery should include this simple tubal function test. If the patient is not able to perform the test, the variation according to Toynbee with a simultaneous swallowing manoeuvre may be helpful. Politzer’s manoeuvre using the rubber balloon on the nostril when performing a k-plosive by the patient is more forceful but can still provide information about Eustachian tube patency. If the ear is Valsalva positive, then there is at least no mechanical blockage of the tube.
The patency of the Eustachian tube is most important regarding drainage function. Even if the situation for ventilation of the middle ear space is unclear, the Eustachian tube may still drain properly. A patient who is able to perform Valsalva’s manoeuvre may be able to open his/her Eustachian tube postoperatively, and secretions from the middle ear can then be transported out of the middle ear space. However, this only indicates that there is an open passage; it is not a robust test of Eustachian tube function. Direct inflation using a tubal catheter [193], in our opinion, has no advantage, does not provide further information and is obviously more invasive.
4.2 Conservative Treatment of the Eustachian Tube Obstruction
Stangerup et al. [186] examined 45 children and 49 adults at Copenhagen Airport on 2 days in May 1995 for baro-otitis after landing. Barotrauma was classified otoscopically; middle ear pressure was assessed by tympanometry. About 25 % of the younger children suffered from baro-otitis. Whereas 21 % of these children were able to equilibrate their middle ear pressure by Valsalva’s manoeuvre, 82 % could successfully increase middle ear pressure when using the Otovent™ treatment system for autoinflation.
4.3 Eustachian Tube Surgery: Tuboplasty Procedures – Bypass Surgery
A tuboplasty is any treatment directly impacting the Eustachian tube. Historically, there have been many tuboplasty procedures, including radioactive seed implantation (Sr-90), irradiation [164], bypass surgery (frontal sinus–middle ear, maxillary sinus–middle ear) [54] and tubal treatment via the middle fossa approach [71]. The tympano-oral conduit approach was performed in cadavers [88], and surgery creating a bypass parallel to the Eustachian tube was performed experimentally in dogs, followed by application in humans [121].
Many of these studies did not exceed the status of preliminary reports, and no major series were published. Other treatments, such as the Fulda aeration surgery [76] and similar procedures, demonstrate the multiple attempts to help patients with severe aeration problems. However, none of these extensive techniques has been proven in a major series.
4.3.1 Tubal Insertion
There have been several attempts to keep the lumen of the Eustachian tube open. Plastic catheters have been inserted, but the reports are only anecdotal and improvement lasted for only a short period of time [142]. Several publications from various institutions describe the gold wire tube conductor introduced by Steinbach (Fig. 4.1). Lieberum and Jahnke [95] reported an increase of aeration after insertion of the wire in 11 out of 13 patients. Schrom et al. [171] inserted the gold wire in 125 patients, but 92 % showed no difference in tubal function after the procedure.


Fig. 4.1
Tube conductor (after Steinbach). X-ray of the skull p.-a
4.3.1.1 Balloon Dilatation of the Cartilaginous Portion
For cases of chronic obstructive Eustachian tube dysfunction, “balloon Eustachian tuboplasty” (BET) has been recently introduced by two different groups: the Bielefeld group [129] and the Boston group [144]. The method of dilatation of the cartilaginous part of the Eustachian tube has been proven feasible and safe in cadaver studies [112] and human adults [144]. Poe et al. [144] with their later study used their own catheter. In BET a balloon catheter is placed into the cartilaginous portion of the Eustachian tube by transnasal endoscopy-controlled insertion. The length of this balloon (Bielefeld balloon catheter, distribution by Spiggle and Theis®, Overath, Germany) with the Sudhoff group is 2 cm. This balloon is dilated up to 10 bar over a period of 2 min. With the dilation procedure, microfractures of the tubal cartilage with a successive expansion of the Rüdinger’s safety canal could be experimentally observed, but the in vivo mechanism of the therapy remains unclear. Sudhoff and colleagues [190] treated 351 patients, of which the short-term results of 167 patients 2 months after the treatment and the long-term results of 53 patients 1 year after the treatment were recently published. They very thoroughly examined the pre- and postoperative Eustachian tube function using a modified manometry after the method of Estève. Depending on the relief with some of their patients, the dilation manoeuvre was repeated. According to their results, this procedure was satisfactory for 87 % of their patients. The Eustachian tube function tests were significantly better in more than 90 % of the cases.
4.3.2 Tubal Augmentation
The reports on augmentation surgery in the osseous part of the Eustachian tube are few. Steel probes were used to open soft tissue and osseous stenosis followed by palisade cartilage tympanoplasty, and good results were reported [63]. Charachon et al. [20] reported on a series of 17 patients in whom the osseous tube was opened and a silastic guide was inserted to keep the lumen patent. This could be achieved in nine ears. Extended tubotympanoplasty and drilling of the osseous part of the tube led to improvement in two of five patients in a study of Kumazawa et al. [87].
4.3.3 Laser Tuboplasty
Laser procedures have become popular in all fields of medicine. Laser treatment of the Eustachian tube is favoured as well. Success rates of laser tuboplasty are reported in up to 70 % of patients [86]. However, it should be noted that the laser treatment is directed towards the pharyngeal orifice or, additionally, the middle ear orifice of the Eustachian tube. It is no general treatment of the tube and does not encompass the mucosa/Eustachian tube system. Another issue with laser treatment is scarring. All procedures involving laser treatment lead to scarring to some extent; however, with regard to tubal function, this is a feared outcome as scarring is a major reason for dysfunction and tubal blocking.
4.3.4 The Unaerated Middle Ear: Total Stenosis of the Eustachian Tube
In cases of very reduced or no aeration of the middle ear space, Wullstein suggested type IV tympanoplasty. The main principle is to protect the round window from sound impact, so the sound wave enters the cochlea at the oval window solely. Absence of the tympanic membrane and ossicular chain leads to a conductive hearing loss of around 30 dB. Gerhardt [50] inserted an air-filled silicone bubble in the round window niche for better protection in type IV tympanoplasties. The type IV tympanoplasty may still be helpful in an atelectatic ear with or without cholesteatoma, providing a safe situation regarding infection but still bearing a large conductive hearing loss. Today, alternatives to the non-reconstructed middle ear mechanism exist in the form of bone-anchored or implantable hearing aids.
4.4 Eustachian Tube and Tympanoplasty
Tympanoplasty itself does not improve Eustachian tube function [68]. One main principle in tympanoplasty should always be to rely on the natural anatomical construction plan of the middle ear, so minimal changes should be made to help nature restore the middle ear’s function [209]. If it is possible to leave the chain intact, ossicles should not be removed. A type I or type II tympanoplasty is preferred over techniques that require more extensive restorations, such as the type III tympanoplasty. Middle ear pressure should stabilize after 4 years, except in cases of cholesteatoma [202]. Alternatives to classical middle ear surgery using electrical hearing devices will be discussed at the end of this chapter.
4.4.1 Basic Considerations in Tympanoplasty. Two Main Goals: Eradication of Disease and Restoration of Hearing
The first aim of treatment in chronic middle ear disease is to cure the chronic inflammation. The risk of complications will depend on the entity of the middle ear disease. The most dangerous disease regarding infectious complications is undoubtedly cholesteatoma. Otogenic facial paresis, labyrinthitis, intracranial complications, sinus thrombosis, meningitis and epidural, subdural and brain abscess, when they occur, are regularly associated with cholesteatoma. The simple perforation of a mesotympanic otitis media may be recognized as less dangerous. A runny ear with slowly increasing hearing loss may be seen as a less dramatic situation, and the risk of life-threatening complications is negligible. Nevertheless, in the case of chronic suppurative otitis media or even with unspectacular chronic otitis media with effusion, all these major complications are possible.
The second aim in treating chronic middle ear disease is restoration of hearing. Since the beginning of modern tympanoplasty techniques in the 1950s, according to Moritz, Zöllner and Wullstein, attention has been recently more focused on hearing restoration techniques.
4.4.2 Materials for Reconstruction of the Tympanic Membrane
Many materials have been suggested for tympanic membrane reconstruction. Three tissues of autogenous origin are used today: temporal fascia (likely the material most favoured by surgeons all over the globe), perichondrium and cartilage [65]. Temporal fascia is easy to harvest and elegant to handle. Similar to fascia is perichondrium, which can be harvested either from the tragus or from the concha. Fascia and perichondrium are of similar resistance although some clinicians see advantages when using perichondrium [66]. Fascia and perichondrium are the materials of choice when the tympanic membrane is still cone-shaped because of the flexibility of the material. Fascia and perichondrium should be used in cases of primary surgery. In revision surgery cases and in atelectasis, a more resistant material is needed. Thus, cartilage is the material of choice for retraction pockets and atelectatic ears.
4.4.2.1 Harvesting Perichondrium and Cartilage
Cartilage and perichondrium are harvested either from the tragus or from the concha. The ideal region in the concha is the region of the cymba (Fig. 4.2a, b). In this area the cartilage is about 1 mm thick, and it is relatively flat with no disturbing connective tissue adhesions. An incision is made through the cartilage using a number 10 blade, and Metzenbaum scissors are used to remove the perichondrium, alone or attached to a piece of cartilage, leaving the anterior perichondrium in place. In a similar way, both materials can be harvested from the tragus. For cosmesis, the cut through the skin and cartilage should be performed about 2–3 mm beneath the free margin of the tragus (Fig. 4.3a, b). The cartilage can be used as a composite graft (cartilage/perichondrium island flap), as a cartilage plate or as shingles or palisades in a palisade technique [33,116].
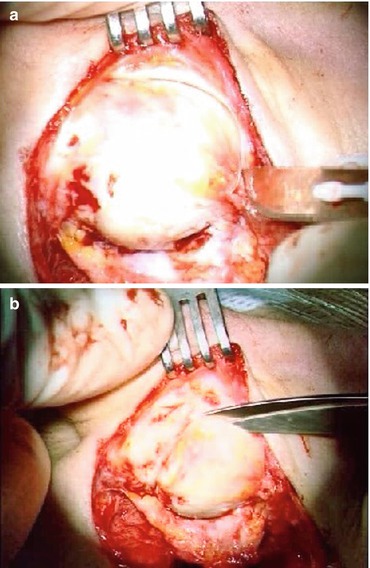
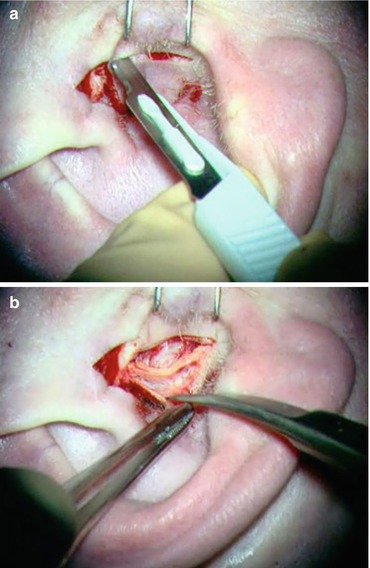
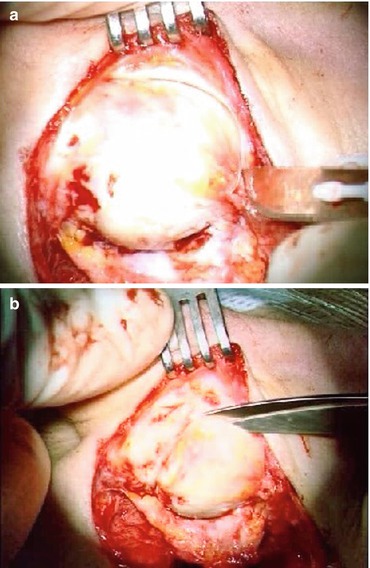
Fig. 4.2
(a) Harvesting cartilage from the concha (cymba), cut through the cartilage. (b) Preparation of cymbal cartilage
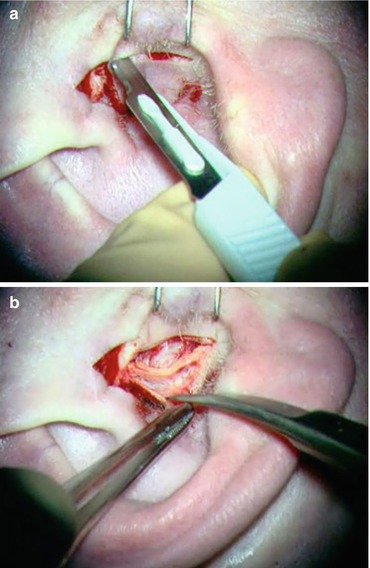
Fig. 4.3
(a) Harvesting cartilage from the tragus. Cut should be 2 mm lower to the free margin for reasons of cosmesis. (b) Preparing tragal cartilage
4.4.2.2 Creating a Cartilage/Perichondrium Island Flap
To create a cartilage/perichondrium island flap, the cartilaginous margin of the harvested composite piece of cartilage and perichondrium is thinned using a number 10 blade. If using concha cartilage, the thinning is performed on the concave side, thus forcing the perichondrium fibres to bend the cartilage towards the opposite side and straightening the flap. The tragal cartilage may be slightly thinner and may not require this marginal trimming. The cartilage of the margin may then be removed with a Plester knife, thus creating a rim of perichondrium around the graft (Fig. 4.4). The acoustic properties of cartilage have been studied extensively by Zahnert and co-workers [215]. The results show that there is no obvious acoustical disadvantage using cartilage versus perichondrium or fascia, but the advantages in stability are enormous.


Fig. 4.4
Creating cartilage/perichondrium island. Notice rim in the middle for the malleus handle
4.4.2.3 Palisade Technique
Heermann has used cartilage palisades since the late 1950s. The technique consists of placing longitudinal strips of cartilage parallel to the malleus handle while avoiding blockage of the orifice of the Eustachian tube in the middle ear [64]. The tympanic membrane reconstruction starts anteriorly, just above the opening of the Eustachian tube in the middle ear. Gaps between the palisades have to be avoided. It is helpful to cut the palisades like shingles and to pose them like shingles on a roof (Figs. 4.5 and 4.6).
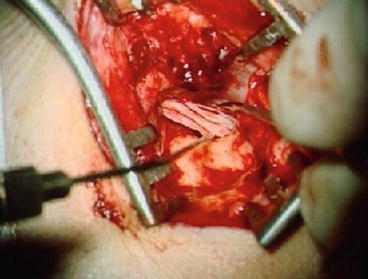
Fig. 4.5
Cutting shingles
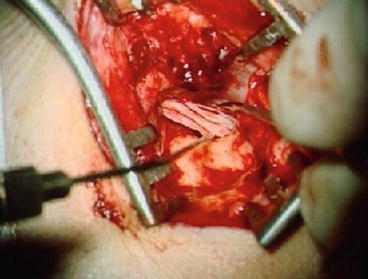
Fig. 4.6
Reconstruction of right tympanic membrane with palisades
Silastic sheeting of tympanic membrane and posterior wall reconstruction helps to avoid major granulation tissue growth in the early postoperative period (Fig. 4.7).
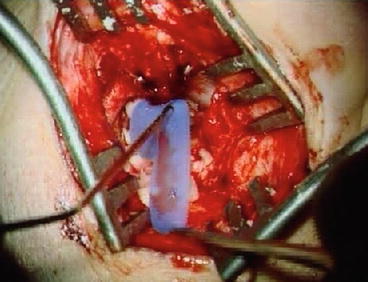
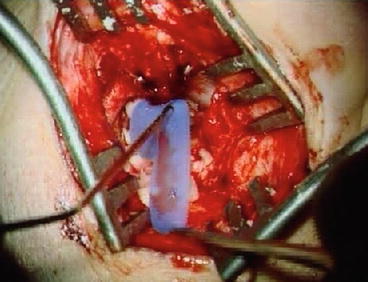
Fig. 4.7
Covering the reconstructed posterior wall, tympanic membrane and outer ear canal with silastic sheets (left ear)
4.4.3 Materials for Reconstruction of the Ossicular Chain
A broad variety of materials are used for reconstruction of the ossicular chain. A patient’s own material remains the gold standard. Autogenous ossicles, with the incus being the first choice, followed by the head of the malleus, are used with great acceptance. Adverse reactions from the implantation site are not expected. If the reconstruction is dislocated, there may be a problem with growth towards the promontory or the Fallopian canal, resulting in osseous fixation. Use of ossicles from ears with chronic otitis, where quite an amount of osteitis has been described histologically [46], is questionable. However, it is doubtful that the histological finding of osteitis is a problem for mechanical instability; rather, it may be the expression of the chronic otitis media itself. In cases of cholesteatoma, the use of a patient’s own ossicles should be avoided in order to prevent recurrences.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


