Classification
Traumatic optic neuropathy is classically separated into two types of injury: direct and indirect. Direct optic nerve injuries result from orbital or cerebral trauma that transgresses normal tissue planes to disrupt the anatomic and functional integrity of the optic nerve, due to a penetrating force that directly collides with the optic nerve. Indirect injuries are caused by forces transmitted at a distance from the optic nerve. Normal tissue planes are not transgressed in indirect optic nerve injuries. Instead, the anatomy and function of the optic nerve are compromised by energy absorbed by the nerve at the moment of impact. The classic example of an indirect injury to the optic nerve is that which occurs when blunt trauma to the forehead results in a transmission of force through the cranium to the confined intracanalicular portion of the nerve.
The prognosis of an optic nerve injury depends in part on whether it is direct or indirect. Direct injuries tend to produce severe and immediate visual loss with little likelihood of recovery. Indirect optic neuropathies, on the other hand, are not infrequently associated with visual recovery and may also produce delayed visual loss that occurs several hours to days after the injury.
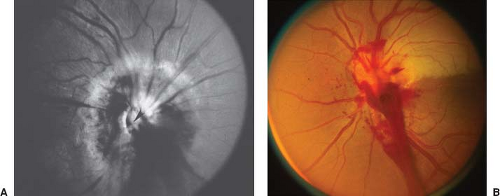
Optic nerve injuries can also be classified anatomically as optic disc trauma (avulsion), anterior optic neuropathy, or posterior optic neuropathy. An avulsion of the optic nerve as it enters the globe produces a distinct ophthalmoscopic appearance, consisting of a partial ring of hemorrhage at the optic nerve head. In some cases, the site of the avulsion can be identified (Fig. 9.1A).
Injuries to the proximal portion of the optic nerve within 10 mm of the globe, anterior to where the central retinal vessels penetrate the nerve, produce a variety of disturbances that are immediately apparent in the ocular fundus, including an ophthalmoscopic picture of a central retinal or branch artery occlusion, central retinal vein occlusion, or anterior ischemic optic neuropathy (Fig. 9.2).
In contrast, injuries to the optic nerve posterior to the entrance of the central retinal artery produce no immediate change in the appearance of the ocular fundus. Specifically, the optic disc remains normal in appearance for at least 3 to 5 weeks, following which it becomes pale. The most common site of posterior indirect optic nerve injury is the optic canal.
The intracranial optic nerve is the next most common site of injury. When the intracranial portion of the optic nerve is injured, the field defect is likely to be hemianopic, and bilateral injury is common, as is associated injury to the optic chiasm.
Epidemiology
The type of trauma that produces a traumatic optic neuropathy is usually a deceleration injury of significant momentum. In cases of isolated traumatic optic neuropathy, the force of the impact is typically directed to the ipsilateral forehead or to the midface region. Motor vehicle and bicycle accidents are the most frequent causes, accounting for 17% to 63% of cases. Motorcycle accident victims may be particularly vulnerable to traumatic optic neuropathy, with up to 18% of such accidents resulting in optic nerve dysfunction. Falls are the next most common cause. Traumatic optic neuropathy can also occur in such diverse settings as frontal impact caused by falling debris, assault, stab wounds, gunshot wounds, and following seemingly trivial head trauma. It may also occur from iatrogenic injury, particularly after endoscopic sinus surgery and orbital surgery. Optic nerve injury is often associated with multisystem trauma and serious
brain injury. Loss of consciousness occurs in 40% to 72% of patients with traumatic optic neuropathy, and traumatic optic neuropathy occurs in about 1.6% of head trauma cases and in 2.5% of patients with maxillofacial trauma.
brain injury. Loss of consciousness occurs in 40% to 72% of patients with traumatic optic neuropathy, and traumatic optic neuropathy occurs in about 1.6% of head trauma cases and in 2.5% of patients with maxillofacial trauma.
Traumatic optic neuropathy that occurs in the setting of orbital hemorrhage defines an important subset of optic nerve injury that does not fit well into the classic delineation of direct and indirect optic nerve injuries. For example, orbital hemorrhage after
retrobulbar block occurs in 0.44% to 3% of patients. In most cases, the hemorrhage is quickly recognized and readily managed, with little impact on visual outcome unless a direct optic nerve injury has occurred from perforation of the nerve by the retrobulbar needle. Thus, the incidence of traumatic optic neuropathy in the setting of iatrogenic orbital hemorrhage is extremely low.
retrobulbar block occurs in 0.44% to 3% of patients. In most cases, the hemorrhage is quickly recognized and readily managed, with little impact on visual outcome unless a direct optic nerve injury has occurred from perforation of the nerve by the retrobulbar needle. Thus, the incidence of traumatic optic neuropathy in the setting of iatrogenic orbital hemorrhage is extremely low.
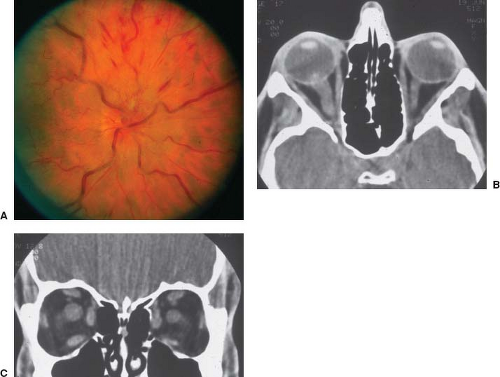
When retrobulbar hemorrhage occurs in association with blunt trauma to the orbit, the risk of visual loss is much greater. In this setting, blood may be dispersed throughout the orbit, in the subperiosteal space, and in the optic nerve sheath. In other cases, a hematic cyst may form, resulting in optic neuropathy from compression of the nerve by the cyst. Imaging studies can help to localize the hemorrhage in such cases. Orbital emphysema is also a rare cause of optic nerve injury. It can follow orbital fractures, usually after vomiting or nose blowing force air into the orbit, compromising the optic nerve.
Clinical Assessment
Traumatic optic neuropathy is a clinical diagnosis typically made when there is evidence of an optic neuropathy that is temporally related to blunt or penetrating head trauma. The head trauma may have been severe, in which case the patient may be unconscious. In some cases, there is no other evidence of orbital or ocular trauma; in other cases, there is obvious evidence of injury to the eye or orbit, such as periorbital or ocular hemorrhage, ecchymosis, or lacerations.
The clinical evaluation of a patient with visual loss following trauma should begin with a complete history, usually obtained from family, friends, or witnesses to the trauma. It is particularly important, for both medical and legal purposes, to determine if the patient with evidence of visual loss had any visual deficits before the injury. The examination of a patient with a possible traumatic optic neuropathy is limited by numerous patient factors, including the presence or absence of other injuries, the patient’s level of consciousness, and the patient’s ability or willingness to cooperate with the examiner. Hence, a good history and careful objective examination is critical.
The severity of initial visual loss in patients with traumatic optic neuropathy varies dramatically, from no light perception to 20/20 with an associated field defect. The prevalence of severe initial visual loss from traumatic optic neuropathy probably ranges from 43% to 56%. Visual loss is more likely to be severe in patients with neuroimaging evidence of a fracture of the optic canal, often signifying direct injury to the optic nerve. Delayed visual loss is reported to be as high as 10% in some series. Color vision, an excellent test of optic nerve function, can be assessed at bedside using a red object and/or color plates.
In cases of unilateral traumatic optic neuropathy a relative afferent pupillary defect




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree