Transoral Lateral Oropharyngectomy (Huet’s Procedure)
F. Christopher Holsinger
INTRODUCTION
The changing epidemiology of oropharyngeal cancer (OPC) has led to a greater role for transoral head and neck surgery within the multidisciplinary treatment paradigm. Reports from the United States and abroad have documented the precipitous rise in the incidence of OPC in individuals younger than typically expected for “traditional” patients with cancer of the head and neck. In a 2008 prospective case-control study, D’Souza and Gillison demonstrated an association between human papillomavirus (HPV) and OPC, as well as the role of increasing oral sexual partners. Using the Surveillance, Epidemiology, and End Results (SEER) repository, Chaturvedi reported in 2011 that the incidence of HPV-positive cancers of the oropharynx increased by 225% from 1988 to 2004. In addition, these HPV+ cancers usually present with a smaller size primary (T0-T2) than HPV-negative OPC, permitting effective transoral resection.
Fortunately, these cancers tend to respond favorably to standard organ preservation approaches. In RTOG 0129, Ang et al., highlighted the significant impact HPV status has on the treatment of OPC; after adjusting for demographics, T stage, N stage, and smoking, patients with HPV+ OPC had a 58% reduction in the risk of death and a 51% reduction in risk of progression or death. While these response rates are encouraging, young survivors of OPC have the potential to live decades with the sequelae of the treatment. Hutcheson et al., have recently drawn attention to the long-term chronic severe dysphagia and cranial neuropathies that may develop or progress years after radiation-based therapy for OPC.
Given the potential long-term sequelae of radiation in a rapidly enlarging population of young patients with OPC, transoral and endoscopic approaches to the tonsil and lateral oropharynx will play a greater role in the management of patients with OPC. With the development of surgical technology, including the surgical robot and laser techniques, the surgical procedure described here has more widespread application for transoral resection of cancers of the oropharynx.
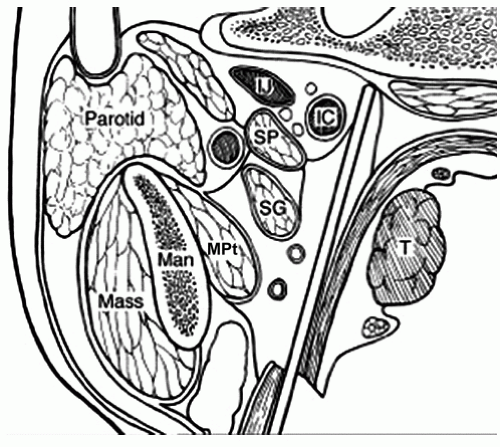
The French head and neck surgeon Pierre-Charles Huet first described the transoral technique for resection of cancer of the lateral wall of the oropharynx, including the tonsil, tonsil fossa, and anterior tonsil pillar (ATP) (Fig. 14.1). In 2005, the first description of this surgical technique “transoral lateral oropharyngectomy” (TLO) was published in English and serves as the basis of subsequent robotic-assisted approaches. Huet’s work demonstrated a safe approach to the parapharyngeal space (Fig. 14.2) to reduce substantially the risk of vascular injury while providing a comprehensive mucosal and deep muscular margin resection of the lateral wall of the oropharynx.
HISTORY
In addition to assessing the patient for the classical head and neck symptoms, such as dysphagia, weight loss, throat pain, oral bleeding, or mass in the neck, the head and neck surgeon should address several specific signs and symptoms for a candidate patient for TLO. These should include prior history of radiotherapy, dentition, cervical spine restriction on neck extension, and Mallampati classification.
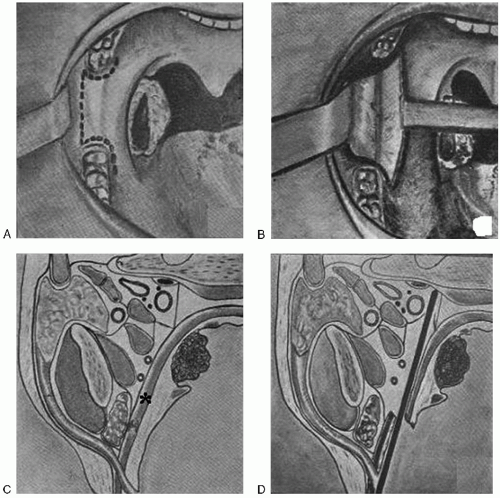 FIGURE 14.1 (Used with permission from Masson Editeurs [120, Bd. Saint-Germain, 75272 Paris Cedex 06, France]). Panel A: (upper left) demonstrates Huet proposed incisions. Panel B: (upper right) reveals the approach to the deep margin, opening the potential space between the medial pterygoid muscle and the superior constrictor, underlying the palatine tonsil. Panel C: (lower left) represents cross-sectional anatomy of the lateral oropharyngeal wall, with an asterisk inserted over the superior constrictor muscle. See Figure 14.2 below for further anatomic detail and higher resolution. Panel D: (lower right) demonstrates the proper cleavage plane to obtain complete mucosal and muscular resection of the lateral oropharyngeal wall. |
PHYSICAL EXAMINATION
As always, a complete head and neck examination should be performed preoperatively. Visual inspection and careful palpation of the ipsilateral tonsillar fossa is important to properly select patients for this surgery. The surgeon should confirm that the tumor is “mobile.” That is, compared to the uninvolved contralateral tonsil, the tumor should roll and pivot as the lateral wall of the oropharynx is carefully palpated. If the tonsil is adherent to the underlying superior constrictor muscle, digital manipulation will reveal this. Fixation of the tonsil to the deep planes of the wall of the oropharynx is a contraindication to surgery.
The boundaries of the tonsil fossa must be carefully examined. Tumors that involve the ATP may extend onto the mobile tongue and floor of mouth. These cancers of the ATP may even extend superficially past the retromolar trigone and toward the buccal mucosa so these areas should be inspected with a bright light and be palpated. The posterior tonsil pillar should also be carefully examined. Tumors that have extensive involvement of the posterior tonsil pillar have a higher rate of local recurrence after Huet procedure and may also have a primary nodal echelon that drains to the retropharynx. Tumors in this site are probably better treated with radiation therapy.
The surgeon should also carefully evaluate the remainder of the patient’s base of the tongue and contralateral tonsil, for sites of synchronous “second” primary cancers, especially in the case of smokers. Synchronous contralateral tonsil cancers are exceedingly rare, but other cancers or premalignant foci in the oral cavity or base of the tongue can sometimes be found. I always measure the extent of spread vertically, to the soft palate above, and inferiorly below to the supraglottic larynx. For instance, when the inferior pole of the tonsil is involved, I always carefully discern the relationship of this cancer to the pharyngoepiglottic fold below and look for potential “cascading” extension into the base of the pyriform sinus, the gateway to the hypopharynx.
Finally, it is important to measure and document interincisor opening, allowing the surgeon to estimate how easy transoral access will be for the surgical resection. I also use the Mallampati scale to estimate the difficulty of exposure. In general, the higher the Mallampati score, the more difficult it is to gain exposure in the operating room.
I always perform an ipsilateral neck dissection of levels II-IV. This can be staged or done concurrently. I do not frequently dissect level I-b, as this nodal echelon is more commonly involved in oral cavity, rather than OPCs. However, I will always fully skeletonize and resect lymphoadipose tissue along the posterior facial vein, which forms the lateral border of I-b, and its path toward the internal jugular vein. As part of the neck dissection of levels II-IV, I’ll usually include some of the anterior most aspect of level Vb—those nodes imbricated within the cervical plexus, which I routinely spare.
Though many tumors are resectable via transoral surgery, I tend to operate on patients with limited neck disease, typically N0-2a and occasionally N2b. Patients with N3 neck disease are better served generally with upfront induction chemotherapy, followed by risk-based locoregional therapy, depending on response.
Many head and neck oncologists are rightfully concerned about the retropharyngeal lymphatics in patients with tonsillar carcinoma. In general, patients with posteriorly based tumors, especially toward the posterior oropharyngeal wall or posterior tonsil pillar, are at highest risk for retropharyngeal metastasis. I tend not to operate on these patients. Occasionally though, I will encounter nodes just superficial to the parapharyngeal adipose tissue. With experience, these can be safely removed via transoral exposure.
INDICATIONS
T1-T2 cancers of the lateral wall of the oropharynx, including the tonsil fossa and ATP
Selected T3 lesions, especially exophytic cancers, may also be amenable to transoral resection.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree