Transnasal Balloon Dilation
Michael Setzen
INTRODUCTION
Thirty-seven million Americans suffer from chronic rhinosinusitis (CRS). Treatment begins with medical therapy, and if this fails, endoscopic sinus surgery (ESS) is the mainstay of treatment. Medical treatment should be anywhere from 3 to 4 weeks and sometimes 12 weeks and includes the use of some or all of the following: antibiotics, steroid nasal sprays, oral steroids, antihistamines, leukotrienes, saline, analgesics, steam, and hydration.
The goals of ESS include improving aeration, ventilation, and drainage of the involved sinus or sinuses with removal of inflammatory tissue and/or osteitic bone.
ESS has been enhanced since its inception in the early 1980s. This advance has occurred as a result of better imaging of the sinuses with multiplanar computed tomography (CT) and the introduction of the endoscope. With the advent of powered instrumentation (microdebrider), surgical navigation, and most recently balloon catheter technology (BCT), the techniques and tools utilized in ESS have witnessed significant evolution in the last decade.
The concept of preservation of normal structures while simultaneously promoting drainage and ventilation of the sinuses has been pioneered for the last 35 years first by Messerklinger and Stammberger and then by Kennedy who introduced this into the United States in 1985 and termed this conservative approach “Functional Endoscopic Sinus Surgery.” Instrumentation used to accomplish this goal of preserving tissue while creating outflow drainage included forceps, curettes, and microdebriders.
Stammberger noted that delicate removal of the obstructing cells in the frontal recess allows frontal sinus outflow tract drainage, thereby preserving frontal sinus mucosa. Kennedy noted that following removal of diseased mucosa from a sinus, the regenerated tissue has remarkably diminished ciliary density and therefore recommended that a mucosal sparing technique be used wherever possible.
In an effort to be even more conservative with respect to tissue removal, sinus BCT was introduced into otolaryngology based on recent success observed with its application in cardiology, urology, gastroenterology, and vascular surgery. Balloon use was first reported in 2005 when a cadaveric study demonstrated its safety and feasibility in paranasal sinus dilation. This was followed by Bolger and Brown’s “first-in-man” study in which balloon catheter dilation was successfully performed on 10 patients with CRS.
Balloon technology has provided the surgeon with an additional tool to navigate the frontal sinus, sphenoid sinus, and maxillary sinus ostia. Transnasal balloon dilation, or better now called balloon sinus ostial dilation, allows the surgeon access via the nose into the sinus ostia with dilation of the narrowed ostium through balloon inflation. Particularly with respect to the frontal sinus, which has historically represented the most technically challenging of all the sinuses to access, balloon devices can assist in locating the frontal sinus ostium and its outflow tract with subsequent dilation of the involved sinus ostium. If necessary, one can then perform traditional surgery on the frontal sinus if the balloon alone does not result in an adequate drainage pathway. The balloon device is designed to microfracture and mobilize the bony fragments surrounding the sinus ostia by inflating the catheter balloon to a specific diameter under high pressure.
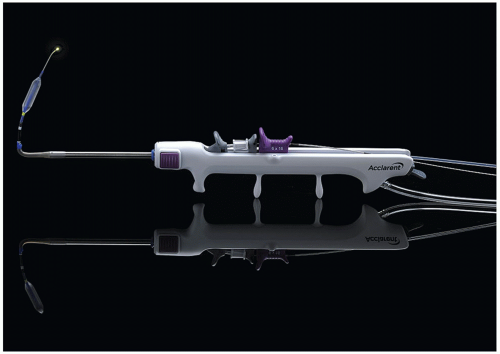
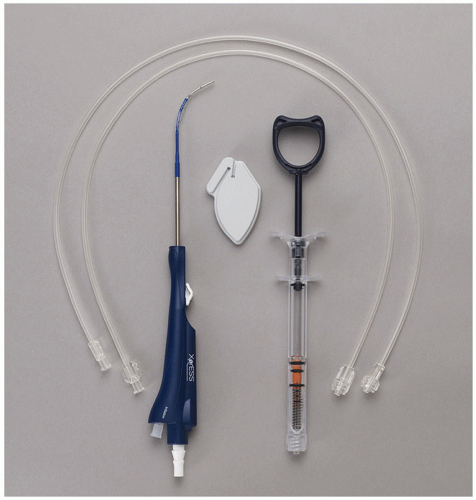
The technology has been pioneered primarily by two companies: Acclarent, Inc. (Menlo Park, CA, USA), Relieva Spin device (Fig. 11.1), and Entellus Medical, Inc. (Maple Grove, MN, USA), Gen2 Xpress
device (Fig. 11.2). Acclarent began investigating the feasibility of this technology for the sinuses in 2002. Their balloon dilation device was approved by the U.S. Food and Drug Administration (FDA) in 2005 and launched as balloon sinuplasty. With this procedure, a guide catheter is placed into the nasal cavity under endoscopic visualization and a flexible guidewire is then placed into the catheter until it reaches the target sinus. A balloon catheter is then passed over the wire using the Seldinger technique and the sinus ostium dilated. Since that time, more than 6,500 otolaryngologists have been trained in a balloon sinuplasty, and more than 300,000 patients have been operated upon to date, with 30,000 having undergone this procedure in an in-office setting.
device (Fig. 11.2). Acclarent began investigating the feasibility of this technology for the sinuses in 2002. Their balloon dilation device was approved by the U.S. Food and Drug Administration (FDA) in 2005 and launched as balloon sinuplasty. With this procedure, a guide catheter is placed into the nasal cavity under endoscopic visualization and a flexible guidewire is then placed into the catheter until it reaches the target sinus. A balloon catheter is then passed over the wire using the Seldinger technique and the sinus ostium dilated. Since that time, more than 6,500 otolaryngologists have been trained in a balloon sinuplasty, and more than 300,000 patients have been operated upon to date, with 30,000 having undergone this procedure in an in-office setting.
Entellus Medical recognized there was a problem gaining access to the maxillary sinus ostium transnasally with the original BCT. Since this was essentially performed as a blind procedure, accessory maxillary sinus ostia were often being cannulated instead of the true natural ostium. Consequently, they developed a transantral approach in which direct access to the maxillary sinus ostium was accomplished via the canine fossa so that there would be no manipulation within the nose. This device was referred to as the Functional INfundibular Endoscopic Sinus System and was approved by the FDA in 2008. Subsequently, Entellus developed the XprESS Multi-Sinus Dilation Tool, a balloon device that consists of a curved sinus seeker with a malleable tip and overlying slideable balloon for transnasal endoscopic cannulation of the sinuses. Unlike the Acclarent balloon, no wire or catheter is necessary.
The use of the balloon in treating sinusitis is threefold:
A. Stand-alone: The balloon is used to find and dilate the sinus ostium (e.g., the maxillary sinus) without tissue removal or any additional sinus surgery being performed.
B. Hybrid procedure: (a) The balloon is used to identify the ostium (e.g., the frontal sinus) and dilate it, and if need be, a traditional ESS is then done on an unrelated affected sinus. This is one form of hybrid surgery,
that is, stand-alone on one sinus and ESS on another sinus. (b) The balloon is used as an ostium seeker, (e.g., frontal sinus ostium) with traditional ESS performed on the same sinus once its ostium has been located and dilated. This is another form of hybrid surgery, that is, balloon dilation and ESS on the same sinus.
that is, stand-alone on one sinus and ESS on another sinus. (b) The balloon is used as an ostium seeker, (e.g., frontal sinus ostium) with traditional ESS performed on the same sinus once its ostium has been located and dilated. This is another form of hybrid surgery, that is, balloon dilation and ESS on the same sinus.
HISTORY
The patient typically has limited disease of the sinuses with or without minimal ethmoid involvement. This may be:
An isolated frontal or both frontal sinuses
An isolated maxillary or both maxillary sinuses
Isolated sphenoid or both sphenoid sinuses
A combination of any of the above
The best uses are for the elderly debilitated individual who cannot undergo an extensive ESS procedure nor have general anesthesia; this can be done in an office or intensive care unit (ICU) setting.
Patients with a bleeding disorder, where no tissue is to be removed, and the ostium can be dilated to promote drainage.
As a guide in gaining access to a sinus, in particular the frontal sinus (whereby it can be used as a frontal sinus seeker). This is now used by many surgeons, who over the years have found it difficult to find and navigate the frontal sinus ostium and the nasofrontal recess where the anatomy can be complex and rather confusing.
Since this is a surgical procedure, albeit conservative, the patient should still always be treated first with appropriate medical therapy including those medications previously discussed and should be tried for a minimum of 3 to 4 weeks.
If this medical therapy fails, then the patient can undergo ESS, and the balloon would be a reasonable first choice as a stand-alone procedure or part of a hybrid procedure.
The history should include nasal congestion, postnasal drip, facial pain, headache, fever, anosmia, cough, and general malaise in accordance with the clinical practice guidelines and diagnostic criteria for adult CRS as established by the American Academy of Otolaryngology-Head and Neck Surgery Foundation in 2007.
PHYSICAL EXAMINATION
After confirming a history consistent with CRS, an endoscopic evaluation of the nose and sinuses must be performed to allow the surgeon to document any anatomical abnormalities that may be present (e.g., deviated septum), evaluate the sinus ostia, and determine if there is any polypoid degeneration or purulent exudate evident in the region of the ostiomeatal complex.
Nasal endoscopy allows the surgeon to determine the extent of the disease, which sinuses are involved, as well as the status of the ostiomeatal complex and sinus ostia.
A CT scan examination of the sinuses is indicated if medical therapy has failed and should be obtained prior to any surgical manipulation be it a balloon alone, ESS, or a hybrid procedure.
The CT scan of the sinuses should always include the ability to use surgical navigation should this be necessary.
For balloon use alone, one must be able to access the involved sinus. Consequently, if there is a deviated septum, this may have to be corrected first and would preclude balloon dilatation being performed as an inoffice procedure.
Diffuse nasal polyposis and extensive rhinosinusitis may be a contraindication for balloon use as a standalone procedure but can be used as a hybrid procedure. Furthermore, if the diffuse disease were present in a sinus (e.g., the frontal sinus), the balloon may be used as a frontal sinus seeker to allow the surgeon to gain access into the frontal sinus, dilate the frontal sinus, and then perform ESS on the nasofrontal recess.
Ethmoid sinusitis is a contraindication for balloon use, as it is not indicated for access or surgery within the ethmoid sinus.
Presence of extensive scarring or osteoneogenesis within the frontal recess secondary to prior surgery and long-standing infection can impede cannulation of the frontal sinus outflow tract and preclude the use of the balloon.
CONTRAINDICATIONS
Diffuse nasal polyposis
Complications of sinusitis—orbital or intracranial
Ethmoid sinusitis
Possible neoplastic sinus disease
Markedly deviated septum
Osteoneogenesis
PREOPERATIVE PLANNING
A decision needs to be made as to whether the procedure will be performed in the office or the operating room.
An office-based procedure requires a compliant patient, limited pathology, a septum that is not so deviated that it limits access to the sinus ostia, and appropriate staff and instrumentation.
A documented history of rhinosinusitis, recurrent, acute, or chronic having failed optimal medical therapy.
Endoscopic evaluation to confirm the presence of rhinosinusitis.
CT sinus evaluation—coronal, axial, and sagittal views.
Surgical navigation if necessary.
Lengthy discussion with the patient once medical therapy has failed—discussion will include the risks, benefits, and alternatives.
MRI not necessary unless there is concern about a complication of rhinosinusitis, be it orbital or intracranial, or concern of a neoplasm.
Evidence of complex frontal sinus anatomy (i.e., Type III frontoethmoidal cells) should be noted to avoid inadvertent cannulation of frontoethmoidal or supraorbital cells instead of the true frontal sinus ostium.
SURGICAL TECHNIQUE
The procedure can be done under local or general anesthesia in an operating room, office setting, or rarely an ICU.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree