Toxic and Deficiency Optic Neuropathies
Physicians have known for centuries that the anterior visual pathway is vulnerable to damage from nutritional deficiency and chemicals. The resulting disorders share many signs and symptoms, and several appear to have a multifactorial etiology in which both undernutrition and toxicity play a role. In light of these facts, it is reasonable to group them together. It must be emphasized that evidence for the localization of the primary lesions is lacking in many of the so-called toxic and nutritional optic neuropathies. In some cases, the optic nerve axon is the damaged structure; however, in others, such as the ocular toxicity produced by several of the tumor necrosis factor-alpha (TNF-α) inhibitors and toluene, it is the myelin covering the optic nerves, and the resulting optic neuropathy is due to demyelination. In still other cases, the retinal ganglion cells are damaged directly. In addition, there probably is a genetic component to some of the toxic and nutritional optic neuropathies, which explain why two individuals may be exposed to the same substance or be deficient in a particular nutrient and yet one develops a “toxic” or “nutritional” optic neuropathy and the other does not. The genetic component may be chromosomal, mitochondrial, or both.
Etiologic Criteria
Nutritional Optic Neuropathies
In the Western hemisphere, the most common cause of a nutritional optic neuropathy probably is alcohol abuse leading to a diet lacking crucial nutrients, particularly vitamin B12 and folate. Other settings include malabsorption syndromes, postbariatric surgery, incorrect vegetarianism, and severe depression. In general, nutritional optic neuropathies develop over months rather than days to weeks. Although some patients with nutritional optic neuropathies show evidence of undernutrition, usually manifested in such obvious forms as weight loss and wasting, many do not do so and appear otherwise perfectly well. Thus, signs such as peripheral neuropathy and hearing loss are useful, when present. Unfortunately, they usually are not.
Identifying the specific nutritional deficiency responsible for an optic neuropathy is very difficult. Undernourished individuals are rarely deficient in only one nutrient; multiple deficiencies are the rule. Even if a specific deficiency is identified in a patient with loss of vision, it does not prove that the deficiency caused the visual loss, nor does recovery when the deficient nutrient is resupplied necessarily establish that the resupplied nutrient effected the cure. With the exception of vitamin B12 (which only rarely becomes deficient for dietary reasons), no specific nutrient deficiency has been proved conclusively to cause optic neuropathy in humans. At the present state of knowledge, one can only speculate about which specific deficiencies can cause or contribute to nutritional optic neuropathy.
Toxic Optic Neuropathies
The primary issue in a patient suspected of having a toxic optic neuropathy is whether or not he/she was exposed to a substance that has been proved to damage the optic nerve by the same route of exposure. Visual loss may occur from either acute or chronic intoxication depending upon the agent, and the patient must have symptoms and signs that are consistent with those of a toxic optic neuropathy and typical of those in other patients proved to have suffered loss of vision from the same agent. In most cases, the exposure is via ingestion (e.g., ethambutol), but in some cases the causative agent has been inhaled (e.g., toluene), and in still others implanted (e.g., cobalt-covered prosthesis).
The response of patients to rechallenge is helpful in evaluating the validity of presumed intoxications and in helping to establish the cause of the patient’s optic neuropathy. If a patient who has recovered vision
following cessation of exposure to a drug or chemical loses vision again when reexposed, the recurrent loss of vision tends to verify the neurotoxic nature of the agent and the toxic etiology of the visual loss. Epidemiologic data, especially those showing correlation of changing disease incidence when and where specific drugs or chemicals are introduced or withdrawn, also can prove useful.
following cessation of exposure to a drug or chemical loses vision again when reexposed, the recurrent loss of vision tends to verify the neurotoxic nature of the agent and the toxic etiology of the visual loss. Epidemiologic data, especially those showing correlation of changing disease incidence when and where specific drugs or chemicals are introduced or withdrawn, also can prove useful.
Confirmatory evidence of exposure from laboratory tests or from associated nonvisual symptoms always is desirable although not always possible. Nontoxic disorders must be considered in the diagnosis of these patients and should be ruled out with appropriate investigations. Animal models can help validate the optic nerve toxicity of putative intoxicants, despite such problems as species variation in susceptibility and difficulty in measuring visual function.
Clinical Characteristics of Nutritional and Toxic Optic Neuropathies
Persons of all ages, races, places, and economic strata are vulnerable to the toxic and nutritional optic neuropathies. Certain groups are at higher risk because they are under treatment with drugs, have occupational exposure, or practice habits such as smoking and alcohol consumption. The value of obtaining a thorough history, including dietary intake, exposure to drugs, use of tobacco, and social and occupational background, cannot be overemphasized, and the history must be obtained in an appropriate manner. For example, it is not sufficient to ask the patient if he or she has a normal diet. Rather, one should ask something like “What did you eat for dinner last night?” Depending on the answer, the next question might be “What about the night before that?” or “What about lunch?”
The symptoms and signs of nutritional and toxic optic neuropathy are similar and most closely resemble those of Leber hereditary optic neuropathy (LHON), with the exception of the speed at which vision is lost (see below). Nevertheless, other etiologies, such as primary demyelination and even compression, ischemia, and infiltration must be considered in some cases.
Toxic and nutritional optic neuropathies are not painful. Thus, one should inquire carefully about this symptom because associated ocular or orbital pain suggests some other diagnosis.
Dyschromatopsia is present early and may be the initial symptom in observant patients. Some patients notice that certain colors, such as red, are no longer as bright and vivid as previously. Others experience a general loss of color perception.
Patients with nutritional or toxic optic neuropathies often initially notice a blur, fog, or cloud at the point of fixation, following which the visual acuity progressively declines. The rate of decline can be quite rapid but usually progresses slowly over weeks to months. In most cases, vision decreases to no worse than 20/400, although some substances, such as methanol can cause such severe visual loss that the patient has no light perception in either eye. Nevertheless, in most patients, loss of vision below 20/400 should suggest an etiology other than a nutritional deficiency or a typical toxic process. Bilaterality is the rule, although in the early stages one eye may be affected before the other becomes symptomatic.
Patients with toxic or nutritional optic neuropathies typically have central (Fig. 10.1) or cecocentral (Fig. 10.2) scotomas with sparing of the peripheral visual field (Fig. 10.3). Peripheral constriction and altitudinal visual field loss are rare. Because of the symmetric and bilateral visual impairment in toxic and nutritional optic neuropathies, a relative afferent pupillary defect is not a common finding in affected patients. When the patient is bilaterally blind (e.g., as a consequence of methanol poisoning), the pupillary light response will be absent or weak and the pupils will be dilated; however, in most cases, the pupils have relatively normal responses to light and near stimulation.
In the early stages of nutritional optic neuropathy, the disc is normal or slightly hyperemic. Disc hemorrhages may be present in eyes with hyperemic discs, but they are rare and usually small. Similarly, most patients in the initial stages of toxic optic neuropathy also have normal discs. In both nutritional and toxic optic neuropathies, lack of treatment of the nutritional deficiency or continued exposure to the toxic substance results in the development of bilateral optic disc pallor, particularly temporally, associated with profound thinning or even loss of the retinal nerve fiber layer in the papillomacular bundle (Figs. 10.4 and 10.5).
Differential Diagnosis
When an individual complains of bilateral visual loss that refraction cannot correct and has an otherwise normal examination, there are many diagnostic possibilities in addition to the toxic and nutritional optic neuropathies. Certain maculopathies can present in this guise (see Chapter 2). With time, the fundus will show abnormalities, but until then, optical coherence tomography and/or fluorescein angiography may show structural abnormalities, and multifocal electroretinography will establish the retinal nature of the process.
One always should be alert to the possibility of nonorganic visual loss. The absence of optic disc pallor and retinal nerve fiber layer thinning are important clues when the visual loss is longstanding. In such cases, an OCT of the peripapillary retinal nerve fiber layer is extremely helpful. In addition, whereas the
visual field defects in the toxic and nutritional optic neuropathies are typically central or cecocentral, such defects are exceptional in patients with nonorganic visual loss; in these patients, visual fields usually are constricted (see Chapter 23).
visual field defects in the toxic and nutritional optic neuropathies are typically central or cecocentral, such defects are exceptional in patients with nonorganic visual loss; in these patients, visual fields usually are constricted (see Chapter 23).
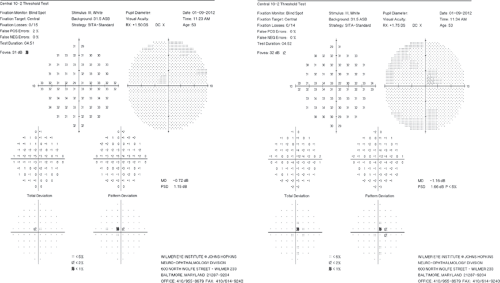 Figure 10.1 Bilateral central scotomas in a 57-year-old woman with a bilateral toxic optic neuropathy from ethambutol. Her visual acuity was 20/70 OU. Peripheral fields were full. |
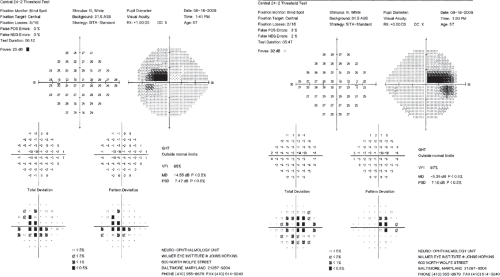 Figure 10.2 Bilateral cecocentral scotomas in a 27-year-old woman with a bilateral nutritional optic neuropathy related to chronic alcohol abuse. Her visual acuity was 20/80 OD and 20/100 OS. |
Dominantly inherited (Kjer) and mitochondrially inherited (Leber) optic neuropathies can be confused with a bilateral nutritional or toxic optic neuropathy if no other family members are known to be affected. The confusion is most likely to occur in patients who




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


