Damage to an optic nerve classically causes an abnormality in visual sensory function, a relative afferent pupillary defect, and, if the damage is irreversible, a change in the appearance of the optic disc. Acquired optic neuropathies can produce any type of visual field defect, including a central scotoma, cecocentral scotoma, arcuate field defect, altitudinal defect, or even a temporal or nasal hemianopic defect. Unless the optic neuropathy is bilateral or the lesion is located near the optic chiasm, the field defect produced by an optic nerve lesion is always monocular.
The visual field defects that occur with various optic neuropathies are not in themselves localizing. Rather, it is the demographics of the patient (age, gender), history of visual loss (rapid vs. slow onset, progressive vs. stable, painful vs. painless), the presence or absence of other neurologic or ocular signs (relative afferent pupillary defect, acquired color deficit, ocular motor paresis, proptosis, optociliary shunt veins, optic disc swelling, optic pallor), and the results of neuroimaging that most often allow the physician to diagnose an optic neuropathy, to localize the pathology along the course of the nerve, and to determine its etiology.
Appearance of the Disc
The optic disc has only two ways to respond to the many acquired pathologic processes that may affect the optic nerve. It can swell, or it can remain normal in appearance. If the pathologic process causes irreversible damage to the optic nerve, the disc will eventually become pale.
Optic Disc Swelling
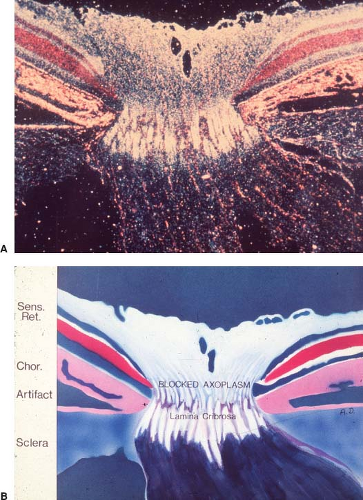
True optic disc swelling of the optic disc occurs when there is obstruction of axonal transport at the lamina cribrosa (Fig. 4.1) and may result from compression, ischemia, inflammation, metabolic dysfunction, or toxic damage (Table 4.1). In some cases, infiltration of the proximal portion of the disc by inflammatory or malignant processes causes an appearance indistinguishable from true swelling. Mimics of true swelling such as congenital disc anomalies are discussed in Chapter 3.
Appearance
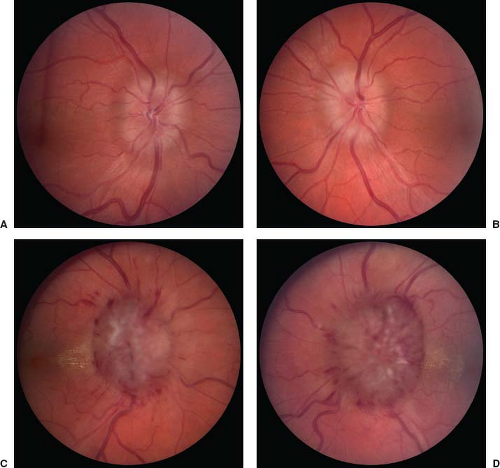
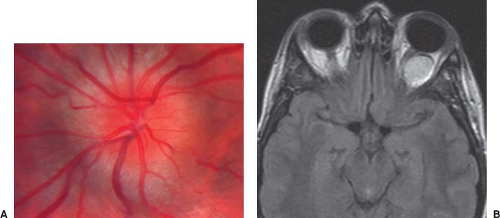
Useful funduscopic signs of early swelling of the optic disc include blurring of the nerve fiber layer around the disc, especially superiorly and inferiorly, and segmental obscuration of small vessels (typically arterioles) as they approach or cross the disc edge (Fig. 4.2A) (see Chapter 5). When disc swelling is fully developed (Fig. 4.2B), additional funduscopic changes can appear, including intraretinal hemorrhages and infarcts (cotton-wool spots) within the nerve fiber layer, hard exudates (sometimes in a star figure around or on the nasal half of the macula), and subhyaloid hemorrhage, occasionally breaking out into the vitreous cavity.
When disc swelling persists for several months or longer, the hemorrhages and exudates tend to resolve, and the initial hyperemia is replaced by a gray or yellow atrophic appearance. Other changes include development of “drusen-like” hard exudates in the superficial substance of the disc itself (Fig. 4.3). Neovascular membranes with subretinal hemorrhages and serous fluid can progressively develop. The peripapillary retinal vasculature may be narrowed with a sheathed quality. Optociliary shunt vessels may also appear on the optic disc, presumably secondary to chronic obstruction of normal retinal venous drainage through the central retinal vein by chronic disc swelling.
Optic disc swelling may not develop if significant optic atrophy is already present: “dead axons can’t
swell.” This is particularly important to remember when the ophthalmoscopic appearance of an atrophic optic disc is being used to determine recurrence or exacerbation of a condition such as raised intracranial pressure (see Chapter 5).
swell.” This is particularly important to remember when the ophthalmoscopic appearance of an atrophic optic disc is being used to determine recurrence or exacerbation of a condition such as raised intracranial pressure (see Chapter 5).
Specific Etiologies
Patients with increased intracranial pressure may develop optic disc swelling. This condition is called papilledema. The symptoms and signs in patients with papilledema generally are those typically associated with raised intracranial pressure, including headache, nausea, vomiting, and pulsatile tinnitus. Visual symptoms in such patients include transient obscurations of vision and diplopia. Loss of central vision, dyschromatopsia, a relative afferent pupillary defect, and visual field defects other than enlargement of the blind spot caused by the swollen disc are uncommon in patients with acute papilledema unless the lesion causing the increased intracranial pressure also directly damages
the visual sensory system in some way, or there are hemorrhages or exudates in the macula. The optic disc swelling in papilledema is usually bilateral and symmetric, but it may be asymmetric or even unilateral. It may be very mild or extremely severe (see Fig. 4.2). Papilledema is discussed in Chapter 5.
the visual sensory system in some way, or there are hemorrhages or exudates in the macula. The optic disc swelling in papilledema is usually bilateral and symmetric, but it may be asymmetric or even unilateral. It may be very mild or extremely severe (see Fig. 4.2). Papilledema is discussed in Chapter 5.
Table 4.1 The Differential Diagnosis of the “Swollen Disc” | ||
|---|---|---|
|
Inflammation of the proximal portion of the optic nerve produces swelling of the optic disc. This condition, called anterior optic neuritis or papillitis, is characterized by relatively acute visual loss, usually in one eye; it is almost always associated with pain around or behind the eye. Eye movement often exacerbates the pain. The appearance of the optic disc ranges from very mild to severe swelling. Vitreous cells may be present, particularly overlying the swollen disc, but peripapillary hemorrhages are rarely seen. In most cases of anterior optic neuritis, vision continues to decline for several hours to several days. It then stabilizes and, after several days to several weeks, begins to improve.
Anterior optic neuritis typically occurs in young adults and is most often caused by demyelination, although it may also develop in patients with a variety of systemic disorders, such as catscratch disease, syphilis, Lyme disease, and sarcoidosis. Patients who develop optic neuritis that is unassociated with a systemic inflammatory or infectious disorder have an increased risk of developing clinical evidence of multiple sclerosis (MS) compared with the normal population.
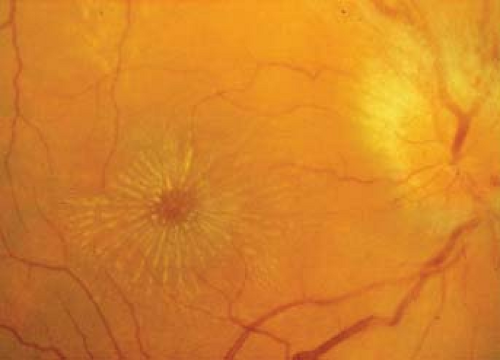
A special form of anterior optic neuritis called neuroretinitis is characterized ophthalmoscopically by optic disc swelling associated with a macular star figure composed of lipid (Fig. 4.4). This form of optic neuritis is almost never caused by demyelination and
occurs most often in the setting of catscratch disease or in association with other systemic infectious diseases, as well as with sarcoidosis. Optic neuritis is discussed in Chapter 6.
occurs most often in the setting of catscratch disease or in association with other systemic infectious diseases, as well as with sarcoidosis. Optic neuritis is discussed in Chapter 6.
Ischemia that affects the laminar or prelaminar portions of the optic nerve produces swelling of the optic disc. This condition, called anterior ischemic optic neuropathy (AION), is characterized by monocular and usually painless visual loss associated with a relative afferent pupillary defect and a visual field defect that is most often altitudinal or arcuate in nature. The loss of vision usually occurs over several hours to several days. It then stabilizes in most cases with only mild recovery if any. AION occurs most often in patients older than 50 years of age who have underlying systemic vasculopathies, particularly diabetes mellitus, systemic hypertension, and giant cell arteritis.
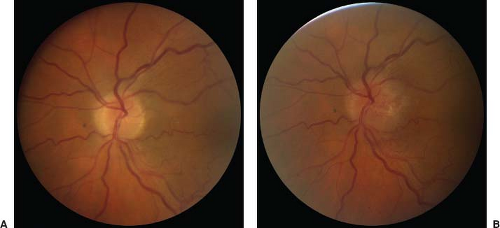
The optic disc swelling that occurs in AION may be hyperemic or pallid (Fig. 4.5) and is usually accompanied by one or more flame-shaped hemorrhages near
the margins of the disc (Fig. 4.6B). Most patients with nonarteritic AION have a congenitally small optic disc with an absent or small central cup (Fig. 4.6A), and this congenital abnormality is thought to be the major predisposing factor for the development of the disorder. Patients with arteritic AION, on the other hand, may have any sized optic disc. AION is discussed in Chapter 7.
the margins of the disc (Fig. 4.6B). Most patients with nonarteritic AION have a congenitally small optic disc with an absent or small central cup (Fig. 4.6A), and this congenital abnormality is thought to be the major predisposing factor for the development of the disorder. Patients with arteritic AION, on the other hand, may have any sized optic disc. AION is discussed in Chapter 7.
 Figure 4.5 Optic disc swelling in anterior ischemic optic neuropathy. A: Hyperemic swelling. B: Pallid swelling. |
Compression of the proximal portion of the optic nerve may produce optic disc swelling. The compression may be caused by a tumor, such as a cavernous hemangioma, meningioma, or schwannoma. In other cases, enlargement of structures normally in the orbit, such as the extraocular muscles in dysthyroid ophthalmopathy, causes optic nerve compression. Patients in whom such compression occurs initially may have no visual complaints and may have few, if any, signs of optic nerve dysfunction other than an enlarged blind spot on visual field testing. Alternatively, they may complain of insidious and slowly progressive visual loss. In such cases, there is invariably some degree of dyschromatopsia, a relative afferent pupillary defect, and a defect in the visual field of the affected eye. The optic disc is generally only mildly to moderately
swollen and hyperemic (Fig. 4.7). Peripapillary hemorrhages are usually absent, but chorioretinal striae are present in some cases, particularly when the compressive lesion is adjacent to the globe. The diagnosis of anterior compressive optic neuropathy is made by neuroimaging of the orbit. Compressive optic neuropathy is discussed in Chapter 8.
swollen and hyperemic (Fig. 4.7). Peripapillary hemorrhages are usually absent, but chorioretinal striae are present in some cases, particularly when the compressive lesion is adjacent to the globe. The diagnosis of anterior compressive optic neuropathy is made by neuroimaging of the orbit. Compressive optic neuropathy is discussed in Chapter 8.
Toxic and metabolic disorders




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree