13
Tinnitus Sound Therapies
Acoustic, or sound, therapy is using external sounds to provide relief from tinnitus. Regardless of which devices are used, the rationale for acoustic therapy remains the same: increase the level of external sounds in the patient’s environment to decrease the patient’s perception of tinnitus. In Fig. 13–1 the tinnitus signal is prominent, and the level of background sound (or noise) is low. There is a large tinnitus signal-to-background noise ratio.
One of the goals of acoustic therapy is to increase the level of background sound to decrease the tinnitus signal-to-noise ratio (as shown in Fig. 13–2). Notice that the amplitude of the tinnitus signal has not changed. Background sound has been increased to make tinnitus less noticeable. By analogy, think of bothersome tinnitus as a candle burning in a dark room. The candle flame seems bright. However, when overhead light fixtures are turned on, the same candle flame becomes much less noticeable than it had been in the dark.
This chapter describes techniques and devices that can help patients to increase their exposure to safe and pleasant external sounds to decrease their awareness of tinnitus. This strategy has multiple advantages and benefits:
• Acoustic therapy is noninvasive and has no adverse side effects.
• Patients often obtain immediate relief from their tinnitus.
• Patients can use external sounds to exert some control over their tinnitus. This often results in reduced patient frustration and anxiety.
• Some patients experience residual inhibition: tinnitus suppression or temporary disappearance following exposure to external sounds.
• Acoustic therapy can facilitate patients’ habituation to tinnitus. That is, increasing the level of external sounds within safe limits can help patients learn to pay less attention to their tinnitus. If tinnitus becomes less noticeable, patients will be bothered by it less often.
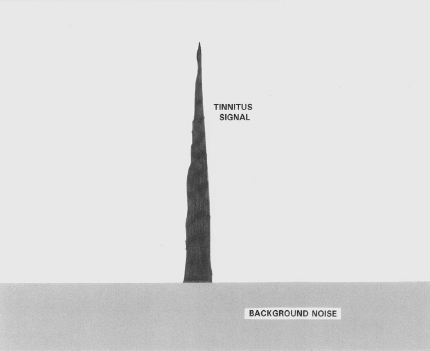
Figure 13–1 Large tinnitus signal-to-background noise.
• Increased exposure to external sounds (within safe limits) can increase blood flow to the inner ear (Quirk et al, 1992). This helps to nourish and maintain auditory structures and may contribute to healing processes.
• Increased exposure to external sounds over time can contribute to reorganizations of neural pathways responsible for tinnitus generation and perception. Altering the pattern of activity within the central auditory system may result in permanent reductions in tinnitus perception.
Acoustic therapy can be a vital component of an effective tinnitus management program. However, to achieve our goal of reducing the severity of each patient’s tinnitus, acoustic therapy should be used in conjunction with other strategies, including
• Medical evaluations and appropriate interventions
• Patient education
• Counseling/psychotherapy
• Lifestyle changes
• Medications as required
Because each tinnitus patient has a unique health, psychological, and social history, therapeutic interventions should be individualized (Hawthorne et al, 1987; Vesterager, 1997). The most successful tinnitus management programs employ multimodal strategies that are designed to address the specific needs of each patient (Folmer, 2002; Sullivan et al, 1994).
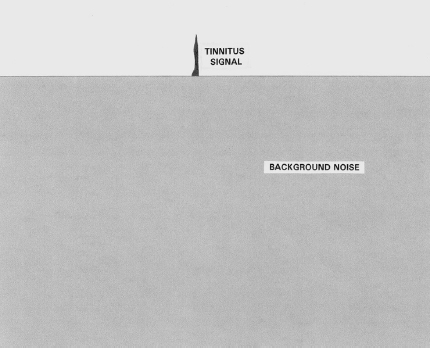
Figure 13–2 Increased background sound in a quiet environment decreases the perception of tinnitus.
Acoustic Therapy Strategies
Environmental Enrichment
Tinnitus is usually more noticeable in quiet environments. That is why we play environmental music in the lobby of our clinic while patients are waiting for their appointment. Most patients say that their tinnitus is less bothersome when they are outdoors walking, working, or recreating. Of course, they have to come inside eventually.
We give this recommendation to every patient: Add pleasant sounds to any environment that is too quiet. Some patients have already figured this out for themselves and routinely turn on a radio or television when they are at home. Unfortunately, this is not always possible away from home, especially at the workplace. Another problem with radio or television is the variability of sounds emanating from these devices: music, talk, commercials, and so on. During the day this variety of sounds may provide a welcome distraction from a patient’s tinnitus. However, if patients want to add sounds to the bedroom to improve their sleeping patterns, we recommend more consistent and less distracting sound sources, such as
Tabletop sound machines Various brands are available that play different types of sounds, such as rain, wind, waterfall, ocean waves, and summer night. Some of these machines also have an input jack for headphones or auxiliary devices such as a pillow speaker.
Cassette tapes and CDs Many different recordings of nature and environmental sounds (e.g., ocean waves, rainforest, summer night) are available. However, some patients are distracted by the sounds of bird calls, crickets, or thunderstorms included in the recordings. For these patients, we recommend compact discs with continuous water or masking sounds with no other sound effects added.
Tabletop water fountains Many types are available in a variety of styles and price ranges.
Fans Some patients turn on a fan to help them sleep. However, some people do not like to feel air circulating in the bedroom all night.
Air purifiers Some patients find that the sound of the fan in an air purifier acts as a masking sound for tinnitus.
Insomnia is a common problem among tinnitus patients (Folmer and Griest, 2000). Improvements in sleep patterns are often associated with reductions in tinnitus severity (Folmer, 2002). Before resorting to medications, adding pleasant sounds to the bedroom is a good way to improve sleep patterns. In addition to the sound generators mentioned previously, we recommend the following sound delivery devices:
Pillows with speakers Regular bedroom pillows with speakers embedded inside can be connected to any sound machine, tape, or CD player that has a stereo jack for headphones. Patients can then play any sort of pleasing or comforting sounds to help them sleep. For many people, delivering these sounds close to the ear is more effective than playing sounds through a machine that sits on top of a nightstand or dresser.
Pillow speakers For people who like to use a particular kind of pillow (or none at all), a pillow speaker can be used instead of a pillow with an embedded speaker. These small, flat speakers plug into a sound machine or tape or CD player and deliver sounds near the patient’s ears.
Headband speakers Originally designed for runners and other athletes, a cloth headband with two small speakers sewn inside the band is another option. The headband plugs into a sound machine or tape or CD player and can be worn to bed. For people who also like to wear a mask while they sleep, the front of the headband can be pulled over their eyes.
Headphones and earpieces Some patients wear these devices to bed and plug them into a sound machine (CD or tape player, radio, television, or tabletop sound generator). However, many patients find headphones or earpieces uncomfortable or impractical when they are trying to sleep.
Delivering sound directly into the ear canal is an efficient way to obtain relief from tinnitus. For this reason, we encourage our patients to listen to comforting sounds through headphones or earphones when possible. Two limitations to these devices are the following: (1) Patients’ movements are restricted because they are attached to the sound machine by a cord. Mobility can be increased by using a portable radio or CD or MP3 player. (2) Headphones and earpieces are conspicuous and are impractical for many people to wear, especially in the workplace. For patients who can afford them, in-the-ear devices are the best alternative.
In-the-Ear Devices
SOUND GENERATORS
In-the-ear (ITE) sound generators (sometimes called “maskers”) deliver broadband sound frequencies (typically 100–8000 Hz) and can provide several immediate benefits for tinnitus patients:
• Sound generators can make tinnitus less noticeable by decreasing the tinnitus signal-to-noise ratio.
• Sound generators can muffle the piercing quality of high-pitched tinnitus, making it more tolerable and easier to ignore.
• Sound generators give patients some control over their tinnitus. Part of the frustration for patients comes from the fact that they cannot escape from their tinnitus, and, if they have not yet employed acoustic therapy, they cannot reduce its loudness.
• Sound generators are the most portable and inconspicuous ways for patients to receive this type of acoustic therapy almost anytime, anywhere.
• Because they deliver sound directly into the ear canal, the devices provide effective acoustic therapy using relatively low levels of sound.
• Some patients report improvement in their ability to concentrate (especially when reading) while wearing sound generators.
• Some patients experience residual inhibition (i.e., tinnitus suppression or temporary disappearance following exposure to external sounds) after using sound generators. Even though residual inhibition is usually brief (30–60 seconds), for some patients it is the first time in years their tinnitus has been absent and they are able to experience silence. For a small number of fortunate patients, residual inhibition can last hours, days, or weeks.
In-the-ear sound generators can also contribute to long-term improvements in tinnitus severity:
• Sound generators can facilitate patients’ habituation to tinnitus. That is, they are tools that can help patients learn to pay less attention to their tinnitus.
• The continuous sound exposure provided by these devices can increase blood flow to the inner ear (Quirk et al, 1992). This helps to nourish and maintain auditory structures and may contribute to healing processes.
• Over time, it is possible that continuous sound exposure provided by in-the-ear devices contributes to reductions in neural activity responsible for tinnitus generation and perception.
It is not necessary—sometimes it is not even possible—to completely mask or cover the patient’s tinnitus with sounds generated by in-the-ear devices. Complete masking of tinnitus is a phenomenon that sometimes occurs as a result of acoustic therapy. However, complete masking is not necessarily the goal unless the patient prefers this type of tinnitus relief. For patients who perceive their tinnitus at relatively low sensation levels (SL) (e.g., 0–2 dB SL), almost any sound delivered to their ears completely masks their tinnitus. We let our patients set the level of sound delivered by in-the-ear devices to obtain maximum relief from tinnitus. We instruct patients to set the level of sound generators to a comfortable, unobtrusive level. We also tell patients not to monitor their sound generators throughout the day. Otherwise, some patients substitute hypervigilance to their tinnitus with hypervigilance to their sound generators. Patients should set the level of sound generators once, then leave them alone and forget about them as much as possible. Sound generators are tools that give patients relief from tinnitus and can help them to pay less attention to tinnitus. We encourage our patients to wear the devices as much as possible during waking hours. Patients sometimes ask the following questions about in-the-ear sound generators.
Q: What if my tinnitus becomes louder? Is it OK to turn up the volume of the sound generators?
A: Yes. Even if most sound generators are turned up all the way, they cannot do physical harm to the auditory system. Most patients do not want or need this level of sound for tinnitus relief. However, they may increase the volume if they so desire. Again, patients should keep the number of volume adjustments per day to a minimum.
Q: What if my tinnitus goes away for a while or becomes so faint that I don’t feel the need to wear my sound generators? Should I still wear them? If I don’t wear them every day, will the habituation process take longer?
A: If a patient does not want or need to wear sound generators for 1 or more days, thatis his or her prerogative. Patients will not necessarily have to use sound generators for the rest of their lives. One of our goals is for patients to eventually be able to ignore their tinnitus most of the time without using any devices. To our knowledge, there is no evidence to indicate that curtailing sound generator use for 1 or more days interferes with the habituation process.
Q: How long will it take for me to habituate to my tinnitus?
A: As long as the patient continues to ask this question, he or she is still monitoring the tinnitus. Some people habituate to tinnitus very quickly. We usually do not see these people in our clinic because their tinnitus is not bothersome and they are not compelled to seek treatment for it. Some patients with bothersome tinnitus seem to believe that habituation is something that will be given to them by a clinician, a device, a medication, or a surgical procedure. In fact, habituation is a set of behaviors that patients must learn to cultivate within themselves. We provide information, tools, and strategies that can facilitate this process. However, patients must take responsibility for their own improvement.
In-the-ear sound generators do not have a good reputation among some clinicians because of the traditionally low success rate and high return rate reported for these devices. Reasons for the low success rate include
• Lack of an integrated, multimodal tinnitus management program. Some clinicians spent a minimal amount of time with each patient, placed sound generators into the patient’s ears, then asked if that was an improvement. This approach has a low likelihood of success.
• Patients were not given the variety of reasons (as described in previous sections of this chapter) for wearing sound generators.
• Complete masking of tinnitus was mistakenly identified as the only goal; when this was not achieved, sound generators were deemed failures.
• Patients did not understand how substituting another sound for their tinnitus was supposed to help them.
• The sounds generated by the devices were described to patients in negative terms, such as “masking noise” and “static.”
To increase the acceptability and perceived benefits of in-the-ear sound generators, we recommend the following:
• Use them as one facet of a multimodal tinnitus management program. In-the-ear devices represent only one type of acoustic therapy. Acoustic therapy is only one component of a comprehensive tinnitus management program.
• If possible, demonstrate in-the-ear devices before patients order them. Give patients time to walk around the clinic while wearing the devices.
• Describe the devices and the sounds they produce in positive terms. For example, if a patient reports that the sound of water running in the shower gives him relief from tinnitus, tell him that the sound generator makes a similar sound. Draw comparisons between the sound produced by the devices and positive experiences with external sounds reported by patients (e.g., with the sound of rain, a waterfall, the ocean, a brook, or the wind). Do not use words such as noise and static because they have negative connotations for many people.
• Thoroughly explain the rationale for recommending a 30-day trial with in-the-ear devices. Explain each of the immediate and long-term reasons for wearing sound generators. Remind patients that complete masking of tinnitus is not always necessary and is not a measure of success.
Criteria for recommending a trial with in-the-ear sound generators:
• Patients with normal or nearly normal hearing who are not candidates for hearing aids
• Otolaryngological exam and clearance by an ear, nose, and throat (ENT) physician
• During the demonstration of these devices, the patient reports that the sound provides some immediate relief from tinnitus
• Patients are interested in using the devices as tools to facilitate improvements in their ability to habituate to tinnitus
• Patients are interested in the possibility of changing patterns of neural activity responsible for tinnitus generation and perception
• Patients with sound hypersensitivity who want to use the devices to desen sitize their auditory system
HEARING AIDS
Hearing aids are another form of acoustic therapy that is usually beneficial for tinnitus patients who also have significant hearing loss. Some patients blame their tinnitus for communication difficulties that are actually caused by hearing loss. This is understandable because hearing loss often progresses slowly over time, and people do not always realize what they have been missing. Tinnitus is the addition of an unpleasant perception that sometimes has a sudden onset. Many patients pay more attention to the addition of tinnitus than to their gradual loss of hearing.
It is important for patients to understand the relationship between hearing loss and tinnitus and to appreciate the differences between hearing loss and tinnitus. We stress the following points with our patients:
• Tinnitus does not cause hearing loss, but hearing loss makes it more likely for a person to hear tinnitus.
• Even if the tinnitus stops completely, patients with significant hearing loss will still have communication difficulties.
• Hearing aids do not amplify tinnitus. In fact, hearing aids usually reduce the loudness of tinnitus by amplifying external sounds.
• Hearing aids improve speech perception for patients with significant hearing loss. This should relieve some of the frustration, isolation, and depression experienced by these patients.
• If hearing could be restored to pretinnitus thresholds, many cases of tinnitus would be cured. At the moment, the most practical way to restore hearing is by using hearing aids.
• Hearing aids are beneficial for the brain of patients with significant hearing loss. If these patients do not stimulate as many parts of their auditory system as possible (at safe levels), the neural pathways are more likely to degenerate.
• Using hearing aids to stimulate the auditory system can contribute to perma nent reductions in neural activity responsible for tinnitus generation and perception.
Some patients are in denial about the extent of their own hearing loss. That is one of the reasons we encourage spouses, significant others, relatives, or friends to accompany patients during their appointment in our clinic and to participate during the interview session. These companions supply important information that would otherwise be missed. The loved ones can also help us to convince resistant patients about the extent of their communication difficulties and associated problems. Some patients require a great deal of encouragement before they are willing to try hearing aids.
Criteria for recommending a trial period with hearing aids:
• Appropriate hearing loss is determined by audiometric testing.
• An otolaryngological exam and clearance are provided by an ENT physician.
• The patient admits communication difficulties.
• During a demonstration of programmable behind-the-ear (BTEs) in the clinic, the patient reports that hearing aids improve his or her hearing sensitivity or reduce the perception of tinnitus or both.
• The patient is willing to pay for the device and to use it regularly.
Fitting tinnitus patients with hearing aids is similar to fitting any patient with a hearing aid. The following factors should be addressed:
• Circuitry (conventional, programmable, digital)
• Style and size (BTE, ITE, completely-in-the-canal [CIC], etc.)
• Cost
• Care and maintenance
Programmable hearing aids give audiologists the opportunity to adjust the pattern of amplification for optimal sound processing and tinnitus relief. For this reason, we recommend programmable digital hearing aids for patients who can afford them.
In order for tinnitus patients to receive maximum benefits from hearing aids, the following strategies should be employed:
• All patients should receive education about the relationship between hearing loss and tinnitus. Understanding this relationship and the mechanisms of tinnitus generation helps patients to put the symptom into perspective. Patients are then less likely to blame tinnitus for communication difficulties resulting from hearing loss.
• The nature of each patient’s hearing loss and its effects on communication and socialization should be identified and discussed in detail.
• All patients should be informed about effective communication strategies that are useful for people with significant hearing loss.
Patients receive multiple benefits from hearing aids, including improved sound localization and identification, improved speech understanding, and reduced tinnitus. Many patients who use hearing aids report reductions in feelings of frustration, social isolation, and depression. Improvements in these areas contribute to reductions in tinnitus severity.
COMBINATION INSTRUMENTS
These devices combine two circuits—hearing aid and sound generator—in one wearable unit. Our criteria for recommending a trial period with combination instruments are the same as our criteria for recommending hearing aids, with one addition: if patients already tried hearing aids and experienced some benefits from amplification, but believe they can receive additional tinnitus relief from a sound generator, a trial period with combination instruments is considered.
PATIENTS WITH ONE “DEAD” EAR
Patients with severe to profound hearing loss and tinnitus in the same ear often present a challenge for clinicians attempting to use acoustic therapy. It is difficult to bring external sounds into the “dead” ear to reduce the patient’s perception of tinnitus. Our advice: try everything. Try the most powerful hearing aid available. Even if it does not improve the patient’s speech discrimination, it may provide some relief from tinnitus. Try an in-the-ear (or behind-the-ear) sound generator or a single ear phone attached to a sound machine. If the sound generator does not work in the dead ear, try it in the opposite ear. Some patients receive tinnitus relief from the contralateral ear thanks to crossover pathways in the central auditory system. If the patient’s better ear could benefit from amplification, try a hearing aid or a combination instrument in that ear. If patients are interested in improving their sound localization abilities, they could try a CROS (contralateral routing of signal), BiCROS, or MultiCROS aid. Another option to consider is a bone anchored hearing aid that is implanted on the affected side of the patient’s head.
Other Devices to Improve Hearing
Any devices or procedures (including cochlear implants, brainstem implants, middle ear amplifiers, and prostheses) that improve patients’ ability to hear external sounds have a good chance of making their tinnitus less noticeable. Future innovations in hearing aid technology, auditory prostheses, and surgical techniques will continue to improve the communication abilities of patients who have significant hearing loss. Many of these innovations will also reduce the loudness of tinnitus for patients who experience this symptom as a result of auditory dysfunction.
COCHLEAR IMPLANTS
Patients with severe to profound bilateral hearing loss usually cannot follow our general recommendation for acoustic therapy, that is, using external sounds to obtain relief from tinnitus. Several studies have reported that cochlear implants reduced or suppressed tinnitus for a majority of patients who experienced tinnitus prior to implantation (Brackmann, 1981; Dauman, 2000; Ito, 1997; McKerrow et al, 1991; Souliere et al, 1992; Tyler and Kelsay, 1990). Cochlear implants are therefore a viable option for some patients who experience tinnitus and bilateral hearing loss of this severity.
Patient Expectations
In most cases, we cannot stop chronic tinnitus that is associated with permanent damage to the auditory system. Before patients arrive for their appointment in our clinic, we inform them in writing that we cannot “cure” their tinnitus. We also remind patients of this fact during their initial interview in the clinic. Adjusting patient expectations into the reasonable range is an important step in the process of reducing tinnitus severity and promoting habituation to the symptom. However, as Tyler et al (2001) suggested, it is also important to provide patients with hope. Even though a cure for most cases of chronic tinnitus is not available now, there are many ways for patients to obtain relief from the symptom. For example, patients can learn to use various forms of acoustic therapy to reduce the severity and intrusiveness of tinnitus. Sound therapy remains our preferred and primary mode of tinnitus management.
Follow-Up
Our patients are encouraged to contact us during business hours if they have questions or concerns. Patients who order in-the-ear devices require follow-up appointments for fittings and adjustments. If we do not hear from them first, we call patients 1 month after their initial appointment in our clinic. Follow-up questionnaires are mailed to patients 6 months and 1 year after their initial appointment. Additional questionnaires are sometimes sent to patients years later.
Regardless of which forms of acoustic therapy a patient uses, clinician-initiated contact at regular intervals after the initial appointment accomplishes several important goals:
• To let patients know that we are committed to helping them
• To address patients’ questions or concerns
• To check patients’ compliance with our recommendations
• To modify recommendations or to suggest different strategies when necessary
• To assess the effectiveness of our tinnitus management program
We remind patients that recommendations made to them at the conclusion of their initial appointment in our clinic are starting points. If a patient follows all of our initial recommendations, yet the severity of his or her tinnitus does not improve over the course of 6 months, we either suggest different strategies or ask the patient to return to our clinic for reevaluation and additional counseling. Different devices and tinnitus management strategies can be described or demonstrated during the follow-up appointment. Particular recommendations will then be reinforced or modified.
Conclusion
All of our tinnitus patients use acoustic therapy in one form or another. Because sound enrichment is just one component of our multimodal tinnitus management program, it is impossible to determine the effectiveness of acoustic therapy alone. However, teaching patients how to use external sounds to reduce their perception of chronic tinnitus usually helps to reduce the severity of their condition.
References
Brackmann DE. Reduction of tinnitus in cochlear-implant patients. J Laryngol Otol Suppl 1981; 4:163–165
Dauman R. Electrical stimulation for tinnitus suppression. In: Tyler RS, ed. Tinnitus Handbook. San Diego: Singular; 2000:377–398
Folmer RL. Long-term reductions in tinnitus severity. BMC Ear Nose and Throat Disorders 2002;2:3. www.biomedcentral.com/1472–6815/2/3
Folmer RL, Griest SE. Tinnitus and insomnia. Am J Otolaryngol 2000;21(5):287–293
Hawthorne MR, Britten SR, O’Connor S, Webber P. The management of a population of tinnitus sufferers in a specialized clinic, III: The evaluation of psychiatric intervention. J Laryngol Otol 1987;101:795–799
Ito J. Tinnitus suppression in cochlear implant patients. Otolaryngol Head Neck Surg 1997;117(6):701–703
McKerrow WS, Schreiner CE, Snyder RL, Merzenich MM, Toner JG. Tinnitus suppression by cochlear implants. Ann Otol Rhinol Laryngol 1991;100:552–558
Quirk WS, Avinash G, Nuttall AL, Miller JM. The influence of loud sound on red blood cell velocity and blood vessel diameter in the cochlea. Hear Res 1992;63(1–2):102–107
Souliere CR, Kileny PR, Zwolan TA, Kemink JL. Tinnitus suppression following cochlear implantation: a multifactorial investigation. Arch Otolaryngol Head Neck Surg 1992;118(12):1291–1297
Sullivan M, Katon W, Russo J, Dobie R, Sakai C. Coping and marital support as correlates of tinnitus disability. Gen Hosp Psychiatry 1994;16:259–266
Tyler R, Haskell G, Preece J, Bergan C. Nurturing patient expectations to enhance the treatment of tinnitus. Semin Hearing 2001;22(1):15–21
Tyler RS, Kelsay D. Advantages and disadvantages reported by some of the better cochlear-implant patients. Am J Otol 1990;11(4):282–289
Vesterager V. Tinnitus: investigation and management. BMJ 1997;314:728–731
< div class='tao-gold-member'>



