10
Tinnitus Retraining Therapy
Tinnitus retraining therapy (TRT) acknowledges that various centers of the brain, particularly the limbic system and the autonomic nervous system, are involved in tinnitus emergence (Jastreboff, 1990). The involvement of these systems is responsible for the annoyance evoked by tinnitus, and the auditory pathways play a secondary role in these processes. TRT is a specific form of sound therapy and counseling (Jastreboff, 2000) that focuses on suppressing negative reactions and associations caused by tinnitus, as well as on suppressing or even eliminating its perception. The directive counseling session and a series of individual follow-up visits facilitate habituation of reaction of tinnitus. Habituation of perception is achieved by means of sound therapy, preferably by wideband noise generators. The application of sound and counseling is dictated by the category of the treatment, basically determined by the patient’s auditory function and responsiveness to sounds.
TRT is not a cure; instead, it allows some tinnitus patients to achieve a condition in which they are not aware of their tinnitus (Jastreboff and Hazell, 1998). In most cases, even though tinnitus is still perceived, it does not induce annoyance and no longer has a negative impact on the patient’s life (Bartnik et al, 1999, 2001a; Jastreboff, 2000). For cases where tinnitus coexists with hyperacusis, TRT is aimed at desensitizing the patient to sound, which results in improving loudness tolerance by decreasing abnormally increased gain within the auditory pathways (Hazell,1995).
TRT is recommended to almost all patients with tinnitus who do not require surgery because of some organic pathology. Patients qualified for TRT have come from various backgrounds, are of different ages, and are from all walks of life (Skarzynski et al, 2000). In each case they are given a thorough audiological evaluation, and in justified cases also a medical examination. The purpose of the diagnosis is to rule out any other medical problems that might contribute to tinnitus and retard habituation. More than 90% of patients in our clinic who qualified for TRT had sensorineural tinnitus. However, we also apply TRT after removing acoustic neuromas and all types of middle ear surgery, including otosclerosis or tympano-sclerosis operations, when tinnitus is still a problem.
Clinical Protocol for Tinnitus Retraining Therapy
We strictly apply all the procedures regarding an established protocol (Jastreboff and Hazell, 1993). The protocol comprises the following:
1. Case history (filling in the initial contact questionnaire)
2. Audiological evaluation
3. Medical evaluation in justified cases
4. Selection of the treatment category
5. Directive counseling
6. Choosing and fitting the most suitable noise generators and hearing aids
7. Follow-up counseling according to the individual needs of the patient and established schedule
Case History
The interview is based on a questionnaire that determines a certain order of the collected data: personal information, work history, the onset of tinnitus and/or hyperacusis and the duration, the location of tinnitus, the assumed (possible) cause of tinnitus and/or hyperacusis, the coexistence of dizziness or vertigo and headache, other illnesses or ailments, medications, the history of ear problems (possible ear infections, surgery, etc.), the exposure to harmful factors such as loud noise, ototoxic drugs, mechanical and chemical injuries, family history, social habits, and usage of stimulants such as coffee, strong tea, and cigarettes (how often and how much).
The information received from the interview is necessary to be able to carry out the directive counseling. All those facts from the case history are useful in explaining to the patient the possible causes of the tinnitus. Sometimes the coexistence of other illnesses or medications may have an influence on the habituation process, which is discussed with the patient.
Audiological Evaluation
The audiological evaluation is an important part of our protocol. It allows us to assess the psychoacoustical parameters of tinnitus and detect the presence of any other disorders in the auditory system. This also allows us to tell patients that their tinnitus does not indicate any serious medical problem in the auditory pathways. In the directive counseling session we always thoroughly discuss the results of all the audiological tests to inform patients of the condition of their auditory system. On the basis of these tests, we can tell patients in greater detail how their middle ear works and the state of their inner ear and auditory nerve. An audiological evaluation consists of the following:
• Pure-tone audiogram for frequencies up to 12 kHz
• Acoustic immittance and acoustic reflexes
• Otoacoustic emission distortion product (to assess and inform the patient about the condition of the outer hair cells in the inner ears)
• Loudness discomfort level for pure tones for 1, 2, 4, and 8 kHz and tinnitus frequency (to assess the level of sound tolerance)
• Special psychoacoustical tests of the characteristics of tinnitus: tinnitus pitch, tinnitus loudness measured for frequency of tinnitus pitch (to assess and explain to patients the psychoacoustical parameters of their tinnitus)
• Threshold of broadband noise and minimal masking level for broadband noise (to be able to discuss with patients the level of broadband noise that is required to mask tinnitus at the beginning of treatment and how it changes during TRT)
• Test of live speech recognition (to assess the condition of the auditory path ways regarding communication)
• Test of auditory brainstem responses (ABRs) for retrocochlear lesion (to determine that there is no pathology at the level of the auditory nerve, especially no acoustic neuroma)
We repeat some of these audiological tests during follow-up visits. Some tests, including the loudness discomfort level and minimal masking level, change during TRT, which shows the progress of therapy.
Medical Evaluation
Some patients qualified for TRT require a medical evaluation to determine if there are any problems related to tinnitus that can influence TRT. If we find such problems (e.g., psychological disturbance, depression, hormonal disorders, illness of circulatory system), the patient needs to be treated simultaneously by specialists in these fields.
Selection of the Treatment Category
On the basis of the interview and some of the audiological tests, the tinnitus patient is assessed using one of five treatment categories (Jastreboff, 2000). The factors determining the appropriate category are the impact of tinnitus on the patient’s life, the presence or absence of hyperacusis, subjective hearing loss, and the presence of prolonged worsening of tinnitus and/or hyperacusis after exposure to moderate or loud sound. “Prolonged effect” means enhancement of tinnitus and/or hyperacusis as a result of noise exposure for several hours or days. The subjective perception of hearing loss takes place when patient subjectively reports problems with hearing in communication.
The separate categories are characterized by the following parameters:
Category 0
• Hyperacusis: absent
• Noise exposure: no prolonged effect
• Subjective hearing loss: absent
In category 0, tinnitus is a limited problem and has little impact on the patient’s life. The directive counseling session and the recommendation to “avoid silence” by using enriched environmental sounds at a level somewhat lower than the tinnitus are often sufficient. This means that every day, the patient must be able to spend substantial amounts of time with environmental sounds just below the level of their mixing point.
Category I
• Hyperacusis: absent
• Noise exposure: no prolonged effect
• Subjective hearing loss: absent
In category I, the patient considers tinnitus a serious problem that affects his or her life. Treatment consists of a directive counseling session, follow-up visits, and a noise generator set at a level close to the mixing point.
Category II
• Hyperacusis: absent
• Noise exposure: no prolonged effect
• Subjective hearing loss: significant
In category II, subjective hearing loss is usually considered the biggest problem, even if the patient shows only a small hearing loss on the audiogram. After directive counseling, we recommend a hearing aid or hearing aid with noise generator in one unit. The aid is needed to improve communication and provide sound therapy. The patient must be able to spend substantial amounts of time during the day using the hearing aid, with the level of environmental sounds set just below the mixing point.
Category III
• Hyperacusis: present
• Noise exposure: no prolonged effect
• Subjective hearing loss: irrelevant or significant
Category III is characterized by significant hyperacusis with or without tinnitus. A noise generator is necessary to help desensitize the hyperacusis. After directive counseling, the patient is told to set the noise generator close to the hearing threshold, and during treatment the level is gradually increased to that of the mixing point. Hyperacusis is always treated first, then tinnitus.
Category IV
• Hyperacusis: present
• Noise exposure: prolonged effect
• Subjective hearing loss: irrelevant or significant
Category IV is tinnitus and/or hyperacusis and prolonged effect of symptoms as a result of sound exposure. This is definitely the most difficult category to treat. In category IV, after directive counseling, the noise generator is set at the hearing threshold, and the level of noise is very gradually increased to the mixing point; however, it is often impossible to use the sound much above the hearing threshold.
The categories of treatment offer general guidelines for directive counseling and the most appropriate approach to sound therapy. These divisions are not strict, and it may be difficult for the clinician to determine whether the patient’s hyperacusis or hearing loss is most problematic and should be the focus of treatment. The most appropriate category can be chosen once a determination has been made regarding the main ailment of the patient.
Directive Counseling
We start with directive counseling (Jastreboff and Hazell, 1998). The counseling session lasts ∼1 hour and is aimed at providing a patient with accurate information about tinnitus: the cause in his or her particular case, where abnormal neuronal activity perceived as tinnitus is generated, and the type of mechanism responsible for tinnitus annoyance. The main purpose is to demystify tinnitus, reassure the patient, and decrease negative associations of tinnitus. Some patients have strong negative beliefs about tinnitus (e.g., tinnitus may intensify to an intolerable level; it may cause hearing loss or even deafness). These fears release negative emotional associations and distress that make habituation impossible. To reassure the patient, we use simple descriptions of the neurophysiological model of tinnitus origin. We modify our way of giving information to the patient to his or her understanding capacities. The first step of directive counseling is explaining the anatomy and physiology of the auditory system. We teach the patient the basic function of the auditory system and the brain in reference to the perception of tinnitus.
ANATOMY AND PHYSIOLOGY
At the beginning of the counseling session discuss the basic structure of the ear. In order for the patient to understand it better, we use some diagrams of the ear and the hearing pathways. We describe the function of the auditory system, explaining sound changing into electrical impulses. We indicate that inner hair cells (IHCs) are responsible for initiating impulses, whereas outer hair cells (OHCs) are responsible for fine-tuning sounds by enhancing weak signals and attenuating loud signals. We tell the patient that the OHC system is controlled by the brain, and that OHCs are vulnerable to damage by viral infections, noise, stress, ototoxic drugs, mechanical trauma, and other disorders. In addition, we lose ∼0.5% of OHCs per year as a result of aging. We show the patient photos of normal and damaged outer and inner hair cells, indicating that usually the OHCs are damaged first, whereas the IHCs are more resistant to injury.
We tell the patient about the phenomenon of frequency specificity that takes place in hair cells on the basilar membrane and in auditory nervous pathways as well. We say that, depending on the place of a lesion, the damage of OHCs will change the mechanical properties of the Corti organ, and consequently abnormal patterns of neuronal impulses can be generated from that place (Jastreboff, 1990).
GENERATION OF ABNORMAL NEURAL ACTIVITY PERCEIVED AS TINNITUS
We inform the patient that there is a high level of random spontaneous activity in the auditory nervous pathways. This activity is normally interpreted as a “silence” and is filtered out at the subcortical levels without being perceived in the cerebral cortex. Consequently, we cannot hear this activity as a sound.
Next, we explain to the patient how the brain handles the information conveyed in neuronal impulses. We say that each change of the spontaneous activity caused by a pathology in any place of the hearing pathways can be detected from the background by subcortical centers. The neural system has particularly sensitive mechanisms of detecting new signals that have never been experienced. There are a few subcortical levels of the brain that detect the signals at the subconscious level. They are responsible for filtering, enhancing, and prioritizing the signals before they are sent to the cortex and we become aware of them.
We mention some possible places of tinnitus generation in the auditory system, and we repeat that in the majority of cases, tinnitus is clearly related to some changes in the inner ear. At the same time tinnitus is not necessarily associated with hearing loss. We share the information with the patient that ∼30% of those who suffer from tinnitus do not have any hearing difficulty, and also that many people with hearing loss or even with total deafness do not have tinnitus.
We suggest to the patient that it is discordant damage of the OHC and IHC system that results in the generation of abnormal neuronal activity (Jastreboff, 1990). This can be responsible for initiating a series of processes that lead to the perception of tinnitus. This hypothesis is very useful to help understand the mechanism by which tinnitus is triggered in cases with normal hearing and with hearing loss as well. We repeat that this abnormal neural activity is not tinnitus yet. It is usually a weak signal that is amplified on its way from the ear to the auditory cortex.
RESULTS OF THE PATIENT’S AUDIOLOGICAL TESTS
It is essential to familiarize patients with the results of the audiological tests to explain what is happening in their hearing system. We discuss the results to explain to them where a possible pathology responsible for generation of changed neuronal activity (perceived as tinnitus) occurs. The results of the audiological tests let us tell patients the condition of different parts of their auditory system, and they let us eliminate some of the negative beliefs (e.g., tinnitus is connected with a serious pathology in the ear or auditory pathways). We discuss the meaning of hearing threshold, impedance audiometry, and speech recognition, as well as minimal masking level and loudness discomfort level, which are especially important in monitoring the process of habituation.
The tests of characterization of tinnitus, such as loudness, pitch, and minimal masking level, are also discussed. We emphasize to the patient that tinnitus is usually a weak signal. The level of a pure tone equal in loudness to tinnitus is most often <10 dB sensation level, even if the patient complains of very loud tinnitus. It is not uncommon for our patients to perform a loudness balance at or near their threshold. In such patients it is easy to confirm that tinnitus is a phantom perception of neuronal activity, and it can never be compared with a real, external sound.
We explain that peripheral hearing loss exerts a strong influence on the perceived pitch of tinnitus because most often tinnitus pitch is located in the range of frequencies in the slope of the audiogram (Hazell, 1995; Meikle, 1995). Next, we evaluate distortion products otoacoustic emission (DPOAE). It indicates functional integrity of outer hair cells, and for almost all of our patients it shows cochlear dysfunction in a frequency region corresponding to their perceived tinnitus, even in patients with normal hearing (Bartnik et al, 2002; Hall, 1999; Shiomi et al, 1997). This information is invaluable in counseling patients about the origin of their tinnitus. The observation of a decrease in DPOAE amplitude in some frequency regions in patients with normal hearing fits exactly in the hypothesis of discordant damage of OHCs and IHCs (Jastreboff, 1990). The information gained from DPOAE can also be useful in convincing patients that their problem is real (Hall, 1999).
Finally, we explain to patients the result of the ABR latency test. This allows us to tell them that there are no retrocochlear lesions in their auditory pathways. Many patients are afraid of tumors, so this information makes them feel much calmer.
HOW DOES THE DETECTION OF ABNORMAL NEURONAL ACTIVITY RELATE TO TINNITUS?
After the first part of our consultation, we tell the patient that each incorrect pattern of neuronal activity is easy to notice from the background of spontaneous activity. Consequently, this signal may not be filtered, and it can reach the cerebral cortex. This is the case when tinnitus is perceived. We explain to the patient that our brain sorts out signals according to their significance, giving important signals priority. Of particular importance are signals that are new, associated with emotional or unpleasant situations, related to survival, or a threat to health or life. Tinnitus meets such conditions, most often posing a threat to the quality of life. That is why people focus their attention on it.
We indicate to the patient that tinnitus is usually associated with negative emotions. It causes fear of hearing deterioration, brain tumor, burst blood vessel in the brain, psychological disorders, and so on. In addition, people cannot free themselves from this sensation, and very often the patient cannot find any effective help for it. On the contrary, health care professionals often offer the patient negative counseling, such as “Nothing can be done for tinnitus” and “You have to learn to live with it,” which makes the patient’s beliefs and concerns stronger. We explain to the patient that when this signal is labeled as something wrong or negative, the activation of the limbic system and autonomic nervous system increases. The signal of tinnitus is qualified as one of the most important tasks the brain needs to attend to. This results in enhanced awareness of this signal, which triggers the increase of tinnitus intrusiveness and annoyance. We emphasize very clearly that the degree of annoyance depends on activation of the limbic system and autonomic nervous system. To stress this, we discuss the patient’s parameters of tinnitus, indicating that the value of tinnitus loudness is usually very close to the hearing threshold, although it may be perceived as a very loud sound. We make the patient aware of a difference between someone who experiences tinnitus and someone who suffers from it.
At this time we summarize information, by answering the following questions.
Q: Where is the most probable place of tinnitus generation in the patient’s particular case?
A: Most often we can indicate that dysfunction in the inner ear or damage to the outer hair cells is responsible for tinnitus generation.
Q: What causes tinnitus?
A: It results from the brain over compensating (overreacting) to the presence of even a small abnormal activity in the auditory nerve. Tinnitus is not a sound; it is the perception of neuronal activity.
Q: Why can tinnitus be so troublesome?
A: The degree of tinnitus annoyance depends on the brain’s interpretation of it, and successive activation of the brain’s systems responsible for emotions and reaction of the body.
Q: What are the main goals of directive counseling?
A: To reassure the patient and decrease his or her negative reactions to tinnitus. Directive counseling seeks to neutralize the negative emotional associations and fears caused by tinnitus.
Q: How can this education help the patient?
A: Education helps because understanding the causes and effects of tinnitus makes it less frightening. Most often tinnitus is a symptom of some disorder in the inner ear, and it is not connected with any serious disease.
Q: What is the next step in therapy?
A: The next step is to initiate the process of habituation, to retrain the emotional and autonomic system to not be activated by tinnitus.
After the first part of counseling, patients usually feel much calmer and more secure. We then tell them that even if they accept that tinnitus does not threaten health or create any harm, the tinnitus will still be perceived. They may not be annoyed by tinnitus so much, but they can still hear it. Consequently, we explain to patients that our next goal is habituating the tinnitus perception.
HOW DOES THE SENSORY SYSTEM OPERATE, AND WHAT RESULTS FROM THIS?
We provide an overview about the regulation of our sensory system. We tell the patient that our sensory system works on detection and enhancement of contrast, and at the same time it adjusts amplification of incoming signals depending on their characteristics. In practical terms this means that the bigger the contrast with the environment, the easier the perception of the signal. For example, a small candle is a big stimulus for our vision in a dark background, whereas the same candle may go unnoticed in the daylight. We give similar examples here concerning different sensory subsystems to show the patient that the absolute strength of a physical stimulus is less important than its contrast against the background. It is easy for the patient to understand that the weak sound will be perceived clearly when there is no other sound around (a big contrast with the environment). According to this, a tinnitus-related signal coming from the inner ear will be easy to detect if the patient is in silence. At the same time, if there are no sounds around us, the brain will try to get any kind of information from the ear. In these cases, the central auditory system will strengthen every neuronal activity related to tinnitus. We talk about an experiment in which young people with normal hearing and without tinnitus started to perceive tinnitus while being in an anechoic chamber (an almost totally silent and echo-free room). We explain to the patient what happened in that situation. We tell the patient that all of us could potentially hear tinnitus if we were in an environment quiet enough, as a result of increased gain in the auditory pathways by the brain. This also can lead to hyperacusis, which can reach an extremely high level so that the patient cannot tolerate normal everyday sounds. In the case of hearing loss, the gain in the central auditory pathways will increase in exactly the same way as with somebody remaining in a soundproof room.
Therefore, taking into consideration all these facts, our first goal will be to decrease gain within the auditory pathways. After increasing the level of acoustical background of the surroundings, tinnitus is supposed to merge with the background. At this point we hope the tinnitus ceases to be noticeable. Next, we discuss the ways we can facilitate this.
WHAT SPECIFIC APPROACH TO SOUND THERAPY DO WE TAKE?
We tell the patient that, because it is pivotal that each signal in the central nervous system is detected on the basis of contrast, we have to decrease the contrast between neuronal activity perceived as tinnitus and general background activity within the auditory system. This will reduce or even remove the tinnitus. According to this, the sound serves the purpose of reducing the contrast in hearing pathways between the tinnitus signal and the background sound. We tell the patient very clearly that he or she should not create the situation where the tinnitus signal is the only stimulus. Thus a strong emphasis is placed on the recommendation to “avoid silence.” What matters is the existence of the sound, not the source of it. It is important for the sound used during the training to be neutral (not to attract the patient’s attention) and set at the level below the mixing point. The sound may be produced by various devices such as an air-conditioner, radio, cassettes, and bedside sound generators. We make patients aware that they cannot habituate to something they cannot perceive. Consequently, complete masking of the tinnitus is prohibited. At the same time we remind patients to avoid loud sounds because the association between a loud noise and tinnitus has been known for many years.
We use Fig. 10–1A,B,C to teach patients the relation of the tinnitus signal to the acoustic background.
We indicate that patients should create a situation similar to that in Fig. 10–1C. We tell patients about the best way to decrease the contrast between tinnitus signal and background activity. This acoustic situation can “turn down tinnitus” after some time for patients in each category (Bartnik et al, 2001a). We finish directive counseling by explaining to patients the importance of enhancing the natural process of habituation, then decide on the best kind of devices for TRT sound therapy.
The next visit is arranged for fitting a hearing aid or noise generator.
Choosing and Fitting the Most Suitable Hearing Aid, Hearing Aid with Noise Generator, or Noise Generator
Patients from category II, who have subjective hearing loss that creates communication problems, are advised to use hearing aids with noise generators. If for some reason that is impossible, we recommend just hearing aids. From the beginning the patient is instructed that the hearing aido provides an additional auditory signal to facilitate habituation during the day and to improve communication when it is needed. The hearing should improve immediately using a hearing aid, but it takes time to reduce tinnitus (Bartnik et al, 2001a). We explain to the patient that hearing loss reduces the sounds reaching the ear, and tinnitus comes to the foreground as a distinctive signal in hearing pathways. We repeat to the patient that a hearing aid can be used for two reasons: to improve the conditions for communication and to amplify the everyday noises that the patient has not been able to hear. If the environment is quiet, then it is necessary to add some sounds for the hearing aid to amplify, but always to the level below the mixing point. Using a hearing aid for communication usually reduces stress connected with hearing difficulties. Specific times listening to constant-level sounds just below the mixing point is recommended.
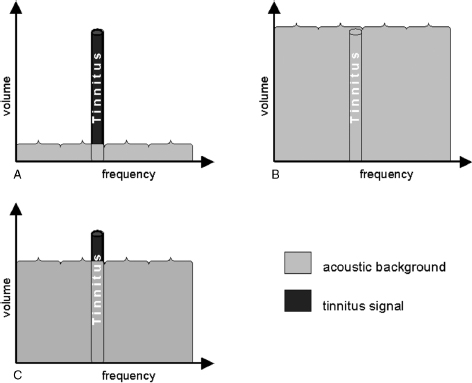
Figure 10–1 Tinnitus under different acoustic conditions. (A) Tinnitus in quiet environment. (B) Tinnitus masked by high level of noise. (C) Tinnitus signal against the background of low-level noise.
For patients from category I, III, and IV we advise using noise generators, generally on both ears. In the case of coexistence of hyperacusis and tinnitus, the therapy always starts with the hyperacusis. In the case of coexisting hyperacusis and hearing loss, we begin treatment of hyperacusis using noise generators. Using a low-level noise generator is a comfortable way of providing sound that decreases gain within the auditory pathway. We emphasize that noise from generators should never mask the patient’s own tinnitus. It should always be set at the level between the hearing threshold and the mixing point. In category I, the sound from noise generators can be very close to the mixing point from the beginning. This situation is shown in Fig. 10–1C.
We always use open ear molds to avoid isolating ears from surroundings.
For category I patients:
• We adjust the volume to the mixing point and tell the patient that he or she has to be able to separate tinnitus from the sound of the instrument at the moment of fitting.
• We demonstrate to the patient how to set the generator very close to the mixing point in each ear.
• We explain how to use a noise generator, turn it on and off, and set the volume.
• We advise the patient to use the noise generator as much as possible (minimum 8 hours a day, preferably throughout the day).
• We tell the patient to put on the noise generator upon waking every morning.
• The instrument must be taken off at night, but the patient should have some other soft sound around the bed during the night.
• The patient is told to set the instrument at the mixing point and not to change the sound level even if he or she cannot hear the sound from the instrument because of another environmental noise. If tinnitus gets louder during the day, after the patient has set the noise generator, he or she should not increase the volume.
• The patient is told that the tinnitus may appear to worsen after he or she has worn the noise generator for a few weeks. This is only a temporary experience, however, and the patient should not worry about it.
• We repeat the recommendation to “avoid silence.” Low levels of background sound (below the mixing point) are recommended.
For category III and IV patients:
• We ask the patient to tell us when he or she begins to hear noise from the generator. For category IV patients, we set the volume at the hearing threshold; for category III patients, we adjust the volume slightly above that point.
• We ask the patient to repeat this activity for both ears because sometimes the level of noise can be a little different in each ear.
• We recommend that the patient not wear ear protection if he or she is used to wearing it; instead, ear protection should be worn only when the patient is exposed to loud noise.
• The rest of the fitting protocol includes the same recommendations as for patients from category I.
Follow-up Counseling According to Individual Needs of the Patient and Established Schedule
After providing the patient with hearing instruments, it is important to monitor the therapy. Category III and IV patients usually need to be seen more often.
On average we follow the following schedule of appointments.
4-week appointment
• Check if the patient is wearing the instrument(s) properly (volume setting, comfort of using, period of use).
• Listen to the patient’s questions and concerns and try to resolve them.
• Reinforce goals.
3- and 6-month appointments
• Check volume setting, time period of use, and comfort.
• Category III and IV patients may be asked to gradually increase the volume to the mixing point.
• Ask the patient if he or she has ever forgotten about the noise generator (indicates that habituation of the sound from the instrument has begun).
• Review counseling.
• Listen to the patient’s questions and concerns and try to resolve them.
• Reinforce goals.
12- and 18-month appointments
• Check volume setting, time period of use, and comfort.
• Change volume setting to the mixing point for category III and IV patients if the patients wear noise generators comfortably for most of the day.
• Assess subjective aspects of hyperacusis in category III and IV patients and observe if hyperacusis has ceased to be a problem.
• Repeat counseling.
• Listen to the patient’s questions and concerns and try to resolve them.
Usually after 24 months of therapy we let patients stop wearing the noise generators if they have shown that they do not need them anymore. In some cases patients do not want to part with the noise generators, and they are allowed to continue wearing them. Some are ready to live without generators only in the third year of therapy.
Conclusion
In our opinion, tinnitus retraining therapy has many advantages, including the fact that it is completely noninvasive. Following therapy, we have observed changes in tinnitus reaction, in tinnitus awareness, and in the particular life activities previously prevented or affected.
We realize that tinnitus retraining therapy has some weaknesses as well. It is time consuming in that it takes about 18 months for stable effects to become obvious. In addition, some patients do not get satisfactory results after this long period of treatment. TRT requires some patience and discipline from the patient and well-educated, experienced professionals to conduct it properly.
Acknowledgments
We would like to thank Professor Pawel Jastreboff and Dr. Margaret Jastreboff for introducing us to tinnitus retraining therapy.
References
Bartnik G, Fabijanska A, Rogowski M. Effects of tinnitus retraining therapy for patients with tinnitus and subjective hearing loss versus tinnitus only: proceedings of the 4th European Conference on Audiology. Scand Audiol Suppl 2001 a;52:206–208
Bartnik G, Fabijanska A, Rogowski M. Experiences in the treatment of patients with tinnitus and/or hyperacusis using the habituation method. Scand Audiol Suppl 2001b;52:187–190
Bartnik G, Fabijanska A, Rogowski M. Our experience in treatment of patients with tinnitus and/or hyperacusis using the habituation method. In: Hazel J, ed. Proceedings of the Sixth International Tinnitus Seminar. London: Tinnitus and Hyperacusis Centre; 1999:567–569
Bartnik G, Rogowski M, Fabijanska A, Raj-Koziak D, Borawska B. DPOAE assessment of cochlear function in tinnitus patients with normal hearing. In: Patuzzi R, ed. Proceedings of the Seventh International Tinnitus Seminar. Fremantle, Australia, University of Western Australia. March 5–9, 2002:45–47
Hall JW III, ed. Handbook of Otoacoustic Emissions. San Diego: Singular; 1999:104–139, 530–539
Hazell JW. Models of tinnitus: generation, perception, clinical implications. In: Vernon J, Møller A, eds. Mechanisms of Tinnitus. Boston: Allyn & Bacon; 1995:57–69
Jastreboff PJ. Phantom auditory perception (tinnitus): mechanisms of generation and perception. Neurosci Res 1990;8:221–254
Jastreboff PJ. Tinnitus habituation therapy (THT) and tinnitus retraining therapy (TRT). In: Tyler R, ed. Tinnitus Handbook. San Diego: Singular Thomson Learning; 2000:357–376
Jastreboff PJ, Hazell JWP. A neurophysiological approach to tinnitus: clinical implications. Br J Audiol 1993;27:7–17
Jastreboff PJ, Hazell JWP. Treatment of tinnitus based on a neurophysiological model. In: Vernon J, ed. Tinnitus: Treatment and Relief. Boston: Allyn & Bacon; 1998:201–216
Meikle MB. The interaction of central and peripheral mechanisms in tinnitus. In: Vernon J, Møller A, eds. Mechanisms of Tinnitus. Boston: Allyn & Bacon; 1995:181–206
Shiomi Y, Tsuji J, Naito Y, Fujiki N, Yamamoto N. Characteristics of DPOAE audiogram in tinnitus patients. Hear Res 1997;108(1–2):83–88
Skarzynski H, Rogowski M, Bartnik G, Fabijanska A. Organization of tinnitus management in Poland. Acta Otolaryngol 2000;120:225–226
< div class='tao-gold-member'>



