15
Tinnitus Person-Centered Therapy
Two blind mice fell into a bucket filled with milk. Neither of them knew how to swim. Then one of them thought: I don’t know how to swim. Thus it drowned. The other one thought: I’ll have to find a way to survive. Then the mouse started whipping its feet in order to keep its head above the surface of the milk. The next morning the mouse, to its surprise, sat on a lump of butter.
Tinnitus can be a most intruding and disturbing experience. Fortunately, most persons become accustomed to it. A small percentage of individuals, however, are continuously and severely bothered by the sound influencing all aspects of their life. Through our psychological work with persons suffering from tinnitus, we have found that sometimes this suffering coexists with other “whole life” personal problems or factors enhancing the annoying influence of the tinnitus. It is difficult to help such patients in the traditional way (i.e., informational counseling and sound therapy). They do not have a psychiatric disorder that can explain the suffering (depression, anxiety disorder).
This protocol is founded on the point of view that for such persons, tinnitus has to be understood as providing important information about the way the person approaches the problems, challenges, and dilemmas in his or her life. The person has to clarify the relevance of this information and then, if possible, take a stand on it. This, however, demands that the focus of treatment is displaced from tinnitus alone to the person as a whole; that is, the person’s relation to himself or herself (including tinnitus) and to others: family life, social life, work life; the individual’s spiritual life, including thoughts of life being time limited; value system: social norms, norms of behavior, moral standards, and ethics. In other words, in these cases as much information as possible has to be obtained about the person to clarify whether there exists a connection between the suffering from tinnitus and the way the person with tinnitus approaches life.
It is our experience that the framework of existential therapies, which center around the person and how they relate to all aspects of life, has particular relevance to the treatment of tinnitus. Existential therapy is “a rich tapestry of intersecting therapeutic practices, all of which orientate themselves around a shared concern: human lived existence”. (Walsh and McElwain, 2002:254, in Cooper, 2004). In this chapter, we explain our own specific application of existential psychotherapies to tinnitus patients, which we refer to as “Tinnitus Person-Centered Therapy.”
The therapist using the framework of the tinnitus person-centered therapy will work in the direction of encouraging the person to examine whether a meaningful perspective could be attached to tinnitus rather than trying to teach the client principles of attention, habituation, or coping strategies. Hence the objectives of therapy will be to support the client to understand, learn from, and integrate tinnitus into his or her life. The person owns the tinnitus instead of being owned (victimized) by it.
The aim of this protocol is to introduce some of the concepts from the framework of the existential therapies that we find useful in our work with clients suffering from tinnitus as well as to outline our method of gathering overall oriented information about the client. We also provide an example of how we work using the framework of person-centered therapies.
Who Can Benefit from Person-Centered Therapy?
Many people let their life be conducted by attitudes, assumptions, demands, and expectations (to themselves as well as to their surroundings), standards (of society) that they unknowingly have applied to life. These elements work like a kind of underlying demanding automatic operating system, bossing the client around and making him or her work very hard in all aspects of life. Such dutiful people often use expressions like “one should,” “one ought to,” “one has to,” and “nothing one can do about it.” An example is the mother dragging herself through watching all the games that her son is playing because she thinks that this is “how a good mother is supposed to be.” Another is the home-maker who wants things done in her own way working very hard every day to satisfy what she believes is the needs of the rest of the household. She is demanding that her husband support her and feels very angry or disappointed when he doesn’t notice all her work or doesn’t help her the way she wants him to. Often this leads to problems between the husband and wife. Another example is the boss who is the first to arrive at the office in the morning and the last one to leave in the evening because he thinks that is how “one sets a good example to the employees.” Such people may seem active and engaged, but their way of living often makes them feel very stressed. However, they actually are exerting a kind of passiveness toward life. They do what they always have done without ever challenging these automatic ways of being by, for instance, posing this question: Might there be other and more rewarding ways of being in life?
At some point in the client’s busy life tinnitus either starts or is enhanced. The client becomes scared or even terrified. In his or her search for the tinnitus cure, a new career begins: the one of becoming a helpless and help-seeking patient suffering from tinnitus. The problem is that nothing really helps and that tinnitus just continues ringing or buzzing. Therefore, the client feels stuck. Depression may develop. Hence tinnitus is felt to be a powerful enemy that hinders the client in coming back to living the familiar life.
What the client disregards or perhaps only vaguely senses is that the demands of the underlying self-imposed automatic system simply have exceeded his or her ability to continuously fulfill them. As a consequence, one way to understand the impact of tinnitus is that it is a warning signal telling the client that the way he or she lives is too exhausting and stressful (assuming that such a person enters therapy, we now use the term client), that it may even be dangerous to go on living the way the person does, and that new ways of being in life have to be discovered.
Elisabeth is a 24-year-old anthropology student. She lives at a dormitory in Copenhagen but is often staying at her parents’ house in the countryside, enjoying their company as well as the wonderful surroundings of nature. She has a good and close relationship with her parents. She doesn’t have a boyfriend because the studies are taking up almost all her time. She has had tinnitus since age 16 (due to fireworks). After some difficulties she is making an effort to learn to live with it. For some unknown reason tinnitus now has worsened. Nothing has been found that can explain this aggravation. However Elisabeth is very influenced by her new situation. She is unable to study. She divides the days into good days (when tinnitus is not annoying) and bad days (when tinnitus is annoying and disturbing). Presently she mostly experiences bad days. On these days she goes to her parent’s house, lies in her old bed, crying. The parents are very concerned, trying to support and comfort her.
The Integrating Concepts in Person-Centered Therapy
When working in the framework of the existential therapies, therapy is understood as a humane meeting between two persons talking about the personal situation of one of them with a special reference to his or her problems, dilemmas, and potential choices (Jacobsen, 1998). The therapist is providing a warm, honest, and respectful relationship to the client, thus establishing a relationship of trust. While at the same time validating and respecting the client’s experience and way of living his or her life, the client is encouraged to investigate/study that life: choices, attitudes, assumptions, relations to himself or herself, symptoms like tinnitus, and other issues.
The overall objective of existential therapies is to help clients become more authentic (“writers of their own life”; van Deurzen, 1997, 2002). This includes becoming aware of their actual existence and to live more in accordance with their true values, beliefs, and experiences—in the context of given possibilities and limitations (Cooper, 2004; van Deurzen, 1997, 2002).
During the therapeutic process, the person-centered therapist’s work continuously shifts between
1. Entering the client’s world, thus being in the position of being-with-the-client
2. Exiting the client’s world, thus being in the position of being-for-the-client
When being-with-the-client, the therapist, together with the client, is a co-student of the way the client exists in life. The therapist tries “entering the world” of the client, thus, metaphorically speaking, being under the client’s skin and looking through his or her eyes at the client’s lived world. The therapist is naive in a disciplined way (Yalom, 1980) and brackets all his or her professionalism and knowledge as well as assumptions and prejudices—whatever the client says or utters is new to the therapist and has to be clarified, whenever needed. The aim of the therapist is to grasp the experience of being the client as fully as possible.
When being-for-the-client, the therapist’s position is one of being a human being meeting with another human being. In this position the therapist’s educational background as a psychologist also is present as well as the therapist’s own experiences and thoughts on the given theme or topic. During the therapeutic process, the existential working therapist shifts between blank slate and being genuine and direct (in a gentle way). The method of the therapist being a “blank slate” is used in other therapeutic directions, making the therapist as neutral as possible. The therapist often starts off by mirroring back what he or she so far has grasped from the study of the client’s life:
Elisabeth: The best place for me to be on my bad days is at my parent’s house. Here I can be myself.
Therapist: So being at your parent’s house allows you to be yourself with your suffering.
This process of mirroring is exerted to ensure that the therapist really has grasped what it is about, or to make the client really listen to and wonder about what the client actually has just said. Sometimes having repeated/mirrored what has been said makes the client examine further whether he or she really means what was actually just uttered. This mirroring can lead to new thoughts or comments from the client that need further clarification (back to step 1), or the mirroring can be followed by an attempt from the therapist to shed light on what may be a different or new, but hopefully more constructive, way of looking at the problem experienced by the client (which would be too early in the present example). Alternatively, the therapist may encourage the client to take a stand on the theme; that is, discuss or give back to the client the therapist’s own thoughts on the theme.
The most important tool that we use to investigate the lived experience of the client as thoroughly as possible is the phenomenological method of investigation (Spinelli, 2000). This method is composed of three rules:
1. Bracketing. The therapist continuously brackets all his or her “initial biases and prejudices of things, suspending his [or her] expectations and assumptions” (Spinelli, 1989) to be as open-minded as possible toward whatever the client may bring instead of immediately judging, taking a stand on, giving professional advice, or interpreting the client’s experience. The aim is to make the therapist able to grasp as clearly as possible what the client is experiencing—to see and feel what the client is feeling. This rule is very difficult to observe. Assumptions, theories, and knowledge will keep intruding. Just stop for a while and try to reconstruct your own thoughts (assumptions) when reading this sentence from the case study: “ The best place for me to be on my bad days is at my parent’s house. Here I can be myself.” Now try to bracket your assumptions. Which questions would you pose to clarify the client’s intent further? The difficult challenge for the professional wanting to use the phenomenological method of investigation is to be aware of all assumptions while trying to grasp the world of the client.
2. Description. The second rule can be summarized as “Describe, don’t explain” (Spinelli, 2000). Instead of discussing, for instance, what clients have read or heard of the physiology of tinnitus, they are encouraged to describe all the different situations in which tinnitus is annoying them, how it annoys them, and how they then react. This rule can be very difficult to keep. Basically, it is about listening while keeping clients on the right track of describing, thus guiding them away from their own attempts at speculation and assumption. If you are interested in trying out this rule, ask someone to describe a headache and how it influenced that person’s day. Your role is only to ask questions elucidating details that will keep the person on topic. Only pose questions when needed, otherwise keep silent while nodding in a confirmative way, thus encouraging the person to speak.
3. Horizontalization. The rule of horizontalization is meant to help the therapist not “making immediate misleading hierarchically based judgments” (Spinelli, 1989) that may lead to wrong conclusions. Whatever the client brings forth is considered as important as anything else brought forth. Thus the therapist is not the one to choose what is more important for the client.
Therapist: I wonder who you are when you are yourself.
Elisabeth: I can do what I feel like. It is okay if I’m in bed or if I’m crying. No demands, no expectations. My parents respect my situation and me. They instinctively know what I need. It is like being a little girl again. It feels safe. I can hide until I’m ready to come back again. [Long thoughtful pause; therapist silently awaits further thoughts.] But then this is how I am when I’m having a bad day. [Cries] I don’t know who I am anymore. I used to be happy. I used to be busy. And interested. Will I be able to come back to life with a tinnitus like this?
Following the rule of horizontalization, everything just said by Elisabeth is of equal importance. The therapist is not to judge, for instance, whether it is more important to examine Elisabeth’s relation to her parents or to examine her thoughts on tinnitus. A choice has to be made on where to continue from. Thus the therapist first mirrors what he or she just heard. Assuming that Elisabeth verifies this, the therapist may continue as follows:
Therapist: Elisabeth, what would be most important for you right now? To go deeper into the bad days, to explore more whom you used to be, or to take a closer look at the parts of you that seem to have been lost?
This example does not imply that the client necessarily has to be asked every time what step to take next. The therapist can choose to go further into one direction but has to keep in mind that other directions may be important to explore further.
The existential therapist is mainly focused on the present because the present is seen as a result of both the past and the future. Therefore, the therapist’s mind is not occupied by speculations about possibly unresolved traumatic events experienced, for instance, in the client’s childhood, youth, or adulthood and their influence on tinnitus. Especially initially in therapy this is of great relevance because most people regard tinnitus as something incomprehensible that has come out of the blue. The client may risk feeling misunderstood, and may even develop uncomfortable and suspicious feelings toward psychological therapy, if the therapist is focused on clarifying such influences.
Thus, metaphorically speaking, the therapist holds the map of the landscape while the client remembers all the many roads. The therapist also shows the map to the client, so that the person can clearly see how far he or she has come, what he or she has successfully gone beyond, and which roads seem to be out there waiting to be explored. This is done to make the client join the process of deciding which road to choose, while at the same time taking care that the client is not losing his or her way. At some point the client takes over the map.
We have outlined some of the important concepts of Tinnitus Person-Centered Therapy, realizing that not everything, for instance, the important philosophical theory on which existential therapeutic practice is based, has been explained. We refer the interested reader to our literature list. Throughout the rest of this chapter the reader will find the concepts elaborated when relevant.
We want to underline the fact that, in our experience, it is most important to meet every new client with tinnitus with an unbiased mind. Consequently, when talking with the client for the first time, we bracket our idea about tinnitus being the expression of something connected to personal problems: Maybe something quite simple that, if treated appropriately, would bring relief, has been overlooked. Maybe it is about personal problems. Maybe the client will profit much more by cognitive-behavioral therapy.
To assess as precisely as possible which kind of intervention should be offered, we collect as much information as possible from the client.
Clinical Protocol
The Initial Telephone Interview
Potential clients first contact us by phone (except for a few who write us and whom we then ask to call). During the initial telephone call we conduct a basic interview that covers the following points.
DETERMINING THE CLIENT’S PURPOSE FOR CALLING
Why is the person calling right now? Has some special event occurred (e.g., onset of tinnitus, worsening of tinnitus)? Is he or she in need of urgent help for psychological intervention (e.g., in a severe crisis or suicidal)? Is the choice of going into psychological therapy undertaken randomly or as a result of careful consideration? Is the individual seeking advice (e.g., on partial masking or where to find an audiologist with a thorough knowledge of tinnitus) rather than wanting to go into therapy? Does he or she want an appointment?
Examining this point gives us an idea about the individual’s emotional state: how badly is the person doing, and why? Should we take the person on as a client immediately, or can the person wait 1 or 2 weeks? Is the person “shopping” for a cure? If so, he or she will most likely leave therapy after one or two sessions, thus wasting money and everyone’s time. Perhaps the person would be better off being referred to someone with an audiological background who can answer hearing questions and provide sound therapy.
DETERMINING THE CLIENT’S UNDERSTANDING OF THE ETIOLOGY OF TINNITUS AND INTERVENTIONS ALREADY UNDERTAKEN
This point addresses what the client knows of or has heard about the etiology of tinnitus, what other intervention(s) (than possibly psychological/psychiatric) the client actually has been offered (i.e., medical examination, hearing aids, noise generators) and whether this makes sense to the person.
It happens that the suffering diminishes or even disappears when information is given, scary misunderstandings are corrected, hearing aids or noise generators are offered, or the use of these devices is explained further. Here therapy often turns out to be irrelevant. When we encounter such unresolved problems, we either refer to the relevant professional or we take care of them ourselves—depending, of course, on whether we have the necessary knowledge. In this context we recommend that psychologists or psychotherapists treating tinnitus both acquire relevant knowledge about tinnitus and hearing and create a good professional interdisciplinary network that can provide the client with whatever support is needed.
DETERMINING WHY THE CLIENT HAS CHOSEN TO CONTACT THIS PARTICULAR CLINIC
We examine the expectations of the client as well as whether it is by accident that the person has chosen our clinic or whether the choice is based on particular knowledge of us. The aim is to understand whether the individual is seeking psychological help in general or is seeking us in particular after learning of our practice using Tinnitus Person-Centered therapy. This enables us to adjust expectations.
If the person’s choice is based on the fact that we prefer to use person-centered therapy, we want to clarify whether the client has any idea of what this actually implies. Being in existential therapy is very different from being, for instance, in psychodynamic-oriented therapy, and the client should be made aware of the most fundamental features characterizing existential therapies. Some of the more traditional psychotherapeutic concepts, such as the subconscious, repression, projection, transference, and countertransference, are not used in person-centered therapy. In line with this, the existential therapist does use the method of interpretation.
We examine whether the person’s call is a result of advice from a professional employed, for example, at the hearing clinic as well as the individual’s feelings about this advice. The recommendation can be relevant. However, sometimes the recommendation reflects the professional’s own feelings of hopelessness and depression that sometimes arise when working with people who seem impossible to help. Such feelings can be very scary and difficult to handle for a professional, especially if the professional has not learned a psychologically based method on how to cope with clients in crisis. In our experience it is important to keep in mind that the client may feel helped very well by the professional, especially if the professional just listens without taking steps toward action (referring or giving advice on how to get better), thus conveying the sense that the feelings expressed are both understandable and acceptable. If this is the need of the client, being recommended to seek psychological intervention may be experienced as a kind of rebuff on behalf of the professional. It may cause feelings of being wrong, unacceptable, or difficult or elicit ideas of having become (or being made into) a “psychological case.” Such feelings can inhibit the therapeutic process and need to be addressed before therapy is initiated.
We recommend that clinicians without a good clinical psychological back-ground seek psychological supervision of their work with difficult clients or refer to someone who does have that background. The ability to be helpful for clients who have severe feelings of hopelessness and sadness can be challenging.
Sometimes the client has been referred so that we can determine whether therapy can decrease the impairment of tinnitus so that the person can return to work. This situation can give rise to feelings of insecurity and suspicion. We examine whether such feelings are present because they can block the therapeutic process.
We determine whether the client has been encouraged to call us by a spouse, relative, friend, or colleague. If that is the case, does the client agree on this idea? What are the expectations of the spouse, relative, or colleague? Will we in reality have both the client’s and this other person’s expectations during therapy? Is the client at all motivated for psychological treatment? This needs to be clarified.
FINDING OUT ABOUT THE CLIENT’S PREVIOUS OR ONGOING EXPERIENCE WITH THERAPY
We determine whether the client has been in therapy before or is going to therapy somewhere else (e.g., with a psychologist or a psychiatrist). We determine whether the client is on any kind of medication, and if so why.
If the person has been in therapy previously and this has been a positive experience, then it may be possible to build on this in the new therapy. However, many clients have had negative experiences with a former therapist that risk being transferred to the new therapeutic relationship, blocking a smooth and fruitful relational development between client and therapist.
Sometimes it is seen that changing therapists reflects general problems with relating to others or enduring the development of a closer kind of relationship. Such a theme can give rise to problems, for instance, in couples counseling. In the sphere of tinnitus, the theme may arise if we encourage the client to relate in a different and more dialogue-focused way toward his or her tinnitus without having taken care of the existence of such a relational theme. Here the client may simply refuse such an idea, get angry, feel insulted, or even want to stop therapy. The problem also may appear disguised as wanting to end therapy quite suddenly. This often happens when the relationship between the therapist and client is developing, providing a safe base for opening up for very private considerations. If during the initial phone interview or during the first sessions of therapy we get the feeling that such a theme may be present, we gently mention this to the client (or wait until the right situation during therapy). If the client’s reaction confirms our thoughts during therapy, we will need to be observant of such situations. We’ll encourage the client to be aware of such feelings and mention them whenever they appear, to transform such themes into ways of being that may be more in the service of the client and the way the person wants to undertake his or her way of living.
We do not take clients into therapy who are at the same time undergoing psychological therapy. With clients taking drugs for psychiatric disorders, we want to be sure that their psychiatrists are prepared to cooperate with us and that the psychiatrists are not undertaking psychotherapy. If so, we encourage the client to continue therapy with the psychiatrist. Generally speaking, we are more reluctant to take in clients with psychiatric disorders.
EXAMINING THE CLIENT’S PSYCHOLOGICAL “MINDEDNESS” AND EXPECTATIONS OF DURATION AND OUTCOME OF THERAPY
One of the aims of the existential therapies is to examine the client’s psychological “mindedness.” How do we best meet the individual’s expectations? Is the person able to enter into dialogue with his or her tinnitus, or will such an attempt be felt to be too “far out”? Is the client, generally speaking, reflective, or does he or she prefer concrete solutions, advice, and tools? Will it be of more help to the client’s needs, for instance, to provide cognitive-behavioral therapy or some kind of relaxation therapy, or will the person achieve more by applying the method of existential therapies? The choice of therapeutic method will be a result of the examination of this point and may very well exclude use of the existential approach.
Another aim is to examine how much time and money the client is prepared to invest when the outcome cannot be foreseen. Do the client’s expectations of duration of the therapy match our own? Does the individual have the impression that therapy has to go on for years, or only one or two sessions? This has to be clarified, as well as the client’s ability to pay for the therapy.
PROVIDING INFORMATION ABOUT ETHICS AND CONFIDENTIALITY
During the interview (when it seems appropriate) the client is informed that our interactions are strictly confidential.
It is our experience that most clients will expect the promise of confidentiality. However, most clients have not thought about what this actually means, whereas others, because of past medical experience, are used to interdisciplinary sharing of information. Therefore, they may not expect this discretion on our behalf. Going into psychological therapy, however, is something very special, something that the client does for himself or herself; it gives clients an opportunity to create a kind of secure and open-minded room of their own where all kinds of thoughts and considerations are invited to emerge. It is a safe place where the client can share thoughts not shared with anybody else but the therapist. Underlining the promise of secrecy will enhance the client’s feelings of confidence and safety.
SUMMING UP
We continue by giving a summary of what we think we have heard or understood during the initial interview. The purpose is to give the client the possibility to correct any misunderstandings or to explain further.
In light of all the information gathered through this initial interview, we usually have achieved a very clear idea, first and foremost, of whether we find ourselves prepared to take this individual into therapy and, second, of whether using the person-centered approach will be in the service of the client and his or her sphere of problems. If both of these requirements are met, we introduce this to the client. If the client wishes to go into Tinnitus Person-Centered therapy, we briefly explain how it is undertaken.
Assuming that the client is prepared to go into therapy, we continue with the following points.
CLARIFYING FORMALITIES
This point informs the client of formalities, such as telephone hours, fee, observance of meeting hour, and rules for cancellation. These should all be addressed before therapy is undertaken.
It is our experience that being precise and structured gives the client a feeling of safety. Because the client actually is hiring the therapist, it is appropriate to make a contract regarding the frames and conditions for therapy that is both understandable and acceptable to the client.
The General Questionnaire
If the client is interested in starting therapy with us, we give a general questionnaire (see Fig. 15–1) and request that it be returned to us before the first session. Some really like this; others do not appreciate the idea of returning a completed questionnaire to someone they have not met. Of course, we respect this. If, however, the client is prepared to undertake this task (and most are), we underline the fact that the person should not feel obliged to answer questions that make him or her feel uncomfortable. Some of the questions have been touched on during the initial phone call. We encourage the client to repeat those answers in writing.
The primary objective is to obtain as much information as possible about the client that can add to the understanding of the client in his or her present situation. Therefore, the questionnaire covers all aspects of the individual’s life, including the possible resources of the client. The questions are formulated in an open way, thus giving clients the possibility to describe their present situation as freely as possible. Consequently, the word tinnitus is not mentioned. Therapists applying the existential framework may find the issue of the questionnaire quite contraindicated because working existential centered means meeting the client in that patient’s “here-and-now,” thus bracketing as much data and assumptions as possible. We have realized, however, that when it comes to a physical complaint like tinnitus, it is very important to “scan” as broadly as possible the client’s life history because sometimes events that the client either has forgotten or does not attach great importance to actually explain some of the difficulties adjusting to tinnitus. When the client takes the time to complete the questionnaire, such important events are apt to pop up. Also, it is our experience that clients seeking psychological help for their tinnitus suffering feel much safer and that their needs are met when we as therapists both meet them in their here-and-now and show a sincere interest in all the bits and pieces that through time have evolved and constitute their present life. For instance, we have experienced that early separation from some parents due to illness and a stay in a hospital has resulted in a sort of flowing anxiety interplaying with tinnitus in a negative way.
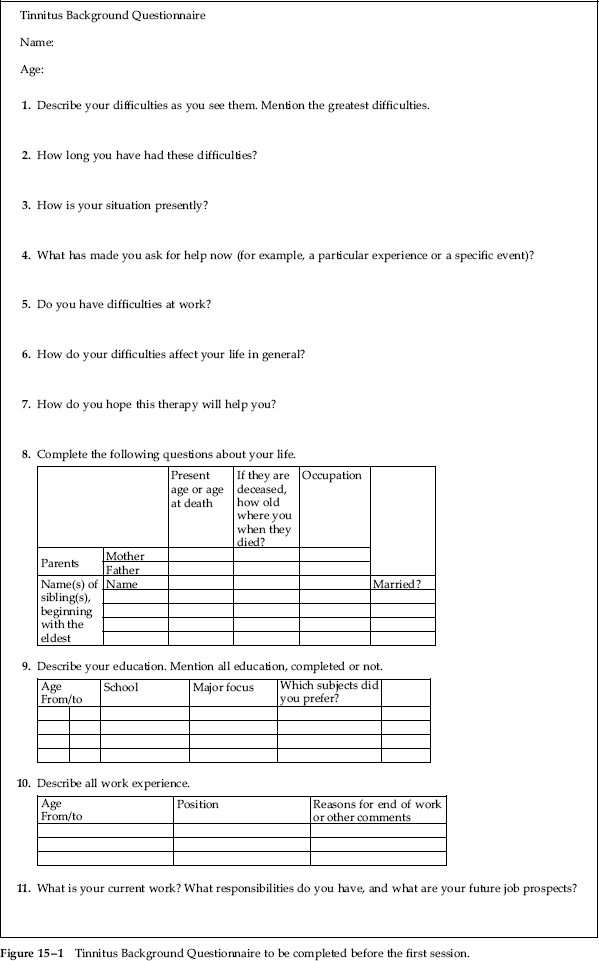
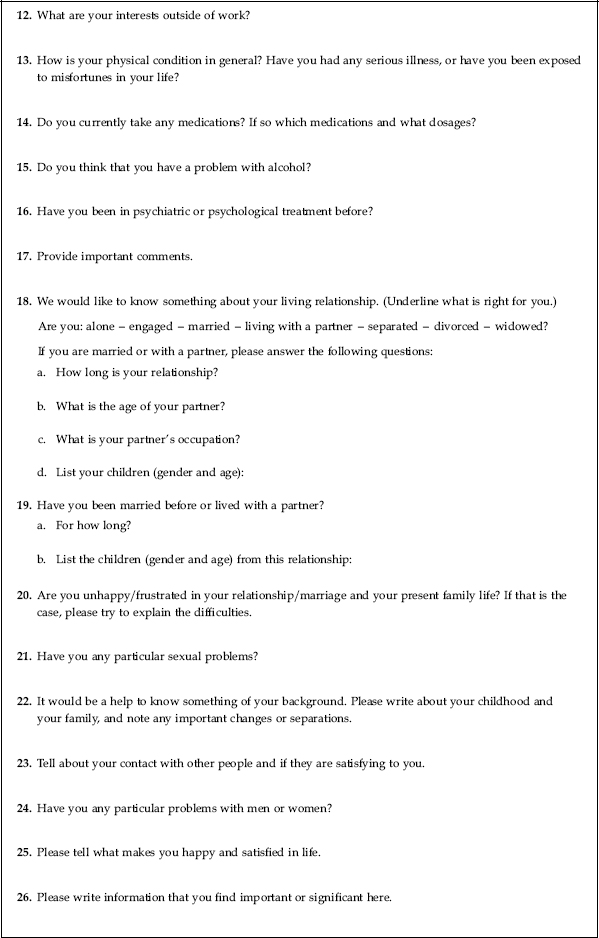
Figure 15–1 Tinnitus Background Questionnaire to be completed before the first session.
The secondary objective is to provide for the client an opportunity to reflect upon his or her life, including what is important right now. If the most important thing right now is tinnitus, the client can choose to attach importance solely to tinnitus when completing the questionnaire. It is not uncommon that clients, during the process of completing the questionnaire, become aware of issues that may interplay with their suffering or become intrigued by some of their answers. Therefore, completing the questionnaire constitutes the first move toward being more reflective on and more curious about existential-centered issues such as the way one chooses to live life. One could say that by completing the questionnaire, the therapeutic process already is initiated before the client actually meets the therapist at the first session.
We end this first contact with the client by saying that the person is always welcome to contact us if any questions arise before the first session.
Preparing for the First Session
We carefully read the questionnaire to review the overall history of the client. The completed questionnaire may contain important information that we need to clarify further to assess whether this particular information is of (or will be of) importance for the present situation with tinnitus or for the therapeutic process. For example, the client might mention episodes of severe alcohol abuse or that one of the client’s parents died by some severe disease or died while the client was still a child. If there are such important issues, we will deal with them during the first session. Depending on the type of information as well as the client’s responses we may very well change plans for the undertaking of therapy/choice of method or refer the client to a more relevant regime. Normally, the thorough phone interview will have shed light on such things.
Going through the completed questionnaire invariably gives rise to some assumptions on the nature of the tinnitus suffering. One of the important tasks in existential therapy, however, is to gain insight into how the client experiences things as clearly as possible. If the therapist is not aware of his or her own assumptions and therefore cannot bracket them, these assumptions can make the picture of the client’s experience unclear. While going through the completed questionnaire, we therefore try to be aware of the nature of our assumptions. We keep them in mind because sometimes presenting the assumptions to the clients—after they have had the chance to clarify their situation—may add a new perspective on the client’s situation.
During therapy we will be very careful with bracketing what we think we know (stemming either from what the client has said to us on the phone or written in the questionnaire) in favor of grasping what the client actually is bringing into therapy. Bracketing what the client said on the phone is necessary because nobody is a static being. Consequently, something may have changed or developed since we first spoke with the client. We have to be open to this possibility—and this openness is achieved by bracketing. This is in line with existential philosophers who have claimed that human existence is fundamentally dynamic in nature (Cooper, 2004).
The rest of this chapter rests on the premise that the client is suited to therapy integrating the existential framework.
The First Sessions
At the first meeting we are careful to start with a bit of informal talk because this normally makes the client feel comfortable and welcome. It is our experience that clients need some time to adjust to this new situation, and we wish to support them in gathering themselves and their thoughts. We continue by encouraging clients to move their attention inward, reflecting upon what it feels like to be with us, the therapist, right now. At the first session this often gives rise to sentences like “I’m nervous” “This is new to me, I’m a bit excited,” and “I’m wondering if I can do this the right way.” Such considerations can be important to examine further. What are they about? What exactly is it that is making the client nervous, and does this influence tinnitus? What are the client’s thoughts on doing therapy “the right way”? Where do these thoughts come from? These considerations may lead to asking the client to be more explicit on how he or she would like therapy to be. Which demands does the client hold toward the therapist? What is important for the client in the therapeutic sessions? What would the client like to achieve? Hence quite early in therapy clients are trained to continuously be aware of their thoughts and needs and through this to get a clearer sense of who they are and who they truly want to be.
It is interesting to note that after a few sessions many of our clients adopt this procedure, subsequently introducing it in the beginning of every session. Actually, one could call this procedure a “tool”—a method of finding yourself right in this moment and explore how you are doing. Are things okay, or is there something that should be done or thought about in a different way to make you feel better? Training oneself in creating such a moment of reflection corresponds to what quite a few clients want to learn; namely, to be aware of the influence of life’s manifold challenges and how they in reality are affecting the individual.
In the first half of the first session we also go through the answers from the questionnaire, paying particular attention to the information that we have highlighted for clarification. We are especially careful to address information that may be of relevance to the client’s present situation with tinnitus. Depending on the content of the completed questionnaire, this may last for the rest of the first session.
At some point in the first half of the first session we explain that each therapeutic session belongs to the client and that it therefore is up to the client to decide where to start. Thus, at some point in the beginning of the session, we will say: So, where would you like to start?
During the first (and quite often also the second) session we are very attentive to whatever the client brings forth (e.g., whiplash due to car or motorcycle accident, episodes of depression or anxiety, diabetes). We consider these bits of information in the context of the client’s answers to some of the first questions on the questionnaire:
• Describe your difficulties as you see them.
• Mention the greatest difficulties.
• How long have you had these difficulties?
• How is your present situation?
• In what way do your difficulties affect your life in general?
• In what way do you hope the therapy helps you?
At the end of the first or the second session we extract themes or issues that we think could be valuable to work with during therapy, comparing these with what the client has answered on the questions mentioned above. Against this background we then try to determine the direction we should head and what should be achieved. We present our thoughts to the client, being very careful to make the client be as explicit as possible: Does the client agree with our thoughts, or are his or her thoughts and expectations headed in another direction? We want the client to be active and to take responsibility for the direction of the therapeutic process, and therefore we are willing to adjust our suggestions, as long as the client’s ideas make sense and are realistic. Therapy is not something that is done to the client but something that he or she is doing together with us.
Having come this far, we agree on a tentative number of sessions and the time between sessions. Having formulated this contract, therapy proceeds. From time to time the contract is reviewed to find out whether we are holding the direction, whether adjustment is needed.
How Is Therapy Undertaken?
In the first part of the therapeutic process, tinnitus most likely will be the pivotal point. Therapy, however, cannot change the fact that tinnitus is present. What may be achieved is a more rewarding way of regarding tinnitus, and this quite often happens, when the client can attach meaningfulness to the tinnitus. Then the client is freed from the disturbing, annoying, or scarring impact of tinnitus.
An important therapeutic strategy, therefore, is to redirect the client’s focus from tinnitus alone to the way the person tackles self-imposed demands, problems, and other dilemmas in life. When facing these issues, the client may realize that other ways of being in life will be much more in line with who he or she is and how he or she wants life to be. The next step is to set priorities as well as to investigate the consequences of the actions and new attitudes that grow during the therapy.
Thus the therapist has to listen to what the client says about tinnitus and be attentive to whatever else the client is conveying about how he or she exists in life. Let us return to the case study of Elisabeth. The therapist has asked her what would be most important for her to look into (horozontalization).
Elisabeth: I don’t really know. I just wish you could tell me that tinnitus sooner or later will go away. But you can’t, I know that. [Pause] I just have to keep on running.
Therapist: What are you running away from?
Elisabeth: From my agony, from not being able to do anything but listen to tinnitus. I keep checking whether it has changed or is the same. … From the phone calls. I don’t want my friends talking to me in this situation. If I answer the phone or go to classes, I have to pretend—and I can’t.
Therapist: What are you pretending?
Elisabeth: That I’m myself, you know. Happy, cheerful, strong. The one that you can count on. Always there for the others. [Pause] It is such a fight to pretend. Ah—I don’t have the strength to pretend. Tinnitus is wearing me out.
Therapist: Do I get you right? Because of tinnitus, you cannot be together with anybody except your parents because you then fight to pretend that you are as you always have been, and this fight is too much for you. Is that so?
Therapist: What would happen if you let some close friends see you the way you are now?
Elisabeth: I haven’t really thought about it. I just shut down. I’ve always done that when I’m sad. Down with the curtains and off to my parents. In bed. Always. [Pause] Why can’t I let them know how I am these days? [Pause] I guess that I have this idea that they would be shocked if they saw me like you see me now. [Cries silently; pause]
Therapist: Elisabeth, do I seem shocked?
Elisabeth: No, but then you don’t get shocked. You’re professional, used to people like me.
Therapist: So one has to be a professional or your parents in order not to be shocked seeing you so sad?
Elisabeth: No, that’s not what I am saying; it’s just that… well, I do hear that it could sound so … [Pause; stops sobbing] This is too far out! [Pause] What I mean is, well… I just think that I cannot very well show how I feel to my friends, not even the close ones. [Pause, then bursts out] I would feel so ashamed of myself! [Blushes] I feel so ashamed right now this very minute. [Starts crying again; a handkerchief is used for tears as well as for a kind of hiding away—the whole face is dried of tears several times.]
In this example, Elisabeth presents several of the bits and pieces that constitute a part of her life. One bit shows us her assumptions of what professionals can handle, another of how close friends will react when seeing her down. One is about what she can let close friends know of her and what she should hide from them. Another is about her way of coping with sadness and challenges (running away). All these need to be clarified.
It is very tempting to make therapeutic assumptions about how all these bits and pieces are interconnected. One of the therapeutic challenges is, as already mentioned, to continuously be aware of these assumptions, trying to bracket them while meeting the client in the now. The therapist, for instance, meets Elisabeth in the now when asking her: “Do I seem shocked?” The therapist here employs one of the strategies used in the existential therapies approach; namely, using the relationship between the client and the therapist to see what their relation is like, what it gives to the client, and from there to explore whether it differs from the relations that the client with others. The existential therapist also will encourage the client to use their relationship actively to try out new ways of thinking and being. Thus the therapeutic relationship is understood as human and represents the world outside the therapeutic room. This presupposes that the therapist is willing to step down from the professional pedestal, thus being both human and professional (and in this sequence).
In the example the intervention brings forth a new bit of information: Elisabeth’s feeling of being ashamed when revealing how badly she is doing. In other therapeutic frameworks at this point it might be of interest to explore where this feeling stems from; that is, to look into the past. When working existential, different feelings like shame will be explored, with the focus on how they are experienced by the client in the present and on how they can be evolved so that they are less stressful and negative. This is done with the intention of making the client able to experience feelings in a more differentiated and giving way, both in the present and in the future. Thus the next move of the therapist could be questions like “Could you please stay with your feeling of being ashamed, as painful as it may be for you, and tell me more about it?”
What clients typically bring forth as answers to such questions are fearful considerations of revealing themselves as weak, imperfect. They may feel anxious about the reactions of others, of becoming a burden to others; they may have the idea that they are worth something only if they “are” a certain way, typically strong and cheerful, competent. Quite often such clients cannot imagine how to exist if they are not always hiding away such vulnerable parts of themselves.
One therapeutic step could be to make Elisabeth clarify what it would feel to learn that a close friend has always hid her anxiousness, sadness, and other stressful feelings. Another step could be to consider a more balanced way of living, for instance, by exploring how it would be to let a close friend know of the feelings that are difficult for Elisabeth to live with. Here the therapeutic relation could be used as a “test room”:
Therapist: Feeling ashamed is so stressful. [Pause] One really feels like hiding away. [Elisabeth nods affirmatively.] Yet you have been very courageous. You have stayed here with me, telling me something that you normally do everything to cover up. How does that feel? [Pause]
Elisabeth: Uhmm … I feel relieved….as if a pressure on my chest has diminished. I feel okay. [She looks straight at the therapist.]
Therapist: So, when it is possible for you to be so courageous with me, I wonder what it would give to you to tell a close friend how you are doing these days?
Elisabeth: I would feel more at ease … less alone. [Long pause] This is quite overwhelming, you know. But I… I’m on to something. Ruth … Ruth is a close friend … she can handle anything.
Here Elisabeth gets an idea of what new ways of being with others can give her. The therapist mirrors her and commends her for courage. He makes her attentive to her feelings. It is interesting to see that what comes up in Elisabeth’s mind isn’t tinnitus but a physical feeling of relief of pressure on the chest. Already at this point a shift of direction is evolving. Tinnitus is not the only physical feeling; for a moment something else is attracting Elisabeth’s attention; namely, that of how to relate to others. Elisabeth also conveys a new bit of her life that needs further exploration: “Ruth can handle anything.” What exactly is it that Ruth needs to handle?
The shift of the focus of existential therapy normally occurs gradually. For example, and with some surprise, the client may slowly begin to realize that when forgetting to invest energy and time in his or her own mental and physical well-being, tinnitus makes itself heard. From then on tinnitus is transformed as a source of information: “When are you, Tinnitus, most annoying, and why is that so?” “What do you take away from me, and what does your presence give me?” “What messages might you carry for me to uncover?” “What is it that you want from me, what are you telling me?” “Am I doing the right thing for me these days?” Tinnitus has been transformed into something meaningful.
Some clients come to the point of putting tinnitus in perspective, serving as an example of the challenges that life imposes on all human beings. Such clients start becoming very aware of the fact that anything can happen at any time. Because of tinnitus, the client has learned that each of us has the freedom to decide which meaning we will attach to or create about the things that happen to us. As a consequence, tinnitus can be understood as something stressful and limiting. However, it also can be understood as something meaningful and expanding. Having come so far, other challenges may be regarded not as something limiting but as something that can contain new possibilities for development and meaningfulness. It is our experience that clients through such processes just described achieve a kind of freer feeling of how to be in life.
Tinnitus continues to be present, and from time to time the client still will find it very annoying. Many of our clients, however, use the sound of tinnitus to keep them on track, to be in touch with what is going on in their life, considering very carefully what their “take” is going to be. For them tinnitus has been transformed from “I have to learn to live with tinnitus” to “I can learn from tinnitus.”
Conclusion
There is no cookbook method to systemizing or manualizing Tinnitus Person-Centered Therapy. First, there exists no grand, all-encompassing system for how to undertake existential therapy (Cooper, 2004). Second, even if every existential therapist followed the overall principle for undertaking existential therapy for the same client, every course will have its own individual way of being (here existential therapy does not differ much from, for instance, psychodynamic-oriented therapy). The way in which the therapeutic process proceeds depends on the therapist’s choice of how to use the overall principles as well as on how the therapist is being in the world (remember that the therapist is not passive or reflective but is genuine and direct with clients; this in itself influences the therapeutic process), the client, the way the client exists in the world and whatever he or she brings forth, the relationship between the two of them, and how they move around together in the therapeutic landscape. Therapy is an individual enterprise.
Acknowledgment
The authors want to thank all of our clients who throughout the years have been our patient and most important collaborators in our process of being engaged in the ongoing challenge of trying to realize what existential therapy is about. Without their confidence and courage it would only have been a theoretical fantasy that we would have been able to describe in this chapter. The authors also have learned so much from the sources listed in the References section; each of them illustrates and explains the rich tapestry of existential practices. Readers who want to explore the philosophy of existential therapy should consult the writings of Medard Boss, Franz von Bretano, Martin Buber, Edmund Husserl, Martin Heidegger, Karl Jaspers, Søren Kierkegaard, Jean-Paul Sartre, and Maurice Merleau-Ponty.
References
Boss M. Existential Foundations of Medicine and Psychology. Hillsdale, NJ: Jason Aronson; 1994
Cohn H. Existential Thought and Therapeutic Practice: An Introduction to Existential Psychotherapy. London: Sage Publications; 1997
Cooper M. Existential Therapies. London: Sage Publications; 2004
Frankl V. Man’s Search for Meaning. London: Washington Square Press; 1984
Frankl V. The Will to Meaning. London: Meridian; 1988
From F. Perception of Other People. New York and London: Columbia University Press; 1971
Jacobsen B. Eksistensens psykologi, en introduktion. Copenhagen: Hans Reitzels Forlag; 1998
May R. Psychology and Human Dilemma. Copenhagen: Van Nostrand; 1967
Moran D, Mooney T, eds. The Phenomenology Reader. London: Routledge; 2002
Spinelli E. Demystifying Therapy. London: Constable; 1994
Spinelli E. Tales of Un-Knowing: Therapeutic Encounters from an Existential Point of View. London: Duckworth; 1997
Spinelli E. The Interpreted World: An Introduction of Phenomenological Psychology. London: Sage Publications; 2000
Spinelli E. The Mirror and the Hammer: Challenges to Therapeutic Orthodoxy. New York: Continuum; 2001
Strasser F. Emotions: Experiences in Existential Psychotherapy and Life. London: Duckworth; 1999
Strasser, F, Strasser A. Existential Time-Limited Therapy: The Wheel of Existence. Chichester, UK: Wiley and Sons; 1997
van Deurzen. E. Everyday Mysteries: Existential Dimensions of Psychotherapy. London: Routledge; 1997
van Deurzen E. Existential Counselling and Psychotherapy in Practice. London: Sage Publications; 2002
Yalom ID. Existential Psychotherapy. New York: Basic Books; 1980
Yalom ID. The Gift of Therapy: Reflections on Being a Therapist. London: Piatkus; 2001
< div class='tao-gold-member'>



