Total thyroidectomy has significantly changed over the years from a morbid procedure to one that is performed routinely on an outpatient basis. This article reviews the history of thyroid surgery with regard to hemostasis, discusses surgical vascular anatomy, and describes the methods of hemostasis. It compares traditional hemostatic surgical techniques with newer techniques such as the Harmonic Scalpel and LigaSure hand pieces. The use of adjunctive hemostatic agents and indications for a drain in thyroid are discussed.
Key learning points
At the end of this article, the reader will:
- •
Understand the risk of bleeding in thyroid surgery.
- •
Have a good knowledge of the neck vessels that can lead to significant perioperative bleeding and describe the management of post-thyroidectomy hemorrhage.
- •
Be able to compare conventional techniques to newer technologies for hemostasis.
- •
Understand the role of hemostatic agents as adjuncts in thyroid surgery.
- •
Be able to discuss the role of a drain in the prevention and management of bleeding and hematoma formation after thyroid surgery.
Introduction
- •
Abu al-Qasim
- ○
In 952 AD , Islam’s legendary medieval surgeon performs first goiter excision.
- ○
His report states that the patient “just avoided exsanguination.”
- ○
- •
Diffenbach
- ○
In 1848, he stated this was ‘‘one of the most thankless, most perilous undertakings which, if not altogether prohibited, should at least be restricted.’’
- ○
- •
Theodor Billroth
- ○
In 1860, 8 of his first 20 patients with goiter died perioperatively leading to cessation of the surgery.
- ○
In 1866, with improved anesthesia, asepsis, and hemostasis, his death rate dropped to less than 10%.
- ○
- •
Emil Theodore Kocher
- ○
In 1909, he won the Nobel Prize for work in decreasing thyroidectomy mortality to less than 1%.
- ○
With close attention to hemostasis, he achieved 0.5% mortality in 5000 thyroidectomies by 1912.
- ○
The first total thyroidectomy for goiter was reported in 952 AD by Islam’s legendary medieval surgeon, Abu al-Qasim. In his initial report, he stated that the patient “just avoided exsanguination.” Diffenbach further described thyroid surgery as “One of the most thankless, most perilous undertakings which, if not altogether prohibited, should at least be restricted.” Despite European sentiment that thyroid surgery was a terrible procedure, Theodor Billroth took on the challenge of the operation. However, in 1860, 8 of his first 20 patients died perioperatively. Emil Theodore Kocher, a trainee of Billroth, was the first to use precise surgical technique and meticulous hemostasis to reduce the mortality rate to 0.5% in more than 5000 thyroidectomies. His work in thyroid surgery led to a Nobel Prize in 1909.
Introduction
- •
Abu al-Qasim
- ○
In 952 AD , Islam’s legendary medieval surgeon performs first goiter excision.
- ○
His report states that the patient “just avoided exsanguination.”
- ○
- •
Diffenbach
- ○
In 1848, he stated this was ‘‘one of the most thankless, most perilous undertakings which, if not altogether prohibited, should at least be restricted.’’
- ○
- •
Theodor Billroth
- ○
In 1860, 8 of his first 20 patients with goiter died perioperatively leading to cessation of the surgery.
- ○
In 1866, with improved anesthesia, asepsis, and hemostasis, his death rate dropped to less than 10%.
- ○
- •
Emil Theodore Kocher
- ○
In 1909, he won the Nobel Prize for work in decreasing thyroidectomy mortality to less than 1%.
- ○
With close attention to hemostasis, he achieved 0.5% mortality in 5000 thyroidectomies by 1912.
- ○
The first total thyroidectomy for goiter was reported in 952 AD by Islam’s legendary medieval surgeon, Abu al-Qasim. In his initial report, he stated that the patient “just avoided exsanguination.” Diffenbach further described thyroid surgery as “One of the most thankless, most perilous undertakings which, if not altogether prohibited, should at least be restricted.” Despite European sentiment that thyroid surgery was a terrible procedure, Theodor Billroth took on the challenge of the operation. However, in 1860, 8 of his first 20 patients died perioperatively. Emil Theodore Kocher, a trainee of Billroth, was the first to use precise surgical technique and meticulous hemostasis to reduce the mortality rate to 0.5% in more than 5000 thyroidectomies. His work in thyroid surgery led to a Nobel Prize in 1909.
Vascular anatomy: arteries
Superior Thyroid Artery
- •
Branch off the external carotid artery
- •
Associated with the external branch of the superior laryngeal nerve (SLN)
- ○
SLN lies less than 1 cm from the superior pole vessels in about 37% of patients and below the upper border of the gland in 20%, thereby putting the nerve at significant risk of injury during thyroid surgery
- ○
- •
Lateral traction on superior pole can be helpful to prevent injury
- •
Fig. 1 shows superior pedicle with lateral traction using an Allis or Babcock clamp
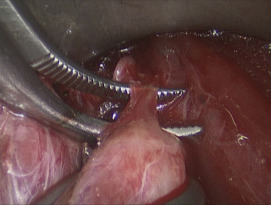
The superior thyroid artery is the first branch of the external carotid artery and descends inferomedially into the central neck (see Fig. 1 ). Care should be taken when dividing the artery to avoid injury to the external branch of the SLN given that it is less than 1 cm from the superior pole vessels in 37% of patients and below the upper border of the gland in 20%. The latter puts the nerve at particularly high risk. Lateral and inferior traction on the superior pole can help identify and avoid the nerve while opening the avascular plane.
Inferior Thyroid Artery
- •
Branch of the thyrocervical trunk
- •
Main vascular supply to the parathyroid glands
- •
Travels posterior to the common carotid artery to enter central neck
- ○
Artery and its branches have variable relationship to recurrent laryngeal nerve (RLN)
- ○
- •
In 10% of cases, the RLN lies between branches of the artery
- •
Attempt to ligate distal to parathyroid branches
- •
Fig. 2 shows inferior artery posterior to the common carotid artery
The inferior thyroid artery arises as a branch from the thyrocervical trunk that arises from the subclavian artery (see Fig. 2 ). In addition to supplying the thyroid gland, these vessels are the main blood supply for both the superior and inferior parathyroid glands. The artery travels posterior to the common carotid artery and has a variable relationship to the RLN. In 10% of cases, the artery will run between branches of the RLN, putting the nerve at particularly high risk during ligation. An attempt should be made to ligate the artery distal to the parathyroid branches to prevent hypoparathyroidism ( Fig. 3 ).
Thyroidea Ima Artery
- •
Arises from the brachiocephalic trunk and ascends in front of the trachea to supply the lower portion of the thyroid gland
- •
Uncommonly encountered but can cause significant bleeding if not identified and controlled
Perforating Tracheal Blood Vessels
- •
Small vessels around Berry ligament that can significantly put the RLN at risk when cauterization is attempted
- •
Fig. 3 shows vessels at Berry ligament
Vascular anatomy: veins
Anterior Jugular Veins
- •
Identify near the midline raphe at the beginning of surgery to prevent injury
- •
Understand that there may be bridging vessels in the midline
- •
Fig. 4 shows anterior jugular veins and bridging vessels
Superior Thyroid Veins
- •
Smaller and within the superior pedicle
- •
Superior veins also associated with the SLN
Inferior Thyroid Veins
- •
Usually associated with inferior parathyroid glands
- •
Anterior to the inferior thyroid artery
- •
Drain directly into the innominate vein and are usually easily ligated
Middle Thyroid Veins
- •
Found laterally during dissection of the strap muscles off of the gland
- •
Course superficial to common carotid artery to enter internal jugular vein
- •
Can be multiple branches
- ○
Fig. 5 shows middle thyroid veins
- ○
Intrathyroidal Capsular Veins
- •
Can cause significant bleeding and can be quite prominent in large goiters
- •
Bipolar cautery is generally enough to control the bleeding
- ○
Fig. 6 shows control of intrathyroidal capsular veins
- ○
The anterior jugular veins are the first encountered during thyroid surgery (see Fig. 4 ). These should be carefully visualized during division of the midline raphe to prevent injury. Because the fascia is released superiorly and inferiorly, understand that bridging veins can be present. The superior and inferior thyroid veins are much smaller. The superior vein runs within the superior pole pedicle whereas the inferior vein drains directly into the innominate vein and is anterior to the inferior thyroid artery. These vessels are easily identified and ligated during capsular dissection. The middle thyroid veins are found during lateral dissection and multiple branches may be present (see Fig. 5 ). These should be divided just outside the capsule. In general, no nerves or parathyroid tissue are associated with the middle veins. Intrathyroidal or capsular veins can be quite prominent in patients with large goiters (see Fig. 6 ). If injured, these vessels can generally be controlled with bipolar electrocautery.
Why is hemostasis important?
- •
To maintain a low intraoperative blood loss and avoid transfusion
- •
To avoid inadvertent injury of the laryngeal nerves and parathyroid glands
- •
To prevent postoperative hematoma causing airway compromise
- ○
Fig. 7 shows a post-thyroidectomy hematoma
- ○
Hemostasis is of the utmost importance during thyroid surgery. Minimizing intraoperative blood loss is the goal but meticulous hemostasis as described by Kocher with capsular dissection is critical. Bleeding during thyroidectomy blurs operative planes thus putting the RLN and parathyroid glands at significant risk of injury. Ultimately, meticulous hemostasis is also important to prevent the dreaded complication of postoperative hematoma (see Fig. 7 ).
Postoperative Hematoma
- •
Incidence of 0.1% to 1.1%
- •
Most occur within first 6 hours of operation
- •
Causes include
- ○
Loosening of the surgical knot
- ○
Opening of the cauterized vessel due to hypertension, retching, or Valsalva during recovery
- ○
Oozing from cut edges of the thyroid
- ○
- •
Prevention
- ○
Perform Valsalva before closing
- ○
Consider closing strap muscles loosely to prevent airway obstruction
- ▪
Described by Terris in 2009
- ▪
- ○
- •
Treatment
- ○
Most hematomas need to be evacuated and re-explored
- ○
If patient is stable without air hunger it is acceptable to intubate before opening the neck
- ▪
The most experienced team member should intubate because marked edema of the epiglottis and arytenoids can be present
- ▪
- ○
- •
Postoperative care proceeds no differently than primary thyroid surgery
- •
Fig. 8 shows the strap muscles being approximated loosely
Postoperative hematoma occurs at a rate of about 0.1% to 1.1%. Almost all cases occur in the first 6 hours after surgery and can be the result of several surgeon or patient factors. Several studies have shown that only around 20% of hematomas occur between 6 and 24 hours postoperatively and virtually no hematomas occur afterwards. Prevention of symptomatic or life-threatening hematoma can also be achieved by avoiding tight reapproximation of the strap muscles as described by Terris in 2009 (see Fig. 8 ). Although this will not prevent hematoma, it should allow earlier recognition of the process and delay the lymphatic outflow blockage that leads to laryngeal edema and dyspnea. Performing a Valsalva can also be effective to identify potential sources of bleeding before closing. Treatment of hematomas really depends on the symptomatology. Most hematomas need to be evacuated and re-explored but only an unstable or progressively worsening hematoma in a patient requires immediate evacuation at the bedside. Often, reintubation in a controlled operating room (OR) environment is possible. The most senior endoscopist should perform the intubation because significant epiglottis and arytenoid edema may be present. Postoperative care generally does not change after an evacuation.
Surgical hemostasis
Clamp, Tie, and Cut
- •
Traditional form of vessel control
- •
Requires meticulous capsular dissection
- •
Requires larger incision and does require more time to perform
- •
Surgical clips are an alternative
Electrocautery
- •
Good for small vessels
- •
Thermal energy is up to 150 to 400°C
- •
Monopolar cautery causes more heat dispersion
- •
Bipolar cautery is more pinpoint and defined
Harmonic Scalpel
- •
Cut and coagulate at lower temperatures of 50 to 100°C
- •
Less dispersion of heat energy
LigaSure
- •
A form of bipolar electrocautery that seals vessels
- •
Direct pressure also required for vessel sealing
- •
Fig. 9 shows LigaSure (Medtronic, New Haven, CT), clamp, tie, cut, bipolar electrocautery, and Harmonic Scalpel (Ethicon Inc., Sommerville, NJ, USA)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


