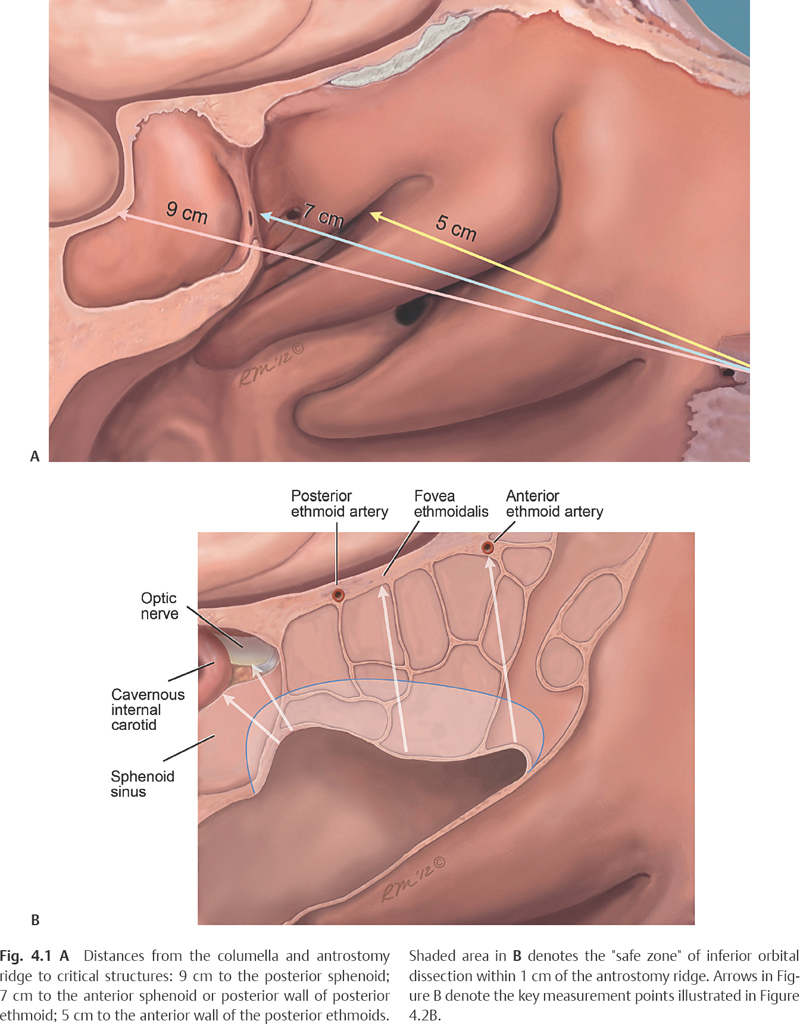
4 In 1994, May and colleagues introduced six friendly anatomical landmarks that are almost always present despite previous surgery1: 1. the arch (or convexity) formed by the posterior edge of the lacrimal bone, marking the lacrimal duct at the anterior margin of the middle meatus 2. the anterior superior attachment of the middle turbinate (vertical lamella) 3. the middle meatal antrostomy and its bony “ridge,” along its superior border, formed by the junction of the floor of the orbit with the lamina papyracea and resected margin of the posterior fontanelle. 4. the lamina papyracea 5. the nasal septum 6. the arch of the posterior choana Using these landmarks, revision endoscopic sinus surgery (ESS) for recurrent or persistent disease in the maxillary, ethmoid, sphenoid, or frontal sinuses can be safely performed. May was one of the first to acknowledge that in advanced sinus disease anatomical landmarks, such as the uncinate process, basal lamella, and superior or middle turbinates are not always readily identifiable. He was also one of the first to point out that the floor of the orbit, as seen through an antrostomy, serves as a consistent landmark from which other structures may be found. The bony “ridge” along the superior border of the antrostomy corresponds to the medial orbital floor, which facilitates identification of the inferior lamina papyracea prior to proceeding with an ethmoidectomy. The ridge is also useful in locating the posterior ethmoid and sphenoid sinuses (see Chapter 5). Despite prior reports that showed great inter-subject variability, May and Stankiewicz reintroduced the possible clinical efficacy of using standard measurements from the columella to orient the surgeon during ESS.2,3 They based this proposal on anecdotal experience and prior anatomical studies by others, noting that the distance from the area of the anterior nasal spine to the sphenoid ostium is ~60 mm (range 47–70 mm).4–6 If one more centimeter is added for the length of the columellar base, the mean distance to the sphenoid ostium would be approximately 70 mm. For this reason, May advocated labeling instruments with colored tape to warn the surgeon when the anterior face of the sphenoid is reached (~7 cm). In fact, today, many instruments come premarked in centimeters markings from the tip to allow for such measurements. However, there will likely be variability among surgeons’ measurements of these distances. In isolation, these measurements have not been shown to be clinically reliable. Schaefer was the first to described a “hybrid or combined technique” that blended the conservation goals of the AP approach with the anatomical virtues of the PA approach.7 Surgery begins with identification and complete removal of the unci-nate process. If further surgery of the ethmoid sinus is warranted, the maxillary natural ostium is enlarged posteriorly or inferiorly, rather than anteriorly, to avoid injury to the lacrimal canal. Schaefer noted that this immediately exposes the level of the orbital floor. Like May, Schaefer recognized the importance of the medial orbital floor as a very important landmark to facilitate identification of the inferior lamina papyracea prior to proceeding with an ethmoidectomy. He also advocated removal of the inferior two-thirds of the ethmoid cells in an AP direction using a zero-degree telescope. Often this involves removal of most, if not all, of the basal lamella of the middle turbinate to address the drainage area of the posterior sinuses and to facilitate entry into the sphenoid sinus. If the ostium cannot be visualized or palpated, the sphenoid is entered in the inferomedial quadrant of the anterior wall of the sinus. This approach ensures that the surgeon will maintain a safe distance from the skull base. It is only after the sphenoid roof has been identified that a superior dissection of the sphenoid face or ethmoid cavity (if indicated) is performed, as with the PA approach. Schaefer’s approach, like May’s, recognizes the importance of performing an antrostomy prior to an ethmoidectomy to identify the orbital floor and medial orbital wall. Schaefer was the first to note the importance of performing an inferior ethmoidectomy before proceeding posteriorly using the medial orbital floor as a reference point. As the surgeon proceeds posteriorly, it is the orbital wall that dictates the trajectory and not some ill-defined and often distorted lamella or turbinate structure, as advocated by proponents of the AP approach. Schaefer’s study did not, however, define the vertical extent of the initial “inferior ethmoidectomy” from the level of the medial floor of the orbit. Mosher has shown that the height of the ethmoid labyrinth ranges from 2.5 to 3 cm8; however, this height may vary even more depending on whether it is measured anteriorly or posteriorly. Similarly, the distance of two thirds of the ethmoid cells, as described by Schaefer, can be quite variable. The maximum vertical distance permitted for an “inferior ethmoidectomy” as the surgeon proceeds posteriorly before critical skull base structures are at risk remained not clear. Similarly, the distances to the critical structures in the posterior and lateral walls of the sphenoid sinus remain undefined. In 2001, Casiano confirmed May’s and Schaefer’s observations on a series of human cadavers.9 In this study, two examiners, with varying experience in endoscopic sinus surgery, performed endoscopic and direct measurements from the columella and medial orbital floor to critical orbital and skull-base structures. The distances to four critical skull-base or orbital structures (the carotid artery, optic nerve, mid-ethmoid roof, and anterior ethmoid artery), and to the anterior and posterior walls of the sphenoid sinus, were measured (Fig. 4.1A,B). The mean, ranges, and standard deviations for all measurements (endoscopic and direct) were calculated. In addition, the variability in measurements between examiners and between the endoscopic and direct measurements was also determined. The mean and range of values for each of the variables correlated well both between examiners and between endoscopic and direct measurements. The columellar measurements appeared to be very consistent between examiners and between endoscopic and direct measurements (Fig. 4.2A,B).
The Use of Anatomical Landmarks
Ento Key
Fastest Otolaryngology & Ophthalmology Insight Engine