Purpose
To evaluate visual performance of subjects implanted monocularly with a small-aperture hydrophobic intraocular lens (IC-8 IOL).
Design
A prospective, noncomparative, multicenter case series.
Methods
A series of 12 patients, presenting for cataract surgery, were implanted monocularly with a single-piece hydrophobic acrylic intraocular with a centrally located opaque annular mask measuring 3.23 mm in total diameter with a 1.36 mm central aperture. Uncorrected distance, intermediate, and near visual acuities (UDVA, UIVA, and UNVA); depth of focus; and subjective symptoms were evaluated for 12 months after implantation. Mean ± standard deviation visual acuity is reported in logMAR.
Results
The mean monocular UDVA, UIVA, and UNVA improved significantly from 0.42 ± 0.18, 0.52 ± 0.22 and 0.66 ± 0.23 preoperatively to 0.06 ± 0.08 ( P < .0001), 0.07 ± 0.11 ( P < .0001), and 0.11 ± 0.15 ( P < .0001) at 1 month, respectively, and remained stable until 12 months. At 12 months, 100%, 100%, and 92% of patients achieved 20/32 or better binocularly for UDVA, UIVA, and UNVA, respectively. One hundred percent of eyes maintained 20/40 or better visual acuity over a range of +0.50 diopter to −1.50 diopters of defocus. Subjects implanted with the IC-8 IOL perceived a small magnitude of visual symptoms and rated their symptoms on the lower end of the severity scale.
Conclusion
Early results demonstrate that monocular IC-8 intraocular lens implantation provides a continuous, broad range of vision and excellent acuity across all focal distances.
Recent improvements to the intraocular lens (IOL) designs focus on providing spectacle independence following cataract extraction. Multifocal IOLs provide improved near visual acuity over standard monofocal lenses ; however, the retinal image quality with this type of implant is still noticeably worse when compared to a standard aspheric monofocal IOL owing to the splitting of light between distance and near foci. This also leads to reduced contrast sensitivity and a well-documented increase in the incidence of glare and halos in subjects with multifocal IOLs. Single-optic accommodating IOL designs have shown minimal to moderate near visual benefit with no loss in visual quality.
The IC-8 IOL (AcuFocus Inc, Irvine, CA) is a 1-piece hydrophobic acrylic posterior chamber IOL into which a circular mask with a small 1.36 mm central aperture has been embedded. The IOL mask works by extending the depth of focus and its design is based on the KAMRA corneal inlay, which operates under the principle of small-aperture optics. The IOL mask is 15% smaller in diameter than the one used in the corneal inlay to account for more posterior placement in the IOL plane and contains fewer microperforations, and is flat or has no curvature when compared to the last-generation KAMRA inlay, which has a curvature of 7.5 mm.
The small-aperture KAMRA corneal inlay has been implanted in over 1000 subjects during clinical trials and over 20 000 subjects worldwide. Small-aperture corneal inlay implanted in presbyopic subjects, with a natural, clear crystalline lens, increases the depth of field and thereby improves intermediate and near vision, with minimal to no change to distance vision. Small-aperture inlay subjects have better contrast sensitivity in the inlay eye when compared to the multifocal IOLs, and better binocular contrast sensitivity when compared to subjects with both multifocal and accommodative IOLs.
The main objective of the study is to investigate the impact of small-aperture technology in an IOL to extend the benefit to subjects that are scheduled for cataract surgery. In this paper we present preliminary results from a case series of 12 subjects who were monocularly implanted with the IC-8 IOL and followed for a minimum of 12 months as a part of the ongoing clinical study. Visual acuity, depth of focus, and subject satisfaction will be reported preoperatively and at all postoperative visits up to 12 months.
Methods
Study Design
This is a case series on the first 12 subjects implanted in a prospective, nonrandomized (EUDAMED or European Databank for Medical Devices, CIV-AT-13-07-011473), multicenter clinical study. The clinical study sites were located in the Philippines and Austria. These subjects underwent cataract extraction by phacoemulsification and implantation with the IC-8 IOL in only 1 eye and were followed with postoperative visits over a 12-month period. The study was performed in accordance with the Declaration of Helsinki and approved by the Ethics Committees of the respective investigational sites. Subjects were screened for eligibility, and informed consents were obtained from all eligible subjects.
Eligibility Criteria
Subjects had to be ≥45 years of age at the time of eligibility and had to have clear intraocular media other than cataract and have best-corrected distance visual acuity of 20/30 or worse, or significant visual symptoms/complaints as a result of cataract in the operative eye. Subjects also had to have an anterior chamber depth, exclusive of corneal thickness, preoperatively of 2.5–4.75 mm. Key exclusion criteria were subjects with life-threatening systemic disease, uncontrolled hypertension, autoimmune disease, uncontrolled diabetes, anterior segment pathology, glaucoma, previous retinal detachment, or retinal pathology in the operative eye; subjects using systemic medications with significant ocular side effects; corneal endothelial cell count of <1800 cells/mm 2 in the operative eye; and previous ocular surgeries. No criteria were required for the fellow eye.
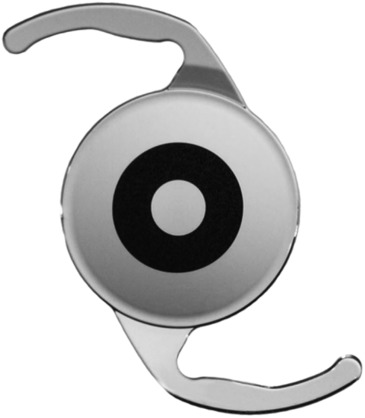
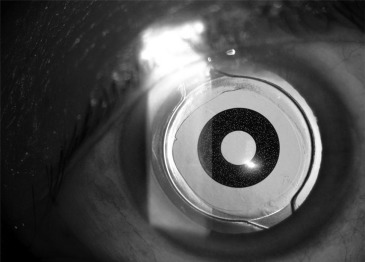
Device Description
The IC-8 IOL is a sterile, single-use, 1-piece hydrophobic acrylic IOL with a centrally located, embedded polyvinylidene difluoride annular mask intended to improve near vision based on the concept of small-aperture optics ( Figures 1 and 2 ). The IC-8 IOL material and design is based on the 1-piece hydrophobic acrylic posterior chamber, monofocal IOL (ASHF600) manufactured by BioTech Vision Care, which has attained the CE mark and is sold worldwide. The AcuFocus IC-8 IOL is intended for implantation in the capsular bag. The lens has modified C haptics and an overall diameter of 12.5 mm. The biconvex aspheric optic is 6 mm in diameter with a 360-degree square posterior edge, and is ultraviolet absorbent, with the hydrophobic material having an index of refraction of 1.48 at 35 °C. The embedded annular mask has an outer diameter of 3.23 mm with a central aperture of 1.36 mm in diameter and contains 3200 microperforations on its annulus (sparing the periphery) ranging in size from 7 to 10 μm diameter and arranged in a pseudorandom fashion. The microperforations are present to aid with the foldability of the IOL and also decrease the possibility of delamination of the IOL mask. The IC-8 IOL is available in powers ranging from 16 to 27 diopters (D) in 0.5-D steps.
Surgical Technique
All surgeries were performed by 2 experienced surgeons. Twelve subjects were implanted with the IC-8 IOL following removal of their cataractous lens. This initial case series was completed prior to verification, validation, and CE approval of the injector. Therefore the IC-8 IOLs were implanted flat through a 6.0 mm scleral incision. The subjects were all targeted for a −0.75 D manifest refractive spherical equivalent (MRSE).
Preoperative Examination
Preoperative examination included pupillary measurement (Procyon P3000, Procyon Instruments, London, UK); manifest refraction; uncorrected and best-corrected far, intermediate, and near visual acuities; optical biometry with the IOL Master (Carl Zeiss Meditec, BRD; eg, axial length, anterior chamber depth lens thickness, white to white, IOL power calculation); central keratometry; computerized corneal topography (Keratron, Optikon, Rome, Italy); specular microscopy of the corneal endothelium (Konan Medical, Irvine, CA); slit-lamp examination (Haag-Streit, Mason, OH, USA); intraocular pressure measured by applanation tonometry (Haag-Streit, Mason, OH, USA); dilated fundus examination; and a baseline subject satisfaction questionnaire.
Postoperative Examination
Visual acuities were measured using the Optec 6500 Vision Tester (Stereo Optical) and high-contrast visual acuity charts. Visual acuities were recorded using the number of Early Treatment Diabetic Retinopathy Study (ETDRS) letters and were converted to logarithm of the minimal angle of resolution (logMAR). Monocular and binocular uncorrected distance (UDVA) at 4 m, intermediate (UIVA) at 80 cm, near (UNVA) at 40 cm, best-corrected distance (BDVA), distance-corrected intermediate (DIVA), and near (DNVA) visual acuities were measured at all visits.
For the IC-8 IOL–implanted eye, the desired refractive endpoint to optimize visual performance and increase spectacle independence was determined to be −0.75 D based on previously published work in the field of small-aperture optics within the cornea. Target-corrected distance, intermediate, and near visual acuities were measured by simulating −0.75 D of myopia over the best-corrected distance midpoint refraction in all subjects at 1, 3, 6, 9, and 12 month postoperative visits. In order to overcome the uncertainty of a refractive endpoint created by the extended depth of focus provided by the small-aperture mask within the optic, the upper and lower limits of the depth of focus are determined and the midpoint refraction calculated. Midpoint manifest refraction was performed at the preoperative visit and at visits 1 week and 1, 3, 6, 9, and 12 months postoperatively.
Defocus curve testing was performed on the IC-8 IOL eye of all subjects while viewing ETDRS charts calibrated for 4 m testing in standard photopic conditions, using the best-corrected distance midpoint manifest refraction. The technician first defocused the image by placing a +5.00 D lens in front of the subject’s best-corrected distance midpoint manifest refraction, and then progressively changed the defocus lens in 0.50-D increments from +5.00 D to −5.00 D. Visual acuity measurements were obtained through each successive increment of additional 0.50 D lenses.
Subjects rated their satisfaction with near vision on a scale of 1 (very dissatisfied) to 7 (very satisfied). Subjects also rated symptoms such as blurry/fluctuating vision, color disturbances, distortion, dryness, glare, halos, night vision problems, pain/burning, double vision, and ghost/overlapping images. If the subjects reported experiencing a specific symptom, then they were asked to rate it in on a scale of 1 (very mild) to 7 (very severe). If no symptoms were reported it was rated as 0.
A small sub-study was conducted on 5 subjects from one site for the purpose of evaluating the visual fields and the ability of the retinal surgeon to examine and diagnose the retina with routinely performed diagnostic testing in the eyes implanted with the IC-8 IOL. Visual field testing was performed with the Zeiss Humphrey 24-2 SITA standard. Diagnostic tests such as binocular indirect ophthalmoscopy, fluorescein angiography, optical coherence tomography, and fundus photographs were obtained on all 5 subjects. The technician completed a questionnaire on the ease of performing the diagnostic tests and the retinal surgeon completed a questionnaire on his ability to adequately examine, diagnose, and, if needed, perform laser treatment or vitrectomy in the IC-8 IOL eye.
Adverse Event Reporting
Both serious and nonserious adverse events were graded on a 3-point scale (mild, moderate, severe) and were reported in detail. The adverse events were graded as mild (condition noticed but no disruption of normal daily activities), moderate (condition sufficient to reduce or affect normal daily activity), and severe (condition with inability to work or perform normal daily activity). Investigators also assessed whether there was a reasonable possibility that the study device and/or the surgical procedure caused or contributed to the adverse event.
Statistical Analysis
Statistical analysis was performed using the JMP statistical package (SAS Institute, Inc). Statistical significance for continuous parameters was determined by performing pair-wise comparisons using the nonparametric Wilcoxon-Mann-Whitney rank-sum tests and corresponding Hodges-Lehman confidence intervals. A P value less than .05 was considered statistically significant.
Results
Demographics and Refraction
Table 1 shows the preoperative demographics of the 12 subjects included in the study. All 12 subjects completed every scheduled follow-up examination through the 12-month visit. Nine subjects (75%) were female and 3 (25%) were male. Nine subjects (75%) were Asian and 3 (25%) were white. Six of the 12 subjects had a monofocal IOL in their fellow eye. Four of the 6 subjects received the monofocal implant prior to implantation with an IC-8 IOL and the remaining 2 received a monofocal IOL implant in the fellow eye 3 months post IC-8 IOL implantation. Table 2 shows the mean MRSE at the scheduled follow-up visits. There was no statistically significant difference in MRSE between 1, 3, 6, 9, and 12 months postoperatively ( P > .05).
| Mean (SD) | Range | Confidence Interval | |
|---|---|---|---|
| Age (y) | 60.5 (7.5) | 42.6, 71.4 | 56.2, 64.7 |
| MRSE (D) | 0.95 (1.06) | −0.50, 2.88 | 0.27, 1.62 |
| Sphere (D) | 1.19 (0.99) | 0, 3.25 | 0.57, 1.88 |
| Cylinder (D) | −0.48 (0.55) | −1.50, −0.50 | −1.02, −0.48 |
| Near reading addition (D) | 2.17 (0.75) | 0, 3.00 | 1.69, 2.64 |
| Visit | MRSE ± SD (D) | Minimum (D) | Maximum (D) | Lower CI 95% | Upper CI 95% |
|---|---|---|---|---|---|
| Preoperative | 0.95 ± 1.06 | −0.50 | 2.88 | 0.27 | 1.62 |
| Month 1 | −0.33 ± 0.52 | −0.88 | 1.00 | −0.66 | 0.00 |
| Month 3 | −0.23 ± 0.51 | −1.25 | 0.63 | −0.56 | 0.10 |
| Month 6 | −0.40 ± 0.83 | −2.25 | 1.00 | −0.92 | 0.13 |
| Month 9 | −0.32 ± 0.46 | −1.38 | 0.50 | −0.61 | −0.03 |
| Month 12 | −0.10 ± 0.49 | −0.75 | 1.00 | −0.42 | 0.21 |
Uncorrected Near, Intermediate, and Distance Visual Acuity
Monocular
Figure 3 shows the cumulative percentage of patients achieving 20/32 (J3) or better monocular uncorrected visual acuity and mean ± standard deviation (SD) for near, intermediate, and distance at all visits. At 12 months, the mean monocular UNVA, UIVA, and UDVA improved significantly from J10 to J2 ( P < .0001), 20/66 to 20/25 ( P = .0002), and 20/50 to 20/20 ( P < .0001), respectively. There were no significant differences in the mean acuity between the postoperative visits ( P > .05). At 12 months, 92%, 92%, and 100% of subjects achieved 20/32 (J3) or better uncorrected visual acuity for near, intermediate, and distance, respectively.
Binocular
Figure 4 shows the cumulative percentage of patients achieving 20/32 (J3) or better binocular uncorrected visual acuity and mean ± SD for near, intermediate, and distance at all visits. At 12 months, the mean monocular UNVA, UIVA, and UDVA improved significantly from J6 to J2 ( P = .0051), 20/44 to 20/21 ( P = .0051), and 20/32 to 20/20 ( P = .001), respectively. There were no significant differences in the mean acuity between the postoperative visits ( P > .05). At 12 months, 92%, 100%, and 100% of subjects achieved 20/32 (J3) or better uncorrected visual acuity for near, intermediate, and distance, respectively.

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


