Purpose
To determine the effect on corneal pseudoaccommodation of anterior corneal wavefront aberrations in normal corneas and corneas with prior myopic or hyperopic photorefractive keratectomy (PRK) or laser-assisted in situ keratomileusis (LASIK).
Design
Theoretical study.
Methods
In 220 normal eyes, 102 myopic-PRK eyes, and 106 hyperopic-LASIK/PRK eyes, anterior corneal higher-order aberrations (HOAs, third to sixth order, 6- and 4-mm pupils) were computed from the Atlas corneal elevation data using the VOL-CT program. Using the ZernikeTool, corneal optical image quality was evaluated by the polychromatic modulation transfer function with Stiles-Crawford effect. Defocus from −3.0 diopters (D) to +3.0 D was added to corneal HOAs, and depth of focus was defined as the ranges over which the polychromatic modulation transfer function maintains 80% of the peak value (DOF80) and 50% of the peak value (DOF50). The depth of focus values between groups were compared, stepwise multiple regression was used to assess if any Zernike terms significantly contributed to the depth of focus, and correlation analysis was performed to evaluate the correlation between depth of focus and corneal HOAs.
Results
The depth of focus varied widely between corneas, especially in corneas with prior hyperopic-LASIK/PRK. For 6-mm pupil, mean depth of focus values in myopic-PRK and hyperopic-LASIK/PRK corneas were significantly greater than those for normal corneas, and for 4-mm pupil, depth of focus values in hyperopic-LASIK/PRK corneas were greater than those in normal and myopic-PRK corneas. Zernike terms significantly contributing to both DOF80 and DOF50 were fourth- and sixth-order spherical aberration and fourth- and sixth-order astigmatism in normal corneas, third-order vertical coma and fourth-order tetrafoil in myopic-PRK corneas, and third-order vertical coma and fourth-order astigmatism in hyperopic-LASIK/PRK corneas. Depth of focus had weak to moderate positive correlation with HOAs (Pearson correlation coefficient r ranged from 0.300 to 0.583).
Conclusion
These theoretical calculations suggest that certain corneal wavefront aberrations affect corneal pseudoaccommodation. To predict corneal pseudoaccommodation, the most important Zernike term is spherical aberration in normal eyes and coma in eyes with prior laser corneal surgery.
Following cataract surgery with implantation of a monofocal intraocular lens (IOL), some patients attain surprisingly good uncorrected near and distance vision. This phenomenon is referred to as apparent accommodation or pseudoaccommodation. Studies have shown that the pseudoaccommodation is inversely proportional to the pupillary diameter and positively correlated with the depth of field and corneal multifocality. Oshika and associates assessed in pseudophakic eyes the relationship between apparent accommodation and wavefront aberrations of the cornea. They found that the root mean square values of the total third-order (coma-like) aberrations of the cornea were significantly correlated to the apparent accommodation. Evidence for the cornea’s role in pseudoaccommodation has also been noted in eyes that have undergone myopic corneal refractive surgery, with treated patients demonstrating enhanced distance-corrected near acuity and greater measured accommodative range.
Pseudoaccommodation has been traditionally studied using subjective measurements. The purpose of this theoretical study was to assess potential corneal pseudoaccommodation as expressed by calculated depth of focus values and to correlate specific higher-order aberrations (HOAs) to the corneal depth of focus values that were calculated from the corneas of eyes in the cataract population, as well as in eyes following myopic and hyperopic excimer laser ablation.
Patients and Methods
Patients
We included data from 3 groups of patients who visited our clinic or underwent myopic or hyperopic photorefractive keratectomy (PRK) or laser-assisted in situ keratomileusis (LASIK) between May 2002 and March 2007. The first group included 220 eyes of 137 patients, aged 40 to 80 years, with no prior corneal surgery. These subjects were selected from our preoperative cataract patients, and their corneas were measured before undergoing cataract surgery. The second group had 102 eyes of 77 patients, aged 22 to 45 years, who underwent wavefront-guided myopic-PRK by 1 surgeon using the CustomVue STAR laser system (Abbott Medical Optics Inc [AMO], Santa Ana, California, USA) and who had 6 months of follow-up. Lastly, the third group included 106 eyes of 80 patients aged 40 to 59 years who underwent standard (81 eyes) or wavefront-guided (7 eyes) hyperopic-LASIK or wavefront-guided hyperopic-PRK (18 eyes) by 1 surgeon using the AMO STAR laser system. Minimum follow-up was 3 months for LASIK eyes and 6 months for PRK eyes.
Inclusion criteria included: 1) no corneal pathology; 2) no prior contact lens wear or wear discontinued 4 weeks for rigid gas permeable lens, 3 weeks for toric soft contact lenses, and 2 weeks for soft contact lenses; and 3) Humphrey Atlas corneal topographic maps with no missing data points within the central 7-mm zone (Carl Zeiss Inc, Pleasanton, California, USA).
In the myopic and hyperopic groups, we included corneas with different procedures. In our clinic, during that period of time, wavefront-guided myopic-PRK was the dominant procedure for myopic corneal laser surgery. Because of the later approval of the wavefront-guided LASIK for hyperopia by the Food and Drug Administration, the majority of the eyes in the hyperopic group had undergone conventional hyperopic LASIK.
Depth of Focus on the Cornea
Corneal wavefront aberrations up to sixth order for 6- and 4-mm pupils were computed from Humphrey Atlas corneal elevation data using the VOL-CT program (Sarver and Associates Inc, Carbondale, Illinois, USA), which uses the standards for calculation and reporting the optical aberrations of eyes as proposed by Thibos and associates. The topographic maps were recentered around the entrance pupil, and wavefront aberrations from the cornea were calculated using a corneal refractive index of 1.376 for the wavelength of 555 nm.
Corneal optical image quality was evaluated by the polychromatic modulation transfer function with Stiles-Crawford effect. The polychromatic modulation transfer function was calculated using the ZernikeTool program (Abbott Medical Optics Inc). With this program, 7 wavelengths (400, 450, 500, 550, 600, 650, and 700 nm) were used to represent the visible spectrum, and the polychromatic point spread function with Stiles-Crawford effect was weighted in the imaging plane based on the retinal spectral response function.
To evaluate the effect of defocus on corneal image quality, defocus from −3.0 diopters (D) to +3.0 D in 0.1-D intervals was added to the HOAs of the corneas. Desired defocus in diopter was converted to wavefront coefficient in μm and added to the second-order defocus term using the following equation derived from the method described by Applegate and associates:
where C 2 0 is the Zernike coefficient in μm for the second-order defocus term, S is the dioptric power of the sphere expressed in diopter, and R is the radius of the pupil expressed in mm.
The polychromatic modulation transfer function at 15 cycles/degree (equivalent to visual acuity of 20/40 object) was used, and depth of focus was defined by 2 criteria based on the polychromatic modulation transfer function at 15 cycles/degree: 1) the range over which the polychromatic modulation transfer function maintains 80% of the peak value (DOF80); and 2) the range over which the polychromatic modulation transfer function maintains 50% of the peak value (DOF50) (this criterion represents a 50% drop in image quality, which could still provide adequate near acuity).
Statistical Analysis
The depth of focus values between groups were compared using Mann-Whitney test.
Correlation analysis was performed to evaluate the correlation between depth of focus and root mean square (RMS) values of total higher-order aberrations (HOAs, third to sixth order) and third-order, fourth-order, fifth-order, and sixth-order wavefront aberrations of the cornea. Stepwise multiple regression was used to assess if any Zernike terms significantly contributed to the depth of focus. For this purpose, for the left eyes, Zernike coefficients for these Zernike terms with mirror symmetry between both eyes were flipped to match the right eye. SPSS 15.0 for Windows (SPSS Inc, Chicago, Illinois, USA) was used for statistical analysis. The Bonferroni correction was employed for multiple tests. A probability of less than 5% ( P < .05) was considered statistically significant.
Results
Corneal Zernike Coefficients
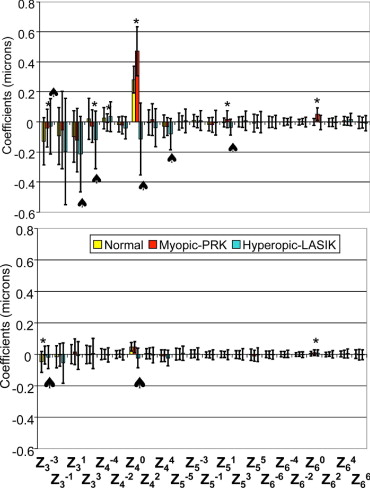
Figure 1 shows the corneal HOAs in normal, myopic-PRK, and hyperopic-LASIK/PRK corneas. Compared to normal corneas, for a 6-mm pupil, myopic-PRK and hyperopic-LASIK/PRK corneas each had significantly different mean coefficient values for 6 Zernike terms: Z(3,−3), Z(3,3), Z(4,−4), Z(4,0), Z(5,1), and Z(6,0) for myopia and Z(3,−3), Z(3,1), Z(3,3), Z(4,0), Z(4,4), and Z(5,1) for hyperopia ( Figure 1 , Top). For a 4-mm pupil, compared to normal corneas, ablated corneas had significantly different mean coefficient values for 2 Zernike terms: Z(3,−3) and Z(6,0) for myopic-PRK corneas and Z(3,−3) and Z(4,0) for hyperopic-LASIK/PRK corneas ( Figure 1 , Bottom) (all P < .05 with Bonferroni correction).
Depth of Focus Values
The depth of focus varied widely among corneas, especially in corneas with prior hyperopic-LASIK/PRK ( Figure 2 ) . The distributions of the depth of focus values are shown in Figure 3 .
Table 1 shows the depth of focus values in each group. There were no significant differences in mean depth of focus values between the 6-mm pupil and 4-mm pupil within each group of eyes. The mean DOF80 and DOF50 values for myopic-PRK corneas were greater than those for normal corneas by 0.04 D and 0.08 D for the 6-mm pupil (both P < .05 with Bonferroni correction) and by 0.00 D and 0.02 D for the 4-mm pupil, respectively (both P > .05 with Bonferroni correction). The mean DOF80 and DOF50 values for hyperopic LASIK/PRK corneas were greater than those for normal corneas by 0.08 D and 0.22 D for the 6-mm pupil (both P < .05 with Bonferroni correction) and by 0.08 D and 0.24 D for the 4-mm pupil respectively (both P < .05 with Bonferroni correction). Lastly, the mean DOF80 and DOF50 values for hyperopic LASIK/PRK corneas were greater than those for myopic-PRK corneas by 0.04 D and 0.14 D for the 6-mm pupil (both P > .05 with Bonferroni correction) and by 0.08 D and 0.22 D for the 4-mm pupil (both P < .05 with Bonferroni correction). Although not demonstrated in Table 1 , in the hyperopic-LASIK/PRK group, there were no differences between depth of focus values among corneas that underwent prior standard LASIK, wavefront-guided LASIK, or wavefront-guided PRK (all P > .05 with Bonferroni correction).
| Group | 6-mm Pupil | 4-mm Pupil | ||
|---|---|---|---|---|
| DOF80 (D) | DOF50 (D) | DOF80 (D) | DOF50 (D) | |
| Normal corneas (n = 220) | 0.53 ± 0.08 | 0.96 ± 0.15 | 0.55 ± 0.14 c | 1.03 ± 0.34 d |
| (0.4 to 0.8) | (0.6 to 1.7) | (0.4 to 1.4) | (0.7 to 2.6) | |
| Myopic-PRK corneas (n = 102) | 0.57 ± 0.13 a | 1.04 ± 0.25 b | 0.55 ± 0.15 c | 1.05 ± 0.40 d |
| (0.4 to 1.3) | (0.6 to 2.4) | (0.3 to 1.4) | (0.6 to 2.9) | |
| Hyperopic-LASIK/PRK corneas (n = 106) | 0.61 ± 0.20 a | 1.18 ± 0.43 b | 0.63 ± 0.22 | 1.27 ± 0.51 |
| (0.3 to 1.4) | (0.6 to 2.7) | (0.4 to 1.5) | (0.7 to 3.5) | |
a,b,c,d For each criterion, depths of focus between groups were significantly different except for pair with a,b,c,d (all P < .05 with Bonferroni correction).
Zernike Terms Contributing to Depth of Focus
Table 2 lists the Zernike terms in descending order of importance that significantly contributed to the depth of focus values for a 6-mm pupil.
| Group | Criterion | Multiple Correlation Coefficient R | Zernike Terms in Descending Order of Importance |
|---|---|---|---|
| Normal corneas | DOF80 | 0.530 | Z(6,0), Z(4,0), Z(6,2), Z(4,−4), Z(4,2), and Z(5,−5) |
| DOF50 | 0.547 | Z(4,0), Z(4,2), Z(6,0), Z(3,−1), Z(3,−3), and Z(6,2) | |
| Myopic-PRK corneas | DOF80 | 0.521 | Z(5,1), Z(3,1), Z(3,−1), and Z(4,4) |
| DOF50 | 0.401 | Z(3,−1), Z(4,4), and Z(3,3) | |
| Hyperopic-LASIK/PRK corneas | DOF80 | 0.469 | Z(3,1), Z(3,−1), and Z(4,2) |
| DOF50 | 0.561 | Z(4,2), Z(5,−3), Z(4,0), Z(3,−1), Z(5,3), and Z(6,−4) |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


