Purpose
To evaluate change in different reading performance parameters after monocular ACI7000PDT corneal inlay implantation for the improvement of near and intermediate vision.
Design
Prospective, interventional case series.
Methods
Twenty-four patients were scheduled for corneal inlay implantation in the nondominant eye in a university outpatient surgery center. Naturally emmetropic and presbyopic patients between 45 and 60 years of age, with uncorrected distance visual acuity of at least 20/20 in both eyes, without any additional ocular pathology were eligible for inclusion. Bilateral uncorrected reading acuity, mean and maximum reading speed, and smallest log-scaled print size were evaluated with the standardized Radner Reading Charts. Measurements of reading parameters and reading distance were performed with the Salzburg Reading Desk (SRD). Minimum postoperative follow-up was 12 months.
Results
The reading desk results showed significant changes in each parameter tested. After 12 months the mean reading distance changed from the preoperative value of 46.7 cm (95% CI: 44.1–49.3) to 42.8 cm (95% CI: 40.3–45.3, P < .004), and the mean reading acuity “at best distance” improved from 0.33 logRAD (95% CI: 0.27–0.39) to 0.24 logRAD (95% CI: 0.20–0.28, P < .005). Mean reading speed increased from 141 words per minute (wpm, 95% CI: 133–150) to 156 wpm (95% CI: 145–167, P < .003), maximum reading speed increased from 171 wpm (95% CI: 159–183) to 196 wpm (95% CI: 180–212, P = .001), and the smallest print size improved from 1.50 mm (95% CI: 1.32–1.67) to 1.12 mm (95% CI: 1.03–1.22, P < .001).
Conclusions
After ACI7000PDT implantation, there were significant changes in all tested reading performance parameters in emmetropic presbyopic patients. These 1-year results indicate that the inlay seems to be an effective treatment for presbyopia.
Within the last decades various surgical procedures for the treatment of presbyopia have been implemented in cataract and refractive surgery. Among the different available surgical options, currently used corneal techniques are based on reshaping the corneal surface (presbyLASIK, intracorneal femtosecond laser, conductive keratoplasty ) or inserting small-aperture inlays.
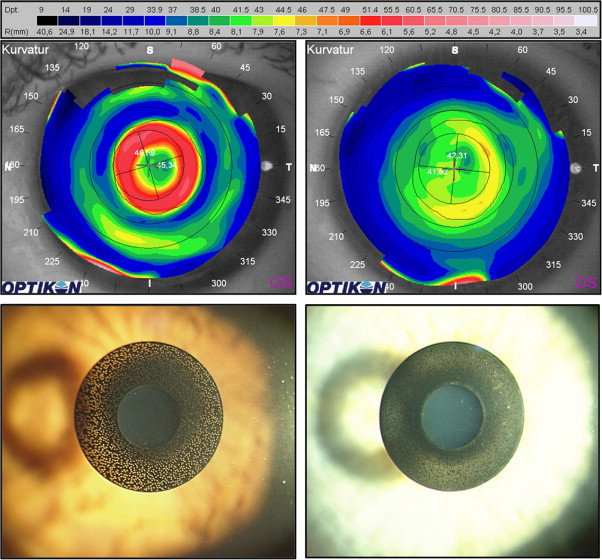
Recently introduced into the market was the KAMRA corneal inlay (AcuFocus, Inc, Irvine, California, USA). By virtue of its gaining the CE mark in 2005, refractive surgeons within the European Union can commercially use this inlay already outside of clinical trials, whereas it is still under investigation in US Food & Drug Administration clinical trials for the treatment of near-plano and plano presbyopia. This intracorneal inlay is designed to increase the depth of focus based on the principle of pinhole optics to restore near and intermediate visual acuity without a significant impact on distance vision. Recent studies support the efficacy and safety of the 1st-generation KAMRA corneal inlay (ACI7000, Figure 1 , Bottom left) for the treatment of presbyopia with published follow-ups of up to 2 years. Within the last 3 years the company has changed the inlay in some specifications. The currently available 3rd-generation KAMRA corneal inlay (ACI7000PDT, Figure 1 , Bottom right) is only 5 μm thick and has more (and smaller) laser-drilled porosity holes than the previous inlay design. Also, the current implantation technique has been modified to some extent. Instead of a flap, a femtosecond laser–assisted pocket is created to minimize the impact on corneal nerves and decrease biomechanical changes.
The assessment of reading performance is considered one of the most important clinical examinations comparing the most important potential benefits of surgical presbyopia treatment. One tool for measuring reading performance is the Salzburg Reading Desk. The system offers computerized testing under standardized conditions while simulating a “natural” reading process. The aim of this study was to evaluate the effectiveness of the ACI7000PDT in improving different aspects of reading performance. In particular, we used the Salzburg Reading Desk to assess uncorrected bilateral reading acuity, reading distance, mean and maximum reading speed, and the smallest log-scaled print size patients could effectively read over a follow-up of 1 year.
Patients and Methods
This prospective cohort study comprised 24 patients after monocular implantation of the 3rd-generation Acufocus KAMRA ACI7000PDT inlay at the University Eye Clinic of the Paracelsus Medical University, Salzburg, Austria.
Subjects were eligible for inclusion in this study if they were naturally emmetropic and presbyopic, between 45 and 60 years of age with a preoperative spherical equivalent of plano, defined as +0.50 to −0.75 diopter (D) with no more than 0.75 D of refractive cylinder—as determined by cycloplegic refraction—and uncorrected distance visual acuity (UDVA) of at least 20/20 in both eyes.
Key exclusion criteria were patients with previous ocular surgeries, anterior or posterior segment diseases or degenerations, or any type of immunosuppressive disorders. In addition, patients using systemic medications with significant ocular side effects or patients with latent hyperopia, defined as a difference of ≥1.00 D between the manifest and cycloplegic refraction, were excluded.
Inlay Studied
We implanted the Acufocus KAMRA ACI7000PDT inlay ( Figure 1 , Bottom right), a 5-μm-thin, microperforated artificial aperture (3.8 mm outer diameter and 1.6 mm inner diameter), centered on the line of sight of the nondominant eye after the creation of a corneal pocket using a femtosecond laser. The inlay is made of polyvinylidene fluoride (PVDF), with nanoparticles of carbon incorporated to make it opaque. This inlay has 8400 laser-drilled porosity holes (diameter: 5–11 μm), arranged in a randomized pattern to allow for a sufficient nutritional flow through the inlay to sustain the viability of the anterior stromal lamella and to prevent corneal thinning and epithelial problems. These holes allow some additional (unwanted) light to pass, for an average light transmission through the annulus of the inlay of approximately 5% (data on file, AcuFocus Inc). This intracorneal inlay is supposed to increase the depth of focus, based on the pinhole effect, to restore near and intermediate visual acuity without significant impact on distance vision.
Surgical Procedure
The “pocket” in the corneal stroma was generated using 3 different types of femtosecond lasers (11× IntraLase Fs-laser, 60 kHz [Abbott Medical Optics, Santa Ana, California, USA], 10× iFs-laser, 150 kHz [Abbott Medical Optics], 3× Femto LDV [Ziemer Group AG, Port, Switzerland]). For the pocket creation a special mask (IntraLase FS-laser, depth 260 μm; iFS-laser, depth 210 μm) or a special software was used (Femto LDV, depth 200 μm). The type of femtosecond laser used for pocket creation and the depth of the pocket had no influence on the surgical outcome. The inlay was removed with forceps from the sterile package and inspected under high magnification for any defects. Via the temporal opening of the “pocket” the inlay was then centered on the stromal bed and centration was controlled (and corrected when needed) with the patient fixating on the microscope light. Centration was regarded as being optimal when the first Purkinje reflex was in the center of the inner diameter of the inlay while the patient was fixating on the microscope’s single light source.
Reading Performance Analyses
The Salzburg Reading Desk system consists of a specially designed reading desk, a computer, and a dedicated software package. Continuous reading distance measurement is performed with video-stereo photogrammetry and additional software processing. With this system, patients choose their reading distance (ie, subjectively most convenient). It has been shown that this technology is a valid and reliable method to evaluate reading speed and reading distance and to calculate reading acuity “at best distance.” Bilateral uncorrected reading acuity, mean and maximum reading speed, and smallest log-scaled print size were evaluated with the standardized Radner Reading Charts. A sentence is accepted, if it can be read with a minimum reading speed of 80 words per minute (wpm). Reading acuity is expressed in logRAD, which represents the reading equivalent of logMAR.
Preoperative and Postoperative Examinations
The preoperative examination included manifest and cycloplegic refractions, UDVA and corrected distance visual acuity (CDVA), uncorrected reading performance evaluation with the Salzburg Reading Desk, slit-lamp examination, corneal topography (Keratron; Optikon Ophthalmic Equipment, Rome, Italy), and dilated fundus evaluation. The reading performance was evaluated at the reading desk by assessing the following parameters: reading distance, mean and maximum reading speed, reading acuity “at best distance,” and the smallest print size (size of a lowercase letter) that could be read effectively. The examinations were all performed at a standard illumination of 500 lux, according to the European norm for the illumination of reading surfaces in offices and libraries. Postoperative follow-up examinations were scheduled for 1, 3, 6, and 12 months. Additionally, patients filled out a satisfaction questionnaire preoperatively and 3, 6, and 12 months after surgery.
Statistical Analysis
Descriptive analysis with 95% confidence intervals for means was performed. Repeated measures ANOVA with 2-sided, paired Student t tests were applied to analyze data. A P value <.05 was considered statistically significant. All analyses were done with STATISTICA 6.1 (Stat Soft Inc, Tulsa, Oklahoma, USA).
Results
All 24 patients enrolled in this study completed every scheduled follow-up examination through 12 months. Table 1 shows the patients’ demographics and preoperative data, including reading parameters. Preoperative UDVA in the surgical eye was 20/20 in 8 patients (33%) and ≥20/16 in 16 patients (67%). Mean spherical equivalent refractive error before inlay implantation was 0.06 ± 0.26 D (range: −0.38 to 0.50 D). No inlay was explanted during the follow-up, no evidence of corneal melt could be seen, and no inlay needed to be recentered.
| Demographic | Value a |
|---|---|
| Age (years) | 52.2 ± 3.2 (48 to 58) |
| Sex (F/M, %) | 50/50 |
| Eye with inlay (R/L, n) | 8/16 |
| Preoperative SE (D) | 0.06 ± 0.26 (−0.38 to +0.5) |
| Preoperative UDVA (lines) | 20/16 ± 0.5 (20/20 to 20/16) |
| Preoperative uncorrected reading performance | |
| Preoperative RD (cm) | 46.7 ± 6.3 (35.0 to 57.5) |
| Preoperative RA “at best distance” (logRAD) | 0.33 ± 0.13 (0.15 to 0.59) |
| Mean preoperative RS (wpm) | 141 ± 20 (112 to 180) |
| Maximum preoperative RS (wpm) | 171 ± 28 (131 to 235) |
| Preoperative smallest log-scaled print size (mm) | 1.50 ± 0.42 (0.94 to 2.32) |
| Preoperative corrected reading performance | |
| Preoperative RD (cm) | 40.9 ± 5.8 (30.7 to 54.9) |
| Preoperative RA “at best distance” (logRAD) | 0.00 ± 0.10 (−0.17 to 0.08) |
| Mean preoperative RS (wpm) | 153 ± 23 (123 to 195) |
| Maximum preoperative RS (wpm) | 190 ± 27 (147 to 230) |
| Preoperative smallest log-scaled print size (mm) | 0.54 ± 0.09 (0.46 to 0.73) |
| Near addition power (D) | 1.90 ± 0.30 (1.50 to 2.50) |
a Age and visual acuity values represented as mean ± standard deviation (range).
Postoperative Reading Performance
The mean reading distance decreased from the preoperative value of 46.7 ± 6.3 cm (range: 35.0 to 57.5 cm) to 44.6 ± 6.2 cm (range: 28.0 to 56.0 cm) 1 month postoperatively, and had a further, statistically significant decrease to 42.8 ± 5.8 cm (range: 34.7 to 55.3 cm) after 12 months ( Figure 2 , Top left; P < .004).
The mean reading acuity “at best distance” statistically significantly improved from the preoperative value of 0.33 ± 0.13 logRAD (range: 0.15 to 0.59 logRAD) to 0.27 ± 0.12 logRAD (range: 0.01 to 0.42 logRAD) after 1 month and was 0.24 ± 0.10 logRAD (range: 0.02 to 0.42 logRAD) after 12 months ( Figure 2 , Top right; P < .005).
The smallest print size increased from the preoperative value of 1.50 ± 0.42 mm (range: 0.94 to 2.32 mm) to 1.20 ± 0.29 mm (range: 0.73 to 1.89 mm) after 1 month, and further statistically significantly increased to 1.12 ± 0.22 mm (range 0.73 to 1.45 mm) during the follow-up period ( Figure 2 , Bottom left; P < .001). A mean improvement in log-scaled reading lines of 1.13 ± 1.03 lines could be seen, with 29% (n = 7) showing no gain or loss and 71% (n = 17) improving up to 4 lines from baseline ( Figure 2 , Bottom right).
Also, reading speed parameters showed statistically significant improvement. Mean reading speed was 141 ± 20 wpm preoperatively (range: 112 to 180 wpm), was 150 ± 26 wpm (range: 105 to 214 wpm) after 1 month, and even slightly further improved within the follow-up period to 156 ± 26 wpm (range: 104 to 222 wpm) after 12 months ( Table 2 ; P < .003). The maximum reading speed increased from the preoperative value of 171 ± 28 wpm (range: 131 to 235 wpm) to 188 ± 35 wpm (range: 135 to 268 wpm) after 1 month, and further increased to 196 ± 38 wpm after 12 months (range: 120 to 298 wpm; Table 2 ; P = .001).
| Mean Reading Speed (wpm) | |||||
|---|---|---|---|---|---|
| Mean ± SD | CI −95% | CI +95% | Min | Max | |
| Preoperative | 141 ± 20 | 133 | 150 | 112 | 180 |
| 1 month | 150 ± 26 | 139 | 160 | 105 | 214 |
| 3 months | 145 ± 22 | 135 | 154 | 96 | 211 |
| 6 months | 150 ± 20 | 141 | 158 | 117 | 194 |
| 12 months | 156 ± 26 | 145 | 167 | 104 | 222 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


