The Ear
Basic concepts
Anatomy and physiology
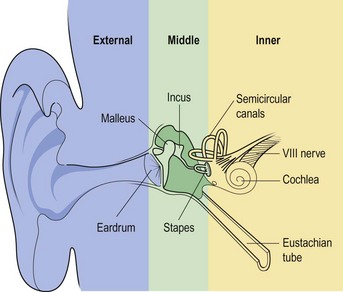
Structurally, the ear has three parts (Fig. 1.1):
The external ear
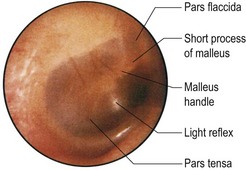
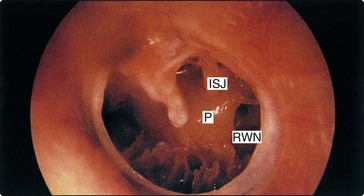
The eardrum is the window of the middle ear and is divided into the pars tensa and pars flaccida. The main landmark on the drum is the malleus handle (Fig. 1.2).
The middle ear
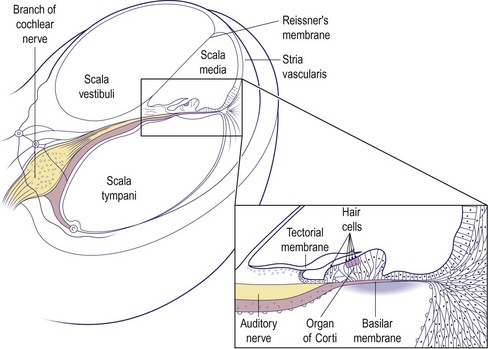
The middle ear is an air-containing space connected to the nasopharynx via the Eustachian tube. It acts as an impedance matching device to transfer sound energy efficiently from air to a fluid medium in the cochlea (Fig. 1.3). The middle ear space, including the mastoid air cells, is closely related to the temporal lobe, cerebellum, jugular bulb and labyrinth of the inner ear. The space contains three ossicles (the malleus, incus and stapes) which transmit sound vibrations from the eardrum to the cochlea. The middle ear also contains two small muscles and is traversed by the facial nerve before it exits the skull.
Symptoms and signs
Symptoms
History taking in ear complaints should be brief but thorough. Table 1.1 provides a reference guide of the major points that should be covered. The otological symptoms are discussed in greater detail later in this section, but it is important to establish the predominant complaint and whether it affects one or both ears.
Table 1.1 Major points in history taking in patients with an otological complaint
| Otological | Nasal |
| Hearing loss – onset and rate of progression | Obstruction, discharge, etc. |
| Otalgia | |
| Otorrhoea | Drugs |
| Tinnitus | Ototoxic agents (e.g. aminoglycosides) |
| Imbalance | |
| Family history | |
| Noise exposure | Hearing loss |
| Previous ear surgery |
Signs
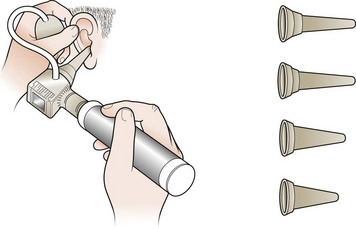
Satisfactory examination cannot be undertaken without adequate lighting. Battery auriscopes with a fibre or glass ring light give a coaxial beam with bright uniform illumination. A pneumatic attachment tests the mobility of the eardrum (Fig. 1.4).
The pinna should be examined for scars and signs of crusting or weeping. Before introducing the auriscope, the ear canal must be straightened by elevating the pinna upwards and backwards (Fig. 1.4). The condition of the ear canal should be noted before the eardrum is examined. If an adequate seal of the canal is achieved by the speculum, gentle pressure on the pneumatic bulb will move the eardrum if the middle ear contains air. This is helpful in distinguishing perforations from thin or translucent segments.
A complete examination also involves viewing the Eustachian tube orifice in the nasopharynx.
Clinical tests of hearing
Tuning fork tests
Rinne test
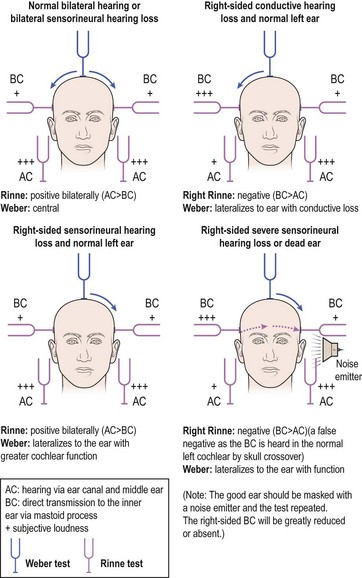
The Rinne test compares air conduction (AC – hearing via ear canal and middle ear) with bone conduction (BC – direct transmission to the inner ear via the mastoid process). The examiner holds the fork by the ear canal and then places it on the mastoid process using gentle counterpressure with the other hand. The patient is asked which position of the fork sounds louder: in front of the ear or touching the mastoid (Fig. 1.5).
Audiometry, vestibulometry and radiology
Audiometry
Subjective tests
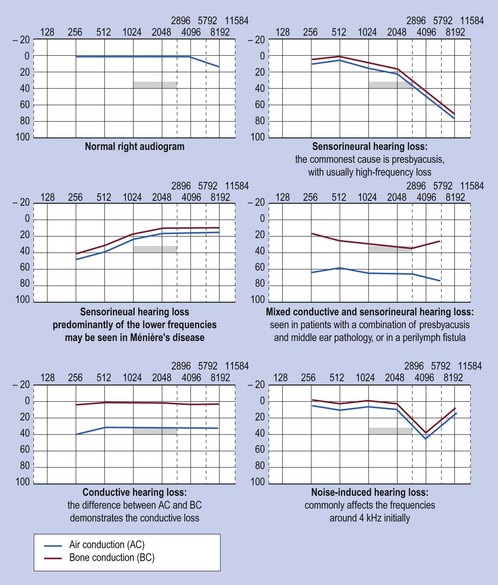
Pure tone audiograms are a standard means of recording hearing levels. Using headphones, each ear is tested individually for air conduction and, if necessary, bone conduction thresholds. The results are usually plotted as a graph. A result of 0 dB (decibels) is the average normal threshold for hearing in young adults (Fig. 1.6).
Objective tests
Impedance audiometry is an extremely useful test in the diagnosis of middle ear disease and some types of sensorineural hearing loss. By varying the pressure in the external ear canal, the compliance (i.e. mobility) of the eardrum may be calculated by the degree of sound reflected from a probe tone. This is very useful when screening for middle ear effusions, particularly in children, and for assessing Eustachian tube function (p. 7). It can also test the integrity of the middle ear mechanism and the auditory reflex arc (stapedius reflex).
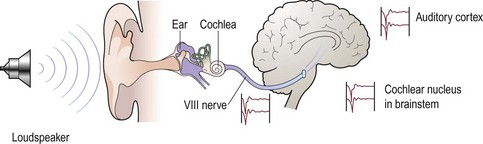
Electric response audiometry (ERA) (Fig. 1.7) is another objective test. An evoked potential in the eighth nerve, brainstem or auditory cortex may be recorded using skin electrodes following acoustic stimulation of the cochlea. This principle is used to objectively assess hearing thresholds where the standard tests are not applicable, e.g. babies, disabled people and suspected malingerers.
Vestibulometry
The vestibule has three parts: the utricle, the saccule and the semicircular canals (see Fig. 1.1, p. 2). Each vestibule tonically discharges information to the brain regarding head position, and linear and angular acceleration. This information is part of the general proprioceptive input (joint, tendon, skin and ocular inputs). Dysequilibrium may be the result of an abnormal input from any part of the proprioceptive sensors, or a dysfunction of the central nervous connection secondary to disease, e.g. ischaemia or demyelination.
Tests
Positional test
From an erect sitting position on a couch, the patient lies flat with the head turned to one side and below horizontal (Fig. 1.8). The onset of any vertigo is noted and the eyes are observed for nystagmus. The feeling of movement and the nystagmus, if present, are allowed to settle before the patient sits upright. The manoeuvre is repeated with the head to the opposite side. This test may help to distinguish vertigo caused by peripheral (otological) as opposed to central pathologies.
Rotation tests and electronystagmography
Rotational tests assess the vestibular response to angular acceleration by measuring nystagmus from surface electrodes around the ocular muscles. Various other tests of eye pivot, optical fixation and suppression of nystagmus may be recorded by electronystagmography. These investigations give information about central mechanisms and disorders of the vestibular nuclei in the brainstem (p. 20).
Radiology
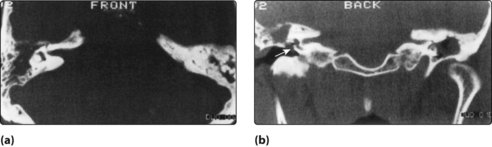
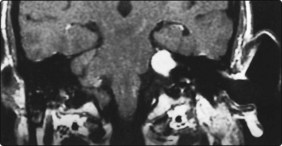
Modern CT scanning and MRI are now widely used to provide information on otitis media with complications, and in the diagnosis of acoustic neuromas (Figs 1.9 and 1.10). MRI is particularly useful in assessing the extent of vascular lesions such as glomus jugulare tumours, and in visualizing the acoustic nerve.
Audiometry, vestibulometry and radiology
 Correctly performed pure tone audiograms are the most reliable method of assessing hearing thresholds.
Correctly performed pure tone audiograms are the most reliable method of assessing hearing thresholds.
 Electric response audiometry may be required in assessing the thresholds in very young infants and others who are unable to respond to subjective audiometric tests.
Electric response audiometry may be required in assessing the thresholds in very young infants and others who are unable to respond to subjective audiometric tests.
 Impedance audiometry is extremely useful in assessing the presence of middle ear effusions.
Impedance audiometry is extremely useful in assessing the presence of middle ear effusions.
 A patient with a positive fistula test in the presence of chronic ear disease requires urgent otological referral.
A patient with a positive fistula test in the presence of chronic ear disease requires urgent otological referral.
Hearing loss – general introduction and childhood aetiology
General introduction
A hearing loss, as mentioned previously, can be conductive, sensorineural or mixed. Any disease affecting the outer or middle ear will produce a conductive deafness. Sensorineural loss results from damage to the cochlea or eighth nerve. The degree of hearing loss can be quantified on an audiogram with the thresholds of hearing quoted in decibels (p. 4).
Table 1.2 lists the most common causes of hearing loss. Most of those leading to a conductive deafness will be evident from history, otoscopy, tuning fork tests and audiometry. However, the aetiology of sensorineural loss is frequently unclear. In these cases, specific points in the history should be determined. These points are listed in Table 1.3.
Table 1.2 Aetiology of hearing loss
| Cause | Conductive hearing loss | Sensorineural hearing loss |
|---|---|---|
| Congenital | Atresia of ear, ossicular abnormalities | Prenatal: genetic, rubella |
| Acquired | External: wax, otitis externa, foreign body | Perinatal: hypoxia, jaundice |
| Middle ear: middle ear effusion, chronic otitis (cholesteatoma, perforated drum), otosclerosis, traumatic perforation of drum (ossicular disruption) | Trauma: noise, head injury, surgery | |
| Inflammatory: chronic otitis, meningitis, measles, mumps, syphilis | ||
| Degenerative: presbyacusis | ||
| Ototoxicity: aminoglycosides, cytotoxics | ||
| Neoplastic: acoustic neuroma | ||
| Idiopathic: Ménière’s disease, sudden deafness |
Table 1.3 Points to cover in clinical history of a patient presenting with hearing loss
Hearing loss in children
The incidence of severe sensorineural deafness is about 1 in 1000. Half of these children have a hereditary type of deafness (Fig. 1.11). The others have hearing losses resulting from acquired causes. Even mild degrees of hearing loss, either conductive or sensorineural, can impair learning ability.
Childhood hearing loss should be suspected in certain groups of individuals (Table 1.4). Children falling into these risk categories should be referred to an audiological physician or otologist for audiometric assessment. This is often a multidisciplinary approach using teachers of the deaf and speech therapists in the same clinic. If a hearing loss can be overcome at an early age, particularly severe sensorineural losses, there is a greater chance the child can attend an ordinary school. Where a hereditary loss is confirmed, a geneticist may advise on risks to future children.
Table 1.4 The childhood groups at risk of suffering from hearing loss
History taking from the parents should concentrate on establishing the answers to specific questions, as well as making a general otological assessment (Table 1.5). Most hearing problems relate to middle ear disease. However, sensorineural deafness may coexist.
Table 1.5 History taking in childhood hearing loss
Otitis media with effusion (glue ear)
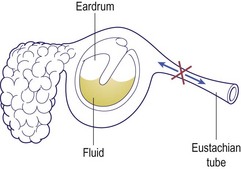
The effusion in the middle ear may be serous, mucoid or thick (glue). The aetiology is usually Eustachian tube dysfunction, where normal ventilation of the middle ear is disturbed (Fig. 1.12). A diagnosis of chronic otitis media with effusion is made when fluid is present behind the eardrum for 12 weeks or more.
Clinical features
Children with OME usually present with hearing loss or recurrent otalgia. Children with a cleft palate or Down’s syndrome have a higher incidence of middle ear effusions. The otoscopic features of OME are characteristic (Fig. 1.13).
The hearing loss is conductive and may fluctuate down to as much as 40 dB. Tympanometry produces a flat trace, indicating an immobile drum (Fig. 1.14).
Treatment
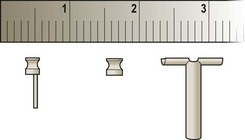
There is as yet no effective long-term medical treatment for established OME. Short-term improvements with antibiotics are not sustained. Decongestant mixtures are ineffective. If the effusion persists, surgery may be required to restore hearing. Removal of the adenoids reduces the incidence of recurrent effusions. Myringotomy, aspiration of fluid and insertion of a ventilation tube (grommet) immediately restores the hearing (Fig. 1.15). Grommets may remain in the drum for up to 12 months before being extruded. After grommet extrusion some children require reinsertion due to recurrent or persisting middle ear effusions.
Otorrhoea after grommets
Hearing loss – general introduction and childhood aetiology
 Childhood hearing loss needs early detection to maximize speech and language acquisition.
Childhood hearing loss needs early detection to maximize speech and language acquisition.
 Screening at 7–8 months used to be mandatory. Test failure requires early referral.
Screening at 7–8 months used to be mandatory. Test failure requires early referral.
 Neonatal screening with otoacoustic emissions is now universal in the UK.
Neonatal screening with otoacoustic emissions is now universal in the UK.
 Middle ear effusions are common, and may be detected by pneumatic otoscopy.
Middle ear effusions are common, and may be detected by pneumatic otoscopy.
 OME may present with otalgia, or may be asymptomatic until hearing loss is suspected.
OME may present with otalgia, or may be asymptomatic until hearing loss is suspected.
 Insertion of grommets is required for persistent otitis media with effusion.
Insertion of grommets is required for persistent otitis media with effusion.
 Otorrhoea due to infected grommets usually resolves with topical treatments.
Otorrhoea due to infected grommets usually resolves with topical treatments.
Hearing loss – adult aetiology
Conductive hearing loss
Ear canal
Wax production varies between individuals and races. Blind attempts to remove wax with cotton buds usually result in impaction. Wax may be properly removed by syringing the ear or with a blunt hook (p. 25). Preliminary softening can be achieved with sodium bicarbonate eardrops three times a day, or hydrogen peroxide. Rarely, excessive accumulations of desquamated skin and wax in the deepest part of the external meatus can expand and erode the ear canal. This is termed keratosis obturans, and an anaesthetic may be required to remove it.
The external canal may be narrowed by bony exostoses predisposing to keratin accumulation (Fig. 1.16). These exostoses often occur in swimmers and require no treatment unless they cause external otitis or hearing deficits.
Eardrum and middle ear
Perforations of the eardrum can occur from trauma and acute or chronic otitis media (Fig. 1.17). The degree of hearing loss depends on the site of the perforation and the extent of middle ear disease.
Adults may suffer with middle ear effusions, although less commonly than children. Investigations should rule out sinusitis, or nasopharyngeal tumours blocking the Eustachian tube (see Fig. 1.12, p. 7).
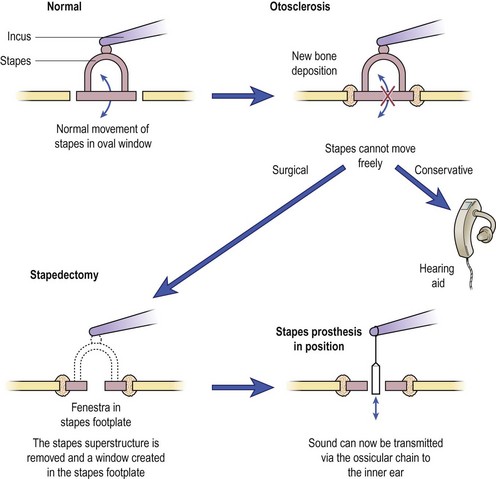
Otosclerosis is a disease where new bone growth occurs in the capsule of the inner ear. This may fix the footplate of the stapes. Hearing loss characteristically develops in the young adult and is usually conductive (p. 3), although the otoscopic appearance of the eardrum is normal. Pregnancy can accelerate the symptoms, suggesting a hormonal association with the disease. A family history is frequently elicited. Tinnitus may also be present.
Surgery for otosclerosis may restore normal hearing but also carries a small risk of total hearing loss. Use of a hearing aid has no complications, but is often refused (Fig. 1.18).
Sensorineural hearing loss
Presbyacusis (common)
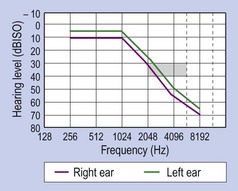
Presbyacusis is a progressive loss of hair cells in the cochlea with age. Roughly 1% of cells are lost each year, and this affects the high-frequency part of the inner ear first (Fig. 1.19). It becomes clinically noticeable from the age of about 60–65 years. The degree of loss varies, as does the age of onset. Some patients with presbyacusis have recruitment (reduced dynamic range of hearing) which reduces effective amplification. The threshold for hearing and the uncomfortable level of sound are abnormally close (e.g. ‘Speak up, I can’t hear you … don’t shout so loud!’). Discrimination may also be affected (‘I hear you but can’t understand you’). There is no treatment to prevent this loss. When a significant social or work handicap is present, a hearing aid may be prescribed. This should be digital so that the pattern of amplification is tailored to the pattern of the individual’s hearing loss. Two hearing aids are better than one, because of binaural hearing.
Acoustic tumours
Acoustic tumours are rare, but treatable, tumours of the vestibular element of the eighth cranial nerve. The most common presentation is a progressive unilateral hearing loss with tinnitus. MRI scanning with gadolinium is the investigation of choice and can demonstrate small tumours (Fig. 1.20). Current treatment options include serial scanning (for small tumours), surgical excision or stereotactic radiosurgery.
Non-organic hearing loss
Hearing loss – adult aetiology
 Wax impaction and presbyacusis are the leading causes of hearing loss in adults.
Wax impaction and presbyacusis are the leading causes of hearing loss in adults.
 Most causes of conductive hearing loss are identifiable on otoscopy.
Most causes of conductive hearing loss are identifiable on otoscopy.
 Otitis media with effusion in adults is rare, so exclude neoplasia of the nasopharynx.
Otitis media with effusion in adults is rare, so exclude neoplasia of the nasopharynx.
 In otosclerosis the eardrum has a normal appearance.
In otosclerosis the eardrum has a normal appearance.
 A progressive unilateral sensorineural hearing loss should be fully investigated to exclude an acoustic neuroma.
A progressive unilateral sensorineural hearing loss should be fully investigated to exclude an acoustic neuroma.
Aids to hearing
Hearing loss is a major disability that can interfere with the social, work and educational spheres of a patient’s life. A 35 dB loss in the speech frequencies (500–2000 Hz) can result in major problems. Fortunately, the majority of sufferers may be helped by employing one or more of the remedies available (Table 1.6).
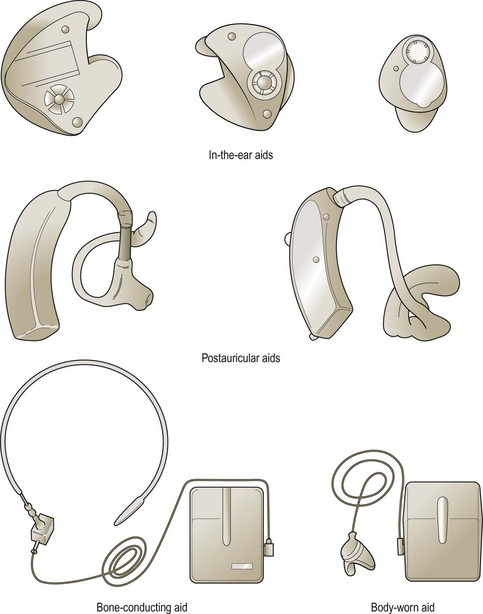
Electronic hearing aids
A variety of aids is shown in Figure 1.21. The majority of patients will be fitted with a postauricular hearing aid which is relatively unobtrusive. However, severe hearing loss may only be assisted by body-worn (BW) aids. It is possible to incorporate the aid into a spectacle frame if desired. Miniaturized aids can also be worn in the ear or inserted into the ear canal.
Problems with electronic hearing aids
The common problems encountered with electronic aids are listed in Table 1.7. Probably the most frequent difficulty is with acoustic feedback. This produces the familiar high-pitched whistle and is particularly seen in patients who require high amplification, and in whom the ear mould allows sound to escape into the microphone. A similar event will occur if the mould is incorrectly inserted, as is frequently seen in elderly people suffering from arthritic joints.
Table 1.7 Common problems with electronic hearing aids
| Problem | Cause |
|---|---|
| Feedback | Badly fitting ear mould |
| Otorrhoea | Ear infection |
| Allergy to mould | |
| No sound | Dead battery |
| Blocked tube |
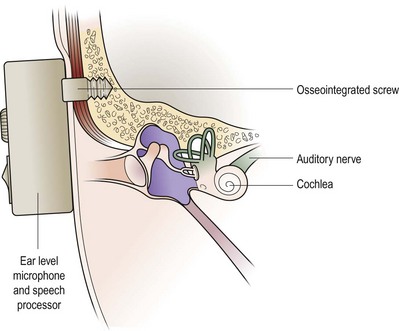
More recent alternatives are bone conduction aids that are anchored in the temporal bone. The external stimulator sets the aid in vibration either across the intervening skin or by a direct percutaneous attachment facility (Fig. 1.22; Fig. 1.53, p. 24). Such aids do not suffer the feedback problems of conventional air conduction aids and also have the advantage of greatly reduced background noise.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree