The Crystalline Lens and Cataract
Dimitri T. Azar
Jose J. de la Cruz Napoli
I. Crystalline lens: Basic anatomy, physiology, and biochemistry
The crystalline lens is a biconvex avascular structure suspended by thin filamentous zonules attached to the ciliary processes between the iris anteriorly and the vitreous humor posteriorly. The lens is the lesser of the two refractive diopteric elements in the eye accounting for approximately 18 D in the unaccommodated state, increasing with accommodation. It is an encapsulated multicellular organ surrounded by a basal lamina and the lens capsule, with an anterior layer of cuboidal epithelium covering concentric layers of fibers (Fig. 7.1). The lens capsule is rich with type IV collagen. The anterior lens capsule is thicker than the posterior capsule and contains another matrix protein, laminin. The epithelial cells contain nuclei, mitochondria, endoplasmic reticulum, and other cytoplasmic organelles; metabolic activity is both aerobic and anaerobic. At the equator, epithelial cells undergo mitotic division and differentiate into lens fibers. With aging and differentiation, all cells are gradually incorporated into the lens by anterior and posterior elongation to form the fiber cells of the lens. Cellular organelles are lost during differentiation. The lens sutures are formed by interdigitation of the anterior and posterior tips of the spindle-shaped fibers. Additional branches are added to sutures as the lens ages. No cells are lost from the lens. Newly laid fibers crowd and compact previous fibers; thus the oldest (embryonic and fetal) layers are the most central. The outermost fibers constituting the lens cortex are the most recently formed fibers. In lens fibers aerobic metabolic activity is absent.
The nucleus, the innermost part of the lens, contains the oldest cells, and metabolic activity in this region is virtually nonexistent. Metabolic activity supports active transport of amino acids and cations across the epithelium as well as protein synthesis in the fibers. Cations move actively across the anterior epithelium, but passively across the posterior lens capsule—a so-called pump–leak system. The maintenance of homeostasis is essential to lens clarity. Physiologic stresses may disrupt this homeostasis and lead to cataract formation, or opacification of the lens.
II. Optics
The lens and cornea form an optical system that focuses light from a distant object on the retina (emmetropia), anterior to the retina (myopia), or posterior to the retina (hyperopia). Myopic and hyperopic refractive errors are corrected with spectacle or contact lenses. The lens has a higher refractive index than its surroundings, resulting from the high concentration of α-, β-, and δ-crystallins in the lens fiber cytoplasm. The ability of the lens to change the refractive power of the eye and focus near objects is called ocular accommodation. The most commonly accepted mechanism of accommodation is that ciliary muscle contraction relaxes zonular tension on the lens and allows the intrinsic elasticity of the lens capsule to increase the central convexity of the anterior lens. This change reduces the focal length of the lens and moves the point of clear vision closer to the eye. When accommodation is relaxed, the equatorial edge of the lens moves toward the sclera (see Chapter 9 and Chapter 14). The accommodative response resulting from the same amount of ciliary muscle contraction, or accommodative effort, may vary depending on the age of the patient. It may be expressed as the diopteric change of lens power (amplitude of accommodation) or as the distance between the far point and the near point of the eye (range of accommodation).
Infants possess great powers of accommodation; with age, this power decreases. By about age 40 years, a substantial amount of accommodative power has been lost,
and reading glasses are needed for clear near vision. This is known as presbyopia, which is one of the earliest age-related lenticular changes. The amplitude of accommodation is helpful to calculate the power of the add used in bifocal spectacles to correct presbyopia.
and reading glasses are needed for clear near vision. This is known as presbyopia, which is one of the earliest age-related lenticular changes. The amplitude of accommodation is helpful to calculate the power of the add used in bifocal spectacles to correct presbyopia.
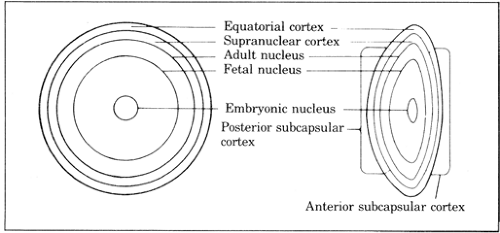 Figure 7.1. Anatomic layers of the crystalline lens. Between the fetal and adult nuclei lie the lamellae of the infantile and adolescent nuclei. |
In addition to presbyopia, ultrastructural deterioration and various biochemical changes of the crystalline lens take place with aging. The lens nucleus also becomes increasingly yellow with age (nuclear sclerosis), and in some cataracts the nuclear color may be brown or black. Nuclear sclerosis per se is not associated with loss of clarity. Often it is associated with an increase in the refractive index of the lens and a myopic shift in refraction, known as lenticular myopia. A change in color perception may result from the superimposition of a yellow filter between the retina and the incident light.
III. Age-related changes
Age-related cataracts are a major cause of visual impairment in older adults. When the transparency of the crystalline lens decreases enough to disturb vision, a clinically significant cataract exists. Such a decrease is usually the result of scattering of light rays or absorption in the axial part of the lens; similar changes in the peripheral parts of the lens may exist without loss of vision. Although these changes in the periphery are strictly cataractous in nature, surgical intervention is rarely warranted in the absence of visual symptoms.
A cataract is characterized by the zones of the lens involved in the opacity: anterior and posterior subcapsular, anterior and posterior cortical, equatorial cortical, supranuclear, and nuclear. In certain congenital cataracts, the nuclear zone is further subdivided into adult, adolescent, infantile, fetal, and embryonic zones (Fig. 7.1). There is a gradual transition but no distinct morphological differentiation between the layers of a cataract. The distinctions between these regions relate primarily to potential differences in their behavior and appearance during surgical procedures.
Epidemiology of cataracts. Ninety-five percent of individuals older than 65 years of age have some degree of lens opacity; many have cataracts sufficiently dense to warrant cataract extraction. The Beaver Dam Eye Study reported that 38.8% of men and 45.9% of women older than 74 years had visually significant cataracts. It is estimated that more than 1 million cataract extractions are performed each year in the United States alone. Cataract accounts for more than 15 million cases of treatable blindness in the world; extraction often leads to complete visual rehabilitation. The Baltimore Eye Survey showed that untreated cataract was the source of blindness in 27% of African Americans and 13% of whites.
Optics of cataracts. Visual disturbances resulting from a cataractous lens are secondary to fluctuation in the index of refraction creating light scattering and/or a loss of transparency. In cortical, supranuclear, and subcapsular cataracts,
protein-deficient fluid collects between fibers. The index of refraction of this fluid is much less than that of fiber cytoplasm, and light scattering occurs at this interface. Light scattering also occurs from large protein aggregates linked to the cell membrane by disulfide bonds. This may cause monocular diplopia. Progressive yellowing of the lens in nuclear sclerotic cataracts causes poor hue discrimination, particularly at the blue end of the visible spectrum. The myopic shift associated with nuclear cataracts may transiently enable presbyopic patients to read without spectacles, a condition referred to as “second sight.”
IV. Evaluation and management of cataracts
Symptoms of cataract formation
Decreased vision. Cataracts cause painless progressive decrease in vision. Clinically significant cataracts cause a decrease in distance or near visual acuity. Posterior subcapsular cataracts of even mild degree can reduce visual acuity substantially. Nuclear sclerotic cataracts cause image blur at distance but not near. Image blur occurs when the lens loses its ability to differentiate (resolve) separate and distinct object points. When this occurs, near visual tasks, such as reading and sewing, become more difficult. Many older patients may tolerate considerable reductions in distance acuity if their night driving is minimal, but they may not be as tolerant of a blur that interferes with their indoor activities.
Glare. One of the symptomatic manifestations of light scattering is glare. When a patient looks at a point source of light, the diffusion of bright white and colored light around it drastically reduces visual acuity. The effect is akin to looking at automobile headlights at night through a dirty windshield. Posterior subcapsular opacification is responsible for much of the glare.
Distortion. Cataracts may make straight edges appear wavy or curved. They may even lead to image duplication (monocular diplopia). If a patient complains of double vision, it is essential to determine whether the diplopia is binocular or monocular. If monocular, the examiner is usually dealing with corneal, lenticular, or macular disease.
Altered color perception. The yellowing of the lens nucleus steadily increases with age. Artists with significant nuclear sclerosis may render objects more brown or more yellow than they actually are.
Unilateral cataract. A cataract may occur in only one eye or may mature more rapidly in one eye than in the other. Unless the patient is in the habit of checking the acuity of each eye, he or she may not be aware of the presence of a dense cataract in one eye. It is not uncommon for a patient to claim that the vision in the cataractous eye was lost precipitously. Because cataracts rarely mature precipitously, it is more likely that the slowly evolving lens opacity was unrecognized until the patient happened to test his or her monocular acuity.
Behavioral changes
Children with congenital, traumatic, or metabolic cataracts may not verbalize their visual handicap. Behavioral changes indicative of a loss of acuity or binocular vision may alert the parents or teachers to the presence of a visual problem. Inability to see the blackboard or read with one eye may be one such symptom; loss of accurate depth perception (e.g., the inability to catch or hit a ball or to pour water from a pitcher into a glass) may be another.
Prepresbyopic adults. Difficulty with night driving is frequently an early sign of cataract.
Presbyopic adults. Frequently, maturation of nuclear cataracts is associated with the return of clear near vision as the result of increasing myopia secondary to the higher refractive power of the rounder, harder nuclear sclerotic lens. Reading glasses or bifocals are no longer needed. This change is called “second sight.” Unfortunately, the improvement in near vision is only temporary as the nuclear zone becomes more opaque.
Signs of cataract formation
Reduced visual acuity. Although it is not part of the usual general physical examination, the measurement of visual acuity will alert the examiner to the
presence of cataract as well as other ocular disorders. The examiner should always inquire about monocular acuity when conducting a review of systems.
Lenticular opacification. Examination of the red reflex with the direct ophthalmoscope set on +5 (black) D at approximately 20 cm from the patient frequently will reveal a black lens opacity against the reddish-orange hue of the reflex. This is an extremely sensitive method of detecting cataractous change. If on upgaze the opacity appears to move down, the opacity is in the posterior half of the lens; if the opacity moves up with upgaze, it is located in the anterior half of the lens or in the cornea.
Leukokoria. The white pupil is seen in mature cataracts; in certain immature cataracts, whitish patches are seen in the pupillary zone, the result of foci of light scattering, located in the anterior subcapsular or cortical zone.
Diagnostic tests and spectacle correction for cataract
Uncorrected and spectacle-corrected Snellen visual acuity. Distant and near acuity with and without the appropriate glasses should be tested. Some patients with cataracts complain of poor visual function despite good Snellen visual acuity. Snellen charts measure high-contrast visual acuity. Cataracts can cause decreased appreciation of contrast, leading to subjective visual dysfunction. Snellen visual acuity in a brightly lit room versus a dark room may be substantially worse secondary to glare.
Non-Snellen acuity. Tests of contrast sensitivity may be used to objectively document subjective decrease in contrast, although they have yet to be widely standardized for this purpose. Cataracts, especially posterior subcapsular and cortical, may cause debilitating glare. Several readily available instruments can document the effect of glare on visual acuity (e.g., brightness acuity testing). Confrontation visual fields and Goldmann and automated visual field testing may be valuable to evaluate the degree of preoperative visual field loss. Potential acuity meter (PAM) testing can be helpful in evaluating the lenticular contribution to visual loss. Similarly, laser interferometry is predictive of final visual acuity in moderately dense cataracts. In severe cataracts, underestimation of potential vision may occur more often with PAM than with laser interferometry. For eyes with concomitant retinal disorders, the laser interferometer may overestimate the potential vision more than the PAM test. The illuminated near card (INC) test is a reliable tool of potential vision testing in eyes with cataract when the preoperative distance vision is 20/100 or better. In addition, in eyes with dense cataracts, a prediction of 20/40 or better with the INC can be a reliable index of good vision potential.
Flashlight examination of lens and pupil. The direct and consensual pupillary responses are not affected by lens opacities if a bright light is used; if a dim flashlight is used, the responses may be less pronounced when illuminating the eye in the presence of a dense cataract. A flashlight may also render anterior lens opacities more visible to the examiner if pupil size is not reduced excessively.
Direct ophthalmoscopy. With the pupil dilated, nuclear cataracts often appear as a lens within a lens when viewed against the red reflex with a +5 D to +10 D lens.
Slitlamp biomicroscopy allows the most detailed examination of the anterior part of the eye. The extent, density, type, and location of the cataract can be easily determined. Slitlamp examination is also helpful in determining the position of the lens and the integrity of the zonular fibers. Excessive distance between the lens and the pupillary margin may indicate lens subluxation. Slitlamp biomicroscopy may have limitations, especially in detecting oil droplet cataracts, which may be easier to detect using the direct ophthalmoscope through the 10 D lens.
Refraction and retinoscopy. Myopia induced by the early stages of nuclear cataract formation can be detected by routine refraction. Patients may be well corrected for years with a stronger myopic distance lens and reading add. Retinoscopy will reveal the abnormal reflexes associated with lenticonus, a condition in which the anterior or posterior surface of the lens (or both) is excessively convex or conical.
Fundus evaluation. Both the direct and indirect ophthalmoscope can be used to evaluate the anatomic integrity of the posterior segment. Dilated fundus examination is necessary to evaluate the macula, optic nerves, vitreous, retinal vessels, and retinal periphery. Attention to macular degeneration, diabetic retinopathy, macular edema, retinal ischemia, vitreoretinal traction, neovascularization, optic nerve pallor, extensive cupping, and posterior capsular ruptures is important because these conditions may limit visual rehabilitation after cataract surgery.
A- and B-scan ultrasonography are techniques for measuring the thickness and location of a cataract. A-scan ultrasound techniques to measure the eye’s axial length paired with keratometric measurement of corneal curvature allow precise calculation of appropriate intraocular lens (IOL) power, thus minimizing postoperative spherical refractive error. B-scan techniques are particularly useful in evaluating partial or total dislocation of the lens and also provide a means of detecting abnormalities in the posterior half of the eye in the presence of a very dense cataract that precludes direct visualization. Ultrasound biomicroscopy (UBM) also allows direct visualization of zonular support in cases in which zonular integrity is in question. Some secondary cataracts form in response to posterior segment tumors or inflammation, thereby necessitating ultrasonography to ascertain the anatomic state of the eye behind the lens (see Chapter 1).
V. Abnormalities of the lens
Homocystinuria. This autosomal-recessive condition is associated with a deficiency of cystathionine beta-synthetase, an enzyme responsible for condensing homocystine and serine to cystathionine. Bilateral lens dislocation occurs in this disease; if the lens dislocates into the anterior chamber, acute pupillary block glaucoma may develop. Cataractous changes are unusual. Systemic manifestations include malar flush, mental retardation, osteoporosis, pectus excavatum, decreased joint mobility, and eczema. Abnormal physical findings are usually apparent by age 10 but may be delayed until the third decade. Surgical removal of dislocated lenses is fraught with complications, including vitreous loss, iris prolapse, and retinal detachment. General anesthesia is to be avoided, if possible, because of the increased risk of vascular thrombosis.
Marfan syndrome. Inheritance of this disorder is autosomal dominant. In contrast to homocystinuria, in which lens dislocation is usually inferior, in Marfan syndrome dislocation is superior and only occasionally into the anterior chamber. Surgical extraction of these lenses is complicated by many of the same problems encountered in homocystinuria. The systemic manifestations of this disease include a tall and thin body habitus, scoliosis, arachnodactyly, elastic skin, hyperextensible joints, aortic insufficiency, and aortic aneurysm. Abnormalities in the expression of fibrillin have been found in some patients with Marfan syndrome. The diagnosis is usually established by the physical examination and the characteristic patient habitus.
Weill-Marchesani syndrome is inherited as an autosomal-dominant or -recessive trait. Patients are short with broad hands and fingers. There may be joint stiffness, prominence, and decreased mobility. Carpal tunnel syndrome may result from fibrous tissue hyperplasia. Lenses are small, spherical, and frequently dislocate anteriorly, precipitating acute glaucoma. Patients are easily distinguished from those with Marfan syndrome or homocystinuria by their characteristic body habitus.
Other heritable conditions with ectopia lentis include hyperlysinemia, Crouzon syndrome, oxycephaly, Sprengel deformity, sulfite oxidase deficiency, Sturge-Weber syndrome, Ehlers-Danlos syndrome, dwarfism, polydactyly, and mandibulofacial dysostosis.
Traumatic dislocation. During ocular injuries, particularly blunt ocular trauma, expansion and compression of the globe equator can lead to lens dislocation or subluxation. The direction of dislocation could be vertical, horizontal, anterior
(into the chamber) or posterior (into the vitreous). Very often this condition is associated with traumatic mydriasis, vitreous prolapse, rosette-shaped cataract formation, blood in the anterior chamber (hyphema), and glaucoma.
Galactosemia is the result of an autosomal-recessive inborn error of galactose metabolism, a deficiency of galactose-1-phosphate uridyltransferase, the enzyme that converts galactose-1-phosphate to uridine diphosphogalactose. In the presence of milk sugar (lactose), this deficiency leads to the accumulation of galactose-1-phosphate and galactose. Galactose is converted by the enzyme aldose reductase to the sugar alcohol, galactitol. The accumulation of this sugar alcohol within lens cells creates a hypertonic intracellular milieu that is neutralized by the influx of water. The entry of water leads to swelling, membrane disruption, and opacification of the lens. Cataracts are not apparent at birth but usually develop within the first few months of life. A central nuclear opacity resembling a drop of oil appears within the lens. This opacity may progress to opacification of the fetal nucleus. The disease is manifest in patients fed milk products that contain the disaccharide lactose (glucose plus galactose). Mental retardation, growth inhibition, and hepatic dysfunction commonly ensue if the disease goes untreated. The diagnosis can be made by an assay for uridyltransferase in peripheral red cells.
Galactokinase deficiency. The enzyme galactokinase converts galactose to galactose-1-phosphate. In this autosomal-recessive disorder, lack of this enzyme leads to the accumulation of galactose, which is then converted to galactitol. The same osmotic events as in galactosemia occur and lead to cataract formation. Systemic manifestations of galactosemia are absent, however. Except for cataracts, these patients usually enjoy normal health. Treatment is dietary restriction of galactose-containing foods. Patients who are heterozygous for this genetic defect are also at increased risk of cataract formation during the first year of life.
Hypoglycemia. Neonatal hypoglycemia occurs in approximately 20% of newborns. The incidence is significantly increased in premature infants. Blood sugars of 20 mg/dL or less may cause repeated episodes of somnolence, diaphoresis, unconsciousness, and convulsions. Repeated hypoglycemic episodes may lead to a characteristic lamellar cataract in which layers of cortical opacity are separated from a deeper zonular cataract by clear cortex. The cataract does not usually appear until the child is at least 2 to 3 years old; in many patients, no visual disability is encountered. Experimental evidence suggests that this cataract may be the result of an inactivation of type II hexokinase. Treatment of this condition is aimed at the restoration and maintenance of normal glucose levels in the blood.
Lowe syndrome (oculocerebral renal syndrome). Bilateral nuclear cataracts and microphakia are always found in this X-linked recessive disorder. Aspiration of these cataracts is associated with a poor prognosis for full visual recovery. Other ocular abnormalities include glaucoma and malformation of the anterior chamber angle and iris. Most striking is the blue sclera, a manifestation of scleral thinning. Frequently, there is associated mental retardation, failure to thrive, absence of eyebrows, and vitamin D–resistant rickets. Vomiting, glucosuria, proteinuria, renal caliculi, and convulsions are not unusual. The exact biochemical defect is unknown. Female genetic carriers have punctate cortical opacities.
Myotonic dystrophy is inherited as an autosomal-dominant trait and is the result of a defect in the gene encoding myotonin protein kinase; the defective gene contains increased repeats of a trinucleotide sequence. Early cataracts are characteristic and consist of fine, scattered, dustlike opacities in the cortex and subcapsular region. Multicolored (especially red and green) refractile bodies are scattered among these finer dustlike opacities; this finding is commonly referred to as a “Christmas tree” cataract. Later in the disease, a granular, posterior subcapsular cataract develops. Cataract extraction usually is performed in adulthood, and the visual prognosis is good if there is no serious posterior segment abnormality such as optic atrophy or retinal degeneration. Associated systemic findings include dystrophic changes in muscles, including impaired contraction and relaxation, gonadal atrophy, and frontal baldness.
Rubella cataract results from fetal infection with rubella virus before the ninth week of gestation. This virus is known to inhibit mitosis and cell division in many fetal tissues. Involvement of the lens vesicle at the time of elongation of the posterior epithelial cells leads to abnormal lens development. The cataract has a characteristic morphology: slightly eccentric, dense, white core opacity and lesser opacification of the surrounding cortex. The anterior suture may be visible. Other ocular manifestations of this disease are microphthalmos, pigmentary retinopathy, and iritis. Because of the involvement of dilator fibers, pupillary dilation is frequently incomplete. Early referral to an ophthalmologist will optimize chances for successful cataract extraction. Surgery is frequently difficult because of poor pupillary dilation, shallow anterior chamber depth, and the small size of the eye. The newest techniques, however, with phacoemulsification and other forms of cataract aspiration, give this procedure a better prognosis. Rubella prevention, through vaccination, probably offers the safest and most effective method of reducing the incidence of this disease.
Other congenital abnormalities in which cataracts are found include Werner syndrome, congenital ichthyosis, Rothmund-Thomson syndrome, Fabry disease, incontinentia pigmenti, Refsum disease, gyrate atrophy of the choroid and retina, Stickler syndrome, neurofibromatosis type II, cerebrotendinous xanthomatosis, Wilson disease, Niemann-Pick disease Type A, mannosidosis, mucolipidosis I, and Hallermann-Streiff-François syndrome (see Chapter 10).
Age-related cataracts. The term senile was previously used to describe cataracts in older adults with no specificity with regard to morphology or etiology. However, with the emergence of surgical procedures specifically suited to certain forms of cataracts, it has become more important to specify the degree of nuclear sclerosis, which often correlates with hardness, when distinguishing one form of cataract from another. Typically, cataracts are now described by their cortical, nuclear, and subcapsular components.
Metabolic cataract
Diabetic cataract
Osmotic cataract. In the pre-insulin era, the acute onset of a mature cataract in an untreated or brittle diabetic was not uncommon. Because blood sugar control is now relatively easy with insulin, this form of acute osmotic cataract is extremely rare. It is possible to precipitate this cataract, however, by abruptly lowering a markedly elevated blood sugar with insulin. The intracellular hypertonicity, which results from the accumulation of sorbitol and glucose, remains after the serum osmolarity decreases precipitously with the blood sugar. A rapid influx of water leads to acute swelling and opacification of the lens.
Poorly controlled diabetics frequently experience changes in their refractive status. Increasing blood sugar is associated with myopic change; decreasing blood sugar is associated with hyperopic change. These changes are most noticeable during periods of poor control. Restoration of control eliminates these refractive error fluctuations.
The reversible appearance and disappearance of a posterior subcapsular cataract
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


