Anterior laryngeal webs can be congenital or acquired and occur secondary to a surgical procedure, intubation, or infection. Clinical presentation can include vocal and respiratory symptoms. The first step in managing a laryngeal web is performing flexible laryngoscopy, followed by a direct laryngoscopy under general anesthesia. Treatment remains a challenge. Endoscopically, the web can be incised with cold instruments or by laser, mitomycin-C can be applied, and a silastic keel can be inserted in the anterior commissure. Externally, an anterior cricothyrotomy is necessary and a silastic keel can be placed; anterior cartilage graft can be inserted in case of a thick web. Regardless of the technique used, the primary concern is recurrence.
Anterior laryngeal webs are generally congenital defects but may be acquired secondary to a surgical procedure, intubation, or infection ( Corynebacterium diphtheriae or Bacillus cereus ) . Management is different because congenital webs are considered to be a form of congenital laryngeal stenosis or atresia, and a with a web needs to undergo a general clinical evaluation for other congenital defects. The surgical management of congenital and acquired webs is similar, but local associated malformations, such as posterior clefts, can make congenital webs more difficult to treat.
A congenital web is a rare malformation in which abnormal fibrous tissue forms between two structures within the larynx. Its most common anatomic localization is at the level of the glottis extending across the anterior one third of the vocal cords, but it can extend from varying degrees toward the posterior glottis and inferiorly to the subglottis. This malformation results from incomplete recanalization of the primitive larynx during the tenth week of embryogenesis . When the embryo is at approximately 33 days’ development, an epithelial structure, the epithelial lamina, obliterates the ventral lumen of the primitive larynx. A posterior communication remains between the pharynx and the trachea: the pharyngotracheal duct. Walander (cited by Cohen ) reported that during the eighth developmental week, the vocal cords appear and serve as a mucosal lining; the false vocal cords also appear above the true vocal cords and mark the upper border of the ventricles. At the same time, the cricoid duct widens until the lower part of the vocal cords has been reached.
Also during the eighth week, the larynx starts to recanalize from caudal to cranial . This process of recanalization is most active in the dorsal part of the epithelial lamina and starts in the ventral direction from the pharyngotracheal duct . More recent studies of laryngeal embryology have examined the origin of the infraglottic cavity. According to Zaw-Tun, the primary pulmonary sac is the entire primordium of the infraglottic cavity. Sañudo suggests that it is the primordium of only the cartilaginous region of the infraglottic cavity . The importance of the web is linked to the time at which the process of recanalization ends. The congenital anterior laryngeal web is one part of the spectrum of this developmental defect—the most important part being the laryngeal atresia. In case of an acquired web, the history can be that of infection, intubation, trauma, reflux, or laryngeal surgery (especially when laser is used). The association of these two factors—laryngeal laser procedures and reflux—is recognized as a significant risk factor for the formation of webs .
Clinical presentation and anatomic findings
Symptoms can vary from an isolated weak cry or voice to an acute respiratory distress. Some cases of adult patients with symptom-free laryngeal web have been reported , showing that if the web is small enough, it can be found in adulthood during anesthetic intubation. The presenting complaint is usually associated with symptoms such as an abnormally weak, soft, husky, or absent cry since birth , stridor (usually biphasic and worsened in exertion), recurrent croup, and episodic cyanosis . Cohen also reported recurrent tracheobronchitis and recurrent pneumonia in 9 of 51 patients, noting that the symptoms were initially mild and increased subsequently with trauma or inflammation. In their series of 21 patients, Wyatt and Hartley found that more than one symptom was usually reported.
Although in some cases the web is an isolated finding, in others it presents with associated congenital defects, with chromosomal and cardiovascular anomalies being the most common . The diagnosis of congenital webs is usually made during the first months of life but can vary from birth to many years of age , depending on the clinical presentation. In general, the more severe the respiratory symptoms, the sooner a diagnosis is made. When a child presents with a clinical history that suggests a web, the initial examination is with fiberoptic laryngoscopy. During the fiberoptic examination, the nasal surface of the soft palate also should be examined carefully for a submucosal cleft. Abnormal pulses of a medialized internal carotid artery behind the muscular wall of the nasopharyngeal midline also should be sought. Both of these findings are variably observed in children with chromosome 22q11 deletion (velo-cardio-facial syndrome and DiGeorge’s syndrome) . With the scope advanced to the hypopharynx, examination of the larynx should include evaluation of vocal cord mobility, swallowing, thickness of the web, size of the subglottic lumen, and presence of a posterior cleft in the interarytenoid notch. Other aspects of the otorhinolaryngologic evaluation should include an oral inspection for submucosal cleft or a bifid uvula, which may be the only other obvious manifestation of a 22q11 deletion.
The second step of the anatomic evaluation is endoscopy under general anesthesia, which allows a complete and accurate staging of the web. The entire airway is observed from the larynx through the mainstem bronchi. The mucosa of the anterior web is palpated to assess thickness and firmness of the tissues, and the interarytenoid area and tracheoesophageal septum are probed for a posterior cleft.
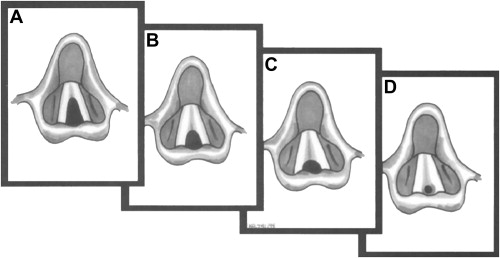
Two classifications are currently used for staging: Cohen’s and Benjamin’s , which are being designed for congenital lesions. Cohen’s classification defines types 1 through 4, depending on the degree of glottic narrowing ( Fig. 1 ). Type 1 anterior webs involve 35% or less of the glottis and are of uniform thickness and free of subglottic extension. Type 2 webs involve 35% to 50% of the glottis and may be thin or moderately thick. Type 3 webs involve 50% to 75% of the glottis and are usually thick anteriorly and thinner posteriorly. Type 4 webs involve 75% to 90% of the glottis, are uniformly thick, have vocal cords that are not identifiable, and have a subglottis lumen that is narrowed by the thickness of the web extending inferiorly. It should be noted that types 2 and 3 may extend into the subglottis and have an associated subglottic stenosis.
Benjamin’s classification defines four degrees of laryngeal atresia according to their anatomic localization. This classification consists of glottic webs, subglottic webs, congenital interarytenoid fixation, and supraglottic webs. It seems that the two classifications can be used concurrently to define a lesion. When there is a simultaneous laryngeal stenosis, the Myers-Cotton classification can be used to further define the problem. The discovery of a web mandates a systemic evaluation to rule out other congenital anomalies.
Management
The initial diagnostic evaluation has three aims: to (1) define whether the web is present and, if so, whether it is congenital or acquired, (2) look for associated anomalies, and (3) determine the best surgical and anesthetic options for reconstruction.
The time of onset of symptoms must be ascertained accurately, particularly if there is any history of laryngeal infections or trauma. If no such history exists, then the web is presumed to be congenital. With congenital webs, a multidisciplinary team that consists of a geneticist, pediatric cardiologist, and pediatric pulmonologist needs to become involved with the child. Cohen reported that 51% of patients had associated abnormalities. McElhinney and colleagues found that a significant number of patients with congenital laryngeal web had a diagnostic triad that consisted of the web, congenital cardiovascular disease, and a chromosome 22q11 deletion. Associated cardiovascular anomalies include vascular rings, ventricular septal defects, valvular atresia, and more complex malformations, such as tetralogy of Fallot hypoplastic or left heart syndrome . When there is an associated laryngeal cleft, the consultation team needs to be expanded to include a pediatric gastroenterologist and speech therapist for swallowing evaluation and management.
Imaging is rarely needed for the web itself but may be necessary for defining the degree of subglottic narrowing or a more complete evaluation of other associated anomalies. Benjamin reported in 1983 that xeroradiographs of the upper airway may give valuable information about the thickness of the web and the presence of an associated subglottic stenosis. Xeroradiography is no longer used; however, a fine cut CT scan is a contemporary alternative for laryngotracheal evaluation. The fine cut axial and coronal images and three-dimensional virtual endoscopy may help identify narrowing of the subglottic lumen . These technologies are particularly useful in children with complete atresia and provide the physician with precise information about the length and degree of stenosis. Unfortunately, technology does replace direct visual analysis, particularly of the evaluation of the airway mucosa and the degree of inflammation.
Management
The initial diagnostic evaluation has three aims: to (1) define whether the web is present and, if so, whether it is congenital or acquired, (2) look for associated anomalies, and (3) determine the best surgical and anesthetic options for reconstruction.
The time of onset of symptoms must be ascertained accurately, particularly if there is any history of laryngeal infections or trauma. If no such history exists, then the web is presumed to be congenital. With congenital webs, a multidisciplinary team that consists of a geneticist, pediatric cardiologist, and pediatric pulmonologist needs to become involved with the child. Cohen reported that 51% of patients had associated abnormalities. McElhinney and colleagues found that a significant number of patients with congenital laryngeal web had a diagnostic triad that consisted of the web, congenital cardiovascular disease, and a chromosome 22q11 deletion. Associated cardiovascular anomalies include vascular rings, ventricular septal defects, valvular atresia, and more complex malformations, such as tetralogy of Fallot hypoplastic or left heart syndrome . When there is an associated laryngeal cleft, the consultation team needs to be expanded to include a pediatric gastroenterologist and speech therapist for swallowing evaluation and management.
Imaging is rarely needed for the web itself but may be necessary for defining the degree of subglottic narrowing or a more complete evaluation of other associated anomalies. Benjamin reported in 1983 that xeroradiographs of the upper airway may give valuable information about the thickness of the web and the presence of an associated subglottic stenosis. Xeroradiography is no longer used; however, a fine cut CT scan is a contemporary alternative for laryngotracheal evaluation. The fine cut axial and coronal images and three-dimensional virtual endoscopy may help identify narrowing of the subglottic lumen . These technologies are particularly useful in children with complete atresia and provide the physician with precise information about the length and degree of stenosis. Unfortunately, technology does replace direct visual analysis, particularly of the evaluation of the airway mucosa and the degree of inflammation.
Treatment
The history of the recognition, evaluation, and management of laryngeal webs has been reviewed by Cohen and McHugh and Loch , and the following narrative is based on their reports. The first case of a laryngeal web was described by Fleischmann in 1820 after performing an autopsy on a 27-day-old infant. In 1869, Zurhelle described the first living case, diagnosed by indirect laryngoscopy, in an 11-year-old boy who presented with voice anomaly. In 1889, Seiffert reported a familial cohort involving a father, son, and two daughters. The first attempt at treatment is attributed to Von Schroetter, who tried to correct an anterior web by dilating the lesion with a hard rubber tube. In 1935, Iglauer tried inserting a ring in the anterior commissural region. Subsequently, a wide variety of other materials, such as polyethylene, tantalum, and silastic, with differing shapes and configurations have been used as keels to prevent reformation at the apex of the webs. In 1932, Tucker performed a laryngoscopic removal of a double web (glottic and subglottic) but resorted to a tracheotomy postoperatively to control the airway. In 1955, Holinger reported a series of 19 children with webs who had incision, resection, and dilatation, with 3 children requiring tracheotomy. In 1967, Holinger updated his series by describing 24 patients with laryngeal webs, and he proposed a hierarchy of intervention depending on the severity of obstruction, advocating simple lysis of the thin translucent variety of webs. Three years later, he advocated treating the thin webs by dilatation and inserting a tantalum keel through anterior thyrotomy. In 1975, Walsh-Waring proposed the insertion of a silastic keel through an external approach and concluded that whatever the treatment, a long-term tracheotomy was the best procedure to recommend in case of severe laryngeal web with airway obstruction. The same year, Holinger reported the case of a patient with simultaneous glottic and supraglottic webs treated with laryngofissure and placement of two keels, one of tantalum and the other of silicone elastomer .
Historically, the evolution of surgery generally begins with the goal of saving a life followed by efforts to preserve function. With laryngeal webs, questions regarding voice quality after surgical reconstruction began to be addressed well after the airway management issues had become systematized. In 1983, Benjamin reported a series of 29 patients with congenital webs treated in various ways (incision, dilatation, laser implemented or not by dilatation) and expressed doubt about successful rehabilitation of the voice when the webs were thick. In 1985, Cohen stated that vocal dysfunction was the second of the two major concerns in the results of laryngeal webs treatment, the first being airway obstruction. In his series of 40 patients, he found that the poorest voices were in patients with thick, sheet-like webs, in whom the anatomic specificity of the vocal ligaments was not visible preoperatively. Patients with initial aphonia or poor voice quality generally had poor voice quality postoperatively and required vocal rehabilitation.
The surgical goals in managing laryngeal webs are the same as they have always been: to resolve the airway obstruction and provide a serviceable voice. We are fortunate to have new tools, drugs, surgical techniques, and intensive care units available to help reach the goals of which our pioneering predecessors could only dream. The carbon dioxide (CO 2 ) laser was developed for laryngeal surgery by Jako in 1972. It is an accurate and efficient tool that precisely cuts and ablates tissue with minimal surrounding tissue injury. An alternative to the complex optical delivery system of the original CO 2 laser is the new flexible delivery system that has recently become available. Other laser systems, such as the solid-state KTP laser (Potassium-Titanyl-Phosphate) and the thulium laser, have further expanded our surgical options .
Mitomycin-C (MMC) is an antitumor antibiotic isolated from streptomyces that has antineoplastic activity by inhibiting RNA and protein synthesis . It was first used in 1963 by Kunimoto and Mori for controlling scars in the treatment of a pterygium . Since then it has been widely used in ophthalmologic practice to reduce scar formation in glaucoma surgery. Recognizing that the antiscarring effect of MMC may have use in laryngeal surgery, Ward introduced its use to our field in 1998. Currently it is used to repair choanal atresia and for sinus and laryngotracheal surgery .
Another major step forward in the management of laryngeal webs came with the evolution of techniques of laryngotracheal reconstruction with rib cartilage grafts, originally developed by Cotton and widely used for acquired laryngeal stenosis . As reported by Wyatt and colleagues , many cases may require laryngo-tracheal reconstruction with a cartilage graft. Advances in endoscopic microlaryngeal surgery , improved anesthetic techniques, and better understanding of postoperative care, including the management of acid reflux, allow us to perform more procedures in more cases.
An algorithm for how we manage laryngeal webs is provided in Fig. 2 . As one can see, several options are available depending on the severity of the web: (1) observation, (2) endoscopic approach, and (3) open approach.




