Purpose
To investigate the longitudinal subjective and objective visual functional results in adult cataract patients younger than 65 years at surgery. To evaluate the 10-year cumulative incidence of neodymium–yttrium-aluminum-garnet (Nd:YAG) laser treatment.
Design
A prospective, longitudinal, population-based cohort study.
Methods
The study comprised 116 patients younger than 65 years who had cataract surgery during 1 year at Norrlands University Hospital, Umeå, Sweden. Most patients (94%) had received implantation with a hydrophobic acrylic intraocular lens. Evaluated were visual acuity (VA) and visual function questionnaire (VF-14) results before and after surgery. A comparison with patients 65 years or older at surgery was made. Ten years later, 102 survivors were offered eye examinations and again asked to fill out the questionnaire. Past Nd:YAG laser treatment, as well as high- and low-contrast VA results, were analyzed.
Results
Ten years postoperatively, 37% of the patients under 65 at surgery had been treated with Nd:YAG in comparison to 20% of the older patients. The cumulative incidence for not having Nd:YAG over 10 years was 72% for those under 65 and 85% for the patients 65 years or more at surgery. Eighteen percent of the younger patients had lost more than 0.1 logarithm of the minimal angle of resolution (logMAR) units of the operated eye, compared with 37% of the older ( P = .00003). A reduction in VF-14 score of 10 points or more was found in 9% of the younger and 28% of the older cataract surgery patients ( P = .00004).
Conclusion
Ten years after surgery, subjective and objective visual function remained stable in most patients younger than 65 years at surgery. More than one-third had received a posterior capsulotomy. Only a few patients with posterior capsular opacification requiring Nd:YAG were untreated at the 10-year follow-up.
Modern cataract surgery is a procedure after which most patients expect perfect visual rehabilitation. Intraocular lens (IOL) implantation is also a refractive procedure often performed in relatively young patients. With the tendency to operate on patients at an earlier stage of cataract development, the pseudophakic lifespan may be longer than previously.
Research on the long-term clinical outcome after phacoemulsification in younger patients is limited. Dholakia and associates studied 54 patients younger than 50 years at surgery with a follow-up time of 3 years, but without data on the subjective visual function. Focusing on the risk for retinal detachment, Chen and associates presented a study on 35 patients aged 32 to 45 years with a follow-up of 1 to 6 years.
The surgical technique for cataract extraction has changed substantially in the past years, leading to excellent outcomes. New implant technologies promise to improve the image quality, and a smaller incision size shortens the time for wound healing and reduces the risk for postoperative astigmatism. The short-term incidence of posterior capsule opacification (PCO) has declined with the development of small-incision phacoemulsification techniques and foldable intraocular lenses, with square edge and better IOL materials. However, PCO is still a significant long-term complication of cataract extraction, with lower age associated with a greater risk. The PCO rates have been documented to be as high as 25% in the first 5 years postoperatively. Neodymium–yttrium-aluminum-garnet (Nd:YAG) laser is the treatment of choice for PCO, and the procedures may cause a relatively large public health-care burden. When comparing surgical costs in the United States, only the original cataract/IOL procedure is more expensive.
Historically, the outcomes of cataract surgery have been assessed in terms of visual acuity (VA), of which the short-term benefits are well known. However, it has been recognized that the patients’ self-assessed visual ability before and after surgery is a better measure of the surgical result than VA alone.
This prospective study aimed to evaluate the longitudinal outcomes of cataract surgery in adults under the age of 65 at surgery, focusing on changes in self-assessed subjective visual function, best-corrected VA (BCVA), and cumulative incidence of PCO 10 years postoperatively.
Methods
Study Population
All patients who had cataract surgery between June 1, 1997, and May 31, 1998, at Norrlands University Hospital in Umeå, Sweden, were prospectively registered. The cataract surgery was performed at the University Clinic as there were no other public or private cataract surgery clinics in the area at baseline. The frequency of cataract surgery was 5.2 per 1000 population for the study period.
A total of 810 cataract surgery patients were included; 116 of them were between 30 and 64 years of age at the time of surgery. Three of the patients had surgery on both eyes during the time period studied. In these cases, the first eye having surgery is referred to as the “operated eye.” Details regarding the cohort, dropouts, inclusion and exclusion criteria, and questionnaire have been published earlier. We selected the patients younger than 65 years at the time of surgery as this is the normal age for retirement in Sweden.
Preoperative and Postoperative Examinations
A few weeks before surgery, and 4 to 8 weeks postoperatively, all patients were examined with dilation. BCVA was measured in each eye on a Monoyer-Granström letter chart. We present data from the “operated eye” and the “better-seeing eye.” We use these terms since the operated eye is not always the better-seeing eye. The presence of any ocular comorbidity or past surgery was noted.
The Questionnaire
A few days before surgery, the questionnaire was mailed to all patients and brought to the clinic at the time of the operation. A couple of months postoperatively, the patients were again asked to answer the same questionnaire. The mean time lapse from date of surgery to return of the second questionnaire was 3.7 months ± 1.4 months (SD). The questionnaire used was a Swedish translation of the VF-14 (visual function) questionnaire, a well-validated instrument to assess visual function in cataract patients. It was developed in the United States and has been found to be appropriate for use in cataract patients in Europe as well. This questionnaire assesses 14 vision-dependent activities such as reading a newspaper, filling out forms, driving, and recognizing people. The VF-14 score was calculated as described by Steinberg and associates, with a range from 0 (unable to do all applicable activities) to 100 (able to perform all applicable vision-dependent activities without difficulty).
Surgical Procedure
Four experienced surgeons were involved. The type of surgery performed was a sutureless, 3.2-mm, temporal-incision phacoemulsification. No polishing of the posterior or anterior capsule was done. The vast majority (806 of 801 patients; 99.5%) received a posterior chamber intraocular lens, of which 94% were an Alcon MA60BM Acrysof (Alcon Laboratories, Inc., Fort Worth, Texas, USA). The complication rates of posterior capsule and/or zonular rupture and vitreous loss were, in all 810 cases, 5.7% and 2.7%, respectively.
Data Collected 10 Years After Surgery
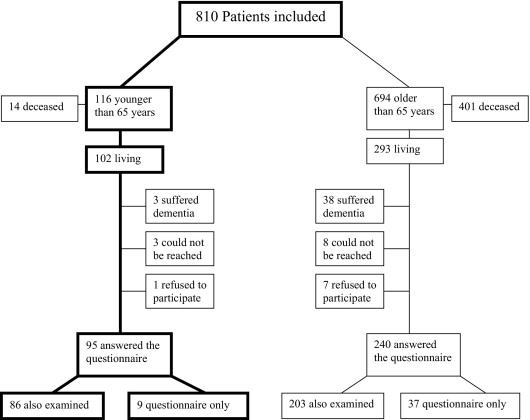
Ten years after surgery, all survivors were asked to participate with the questionnaire. Fourteen of the 116 patients less than 65 years at surgery (12%) were deceased, in comparison to 401 of the 694 patients 65 years or older (58%).
The patients received the same eye examination as performed 10 years earlier, with the exception that VA was measured with the early treatment diabetic retinopathy study (ETDRS) chart. Included in the examination was a subjective assessment of any present PCO. Low-contrast VA 10% and 2.5% were also tested. The flow chart of the patient cohort is presented in Figure 1 .
Statistical Methods
When the Monoyer-Granström letter chart was used, the VA values were converted into a log scale using the method outlined by Holladay and Prager. This was done to facilitate calculations of VA change (VA change = logarithm of the minimal angle of resolution [logMAR] acuity before surgery – logMAR acuity after surgery; a negative value denotes worse VA after surgery).
We defined a decline in VA as an increase in logMAR of 0.1 or more, compared with the VA recorded after surgery for each eye. Details regarding the calculation of VA when using the ETDRS chart have been described earlier.
Monocular low-contrast VA was tested using Sloan letter logarithmic translucent contrast charts (10% and 2.5%) (Precision Vision, La Salle, Illinois, USA) at a distance of 4 m. Participants who failed to read the largest letters at 4 m were tested at 1 m.
Nonparametric Mann-Whitney U tests were used to analyze differences in VF scores and VA data between the age groups, as the distribution of data was skewed. Independent-samples t test was used to compare the axial length between the age groups. The change in VA and VF-14 total score from postoperatively to 10 years after surgery was calculated by paired Wilcoxon signed rank test. Changes in trend were analyzed by χ 2 tests for trend. The 2-by-2 tables were calculated with χ 2 tests.
A life-table calculation was made to estimate the 10-year cumulative incidence of Nd:YAG laser posterior capsulotomy. Cox proportional hazard model was used to determine the differences in Nd:YAG treatment frequency between the patients less than 65 years of age and those 65 years or older at surgery.
All tests were 2-sided, and P values <.05 were considered statistically significant. Statistical analyses were performed using SPSS ver.16.0 (Statistical Package for the Social Sciences for MS Windows, SPSS Inc, Chicago, Illinois, USA).
Results
Demographics
Details of the demographic and clinical patient data are shown in Table 1 . A significantly higher proportion of the patients less than 65 years of age at surgery had received a Nd:YAG posterior capsulotomy 10 years after surgery, compared with the patients 65 years or older ( P = .0028).
| All Patients | Less Than 65 at Surgery | 65 Years or Older at Surgery | P value a | |
|---|---|---|---|---|
| No. of patients with 10-year VF-14 data | 335 | 95 | 240 | |
| No. of patients with 10-year VA and VF-14 data | 286 | 86 | 200 | |
| Mean age 10 years after surgery, years (SD) | 64.6 ± 8.3 | 84.0 ± 5.0 | ||
| Males, no. (%) | 107 (32) | 41 (43) | 66 (28) | .08 b |
| No. of patients operated on both eyes after 10 years (%) | 274/335 (82) | 73/95 (77) | 201/240 (84) | .19 b |
| Mean axial length, (mm) (SD) | 24.1 ± 1.960 | 23.54 ± 1.394 | .003 c | |
| Nd:YAG laser treatment, operated eye, n/total (%) | 84/335 (28) | 35/95 (36.8) | 49/240 (20.4) | .0028 b |
a Values in boldface are statistically significant ( P < .05).
Visual Functional Longitudinal Changes
In Table 2 , the VF-14 scores before surgery, 4 months after surgery, and 10 years later are presented. There were no significant differences in the VF-14 scores between the younger and the older patients before surgery and 4 months postoperatively. At the 10-year follow-up, the patients less than 65 years at surgery had a significantly better VF-14 score ( P = .000).
| Group | Number of Patients (Mean Age at Surgery, Years) | Before Surgery | 4 Months After Surgery | 10 Years Later | P value a |
|---|---|---|---|---|---|
| Less than 65 | 95 (54.6) | ||||
| VF-14 score | |||||
| Mean ± SD | 75.2 ± 19.8 | 94.6 ± 10.6 | 93.6 ± 13.3 | ||
| Median | 79.2 | 100 | 98.2 | .422 | |
| Q1:Q3 | 63.9:90.9 | 92.5:100 | 93.8:100 | ||
| 65 years or older | 240 (74) | ||||
| VF-14 score | |||||
| Mean ± SD | 74.4 ± 22.2 | 93.0 ± 14.2 | 82.6 ± 26.1 | ||
| Median | 80.6 | 100 | 95.0 | .000 b | |
| Q1:Q3 | 61.4:92.3 | 92.5:100 | 78.6:100 | ||
| P Value | 0.924 | 0.972 | 0.000 c |
a Values in boldface are statistically significant ( P < .05).
b Change in VF-14 postoperatively vs 10 years after surgery (paired Wilcoxon signed rank test).
c Differences in VF-14 total score between the young and the old (Mann-Whitney U test).
Table 3 shows the distribution of changes in VF-14 total scores 4 months postoperatively compared with 10 years after surgery. There was a significantly larger proportion of patients with a greater decline of VF-14 score 10 years after surgery in patients 65 years or older at surgery ( P = .00004).
| Change in VF-14 Score | Less Than 65, No./Total (%) | 65 Years or Older, No./Total (%) |
|---|---|---|
| VF-14 unchanged or better | 59/95 (62%) | 105/240 (44%) |
| Decline in VF-14 score <10 points | 27/95 (28%) | 66/240 (28%) |
| Decline in VF-14 score 10-20 points | 6/95 (6%) | 20/240 (8%) |
| Decline in VF-14 score >20 points | 3/95 (3%) | 48/240 (20%) |
| P value | .00004 a |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


