Tectonic Corneal Transplantation
Beatrice E. Frueh
Tectonic (from Latin tectum, “roof”) grafts, also called patch grafts, are either lamellar or perforating, and cover corneal stromal defects, restoring the structure of the cornea or sclera.
INDICATIONS
Indications for tectonic keratoplasty include infectious and sterile stromal defects, with perforation or impending perforation. Patch grafts can be used temporarily (for a later penetrating keratoplasty with better donor material and when there is less inflammation) or permanently to repair peripheral or central descemetoceles and perforations (1,2). Local and systemic autoimmune diseases, like rheumatoid arthritis, Sjögren’s syndrome, Wegener’s granulomatosis, polyarteritis nodosa, Stevens-Johnson syndrome, systemic sclerosis, and Mooren’s ulcer can cause stromal ulceration (3, 4, 5, 6). In developed countries, herpes simplex virus and varicella zoster virus are the most frequent causes of infectious stromal melting, whereas in developing countries fungal and bacterial keratitis are more frequent. Thinning disorders, like Terrien’s marginal degeneration, pellucid marginal degeneration, and keratoglobus, can also be improved with tectonic grafts. Corneal ulceration can also be caused by secondary changes resulting from other diseases, such as conjunctival cicatrization, lid abnormalities, keratoconjunctivitis sicca, and trichiasis. The correct diagnosis of the etiology of the melting process is extremely important to treat underlying disease before and after the corneal surgery.
SURGICAL TECHNIQUE AND POSTOPERATIVE CARE
Depending on the clinical situation, a patch graft can be performed with cornea, sclera, tissue adhesive, amniotic membrane, or polytetrafluoroethylene (Gore-Tex). In general, cyanoacrylate tissue adhesive can seal only small perforations and is rather unsuitable for use in the visual axis (less transparent than a patch graft with corneal tissue). In case of larger or central perforations, penetrating keratoplasty may be a better option.
In cases of Mooren’s ulcer, conjunctival excision should be performed before the melting process becomes too severe, or at the time of tectonic grafting (7). Application of tissue adhesive can stop the melting process (8) or, in case of perforation, reform the anterior chamber and also allow one to wait for suitable donor tissue. Before surgery, a bandage soft contact lens can be fitted to reform the anterior chamber.
Surgery is preferably done with general anesthesia after mannitol infusion for reduction of intraocular pressure. After placing a speculum, a paracentesis is performed and a viscoelastic is injected into the anterior chamber. Usually the paracentesis can be done even if the anterior chamber is flat and the eye is soft. If this is not possible, viscoelastic agents can be injected directly through the perforation site. All necrotic tissue should be removed from the area of the stromal melt to assess the real size of the ulceration and decide on the size and shape of the trephination. The goal of the dissection should be to remove all affected corneal tissue but to preserve as much healthy host tissue as possible. When possible, the visual axis should be spared from wound margins or sutures. Peripheral ulcers may require conjunctival peritomy and scleral dissection. If the ulceration or thinned area is peripheral and not too irregular in shape, a small, standard hand-held trephine can be used (9). A partial-thickness trephination of the recipient bed is performed: In most cases, the trephination will be superficial because of the hypotony. Deepening of the trephination with a sharp blade or diamond knife and lamellar dissection are then performed. A donor button of the same size or slightly oversized, full or partial thickness, is then sutured in place using interrupted 10-0 nylon sutures. Running sutures are contraindicated because of the greater risk for suture loosening
in inflamed eyes. In cases of irregular or crescentic ulcerations, the patch graft should match the ulceration shape and therefore cannot be achieved with a simple round trephination. In such instances, one side of the trephination can be achieved with an hand-held trephine and the rest must be cut freehand. It is advisable to use a caliper to measure exactly the size of the lesion before cutting the donor tissue. A template exactly matching the area to be removed can be cut from a surgical drape and can be helpful in cutting the donor tissue. In perforated corneas or when the iris adheres firmly to the cornea, an iridectomy is performed.
in inflamed eyes. In cases of irregular or crescentic ulcerations, the patch graft should match the ulceration shape and therefore cannot be achieved with a simple round trephination. In such instances, one side of the trephination can be achieved with an hand-held trephine and the rest must be cut freehand. It is advisable to use a caliper to measure exactly the size of the lesion before cutting the donor tissue. A template exactly matching the area to be removed can be cut from a surgical drape and can be helpful in cutting the donor tissue. In perforated corneas or when the iris adheres firmly to the cornea, an iridectomy is performed.
At the end of surgery, the viscoelastic agent is removed, and antibiotic (gentamicin 40 mg/mL) and steroid are injected subconjunctivally. We refrain from injecting steroids in cases of fungal or severe bacterial infections. An ointment (tobramycin and dexamethasone) is applied and systemic antibiotics are administered. The postoperative topical regimen depends on the etiology of the melt: For sterile ulcerations, prednisolone acetate 1% is given four times daily. For infectious ulcers, the further use of fortified antibiotics (according to sensitivity tests) or antifungal agents may be needed, and the use of corticosteroids is contraindicated, despite a higher risk for rejections. The eradication of the infection in the perioperative period is more important than a possible rejection of the patch graft. In viral ulcers, antivirals locally and systemically are indicated. The treatment of underlying autoimmune diseases, with appropriate systemic immunosuppression, is of eminent importance (10,11).
Secondary glaucoma, because of synechia formation, intraocular inflammation, or steroid dependence, is not uncommon. I prefer not to prescribe prostaglandin agonists or prostamides as first-line therapy because of their potential for causing increased inflammation.
A not uncommon problem of patch grafts is nonhealing epithelial defects, leading to stromal melt and loosening of sutures. Aggressive lubrication, punctum plugs, serum drops, and bandage contact lens or tarsorrhaphy should be used. All loose sutures must be removed and replaced. If the epithelial defect is persistent, amniotic membrane transplantation or conjunctival flap should be considered before the melting process resumes. After the first 6 to 8 postoperative weeks, long-term care usually does not differ from that in standard keratoplasty.
RESULTS
Results vary depending on the initial diagnosis, and a comparison of technique outcomes is difficult owing to the relative paucity of patch grafts compared with standard lamellar or penetrating keratoplasties, the variety of shapes and sizes of the melting processes and their medical management, and the severity of systemic disease.
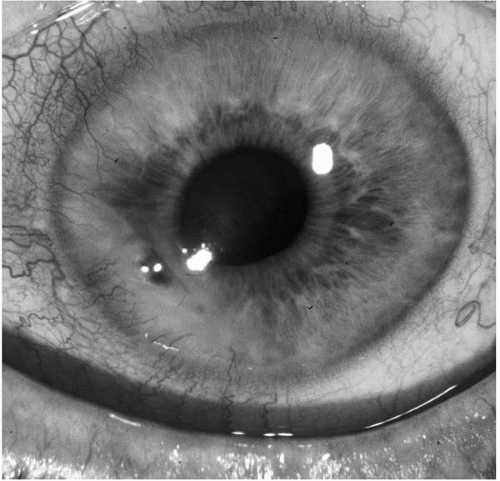 FIGURE 53-1. Peripheral ulcerative sterile keratitis in an 84-year-old patient without an underlying immunologic disorder.(see color image) |
Visual results of tectonic keratoplasties are in general inferior to elective penetrating keratoplasties in nonmelting situations (12,13).
Mooren’s ulcer, as a special entity, appears to do favorably after lamellar keratectomy or lamellar keratoplasty. The possible mechanism is the removal of a corneal antigen stimulus to a self-perpetuating autoimmune process (14).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


