CHAPTER 54 Surgical rehabilitation of Graves’ orbitopathy
Introduction
Graves’ orbitopathy (GO) is one of the phenotypic appearances of Graves’ disease, a multisystem disorder which usually leads to hyperthyroidism and goiter, less frequently to GO, and rarely to pretibial myxedema and acropachy. GO is the most frequent and important extrathyroidal expression of Graves’ disease. It may also be found, although less frequently, in patients with no present or past history of hyperthyroidism (so-called euthyroid or ophthalmic Graves’ disease), or in patients who are hypothyroid due to chronic autoimmune (Hashimoto’s) thyroiditis1,2. In most affected individuals GO is mild and self-limiting, and only in 3–5% of cases is it severe and potentially sight threatening1,3.
The exact pathogenesis of GO is unknown4–7. It is, however, worth highlighting the clear-cut link between the orbit and the thyroid, because this has important clinical and therapeutic implications8. In addition to endogenous (non-preventable) determinants, such as genetics, age- and gender-related factors9, GO occurrence and progression are influenced by environmental (preventable) factors, such as cigarette smoking, thyroid dysfunction, and different treatments for hyperthyroidism3,10. This implies that control or correction of these risk factors is an integral part of GO management.
The natural history of GO is of gradual increase in severity followed by a plateau phase then gradual improvement11. These are the active phases. The inactive phase follows with no change in severity. GO is thus self-limiting, although it often does not return to baseline. Treatment is aimed at accelerating recovery, preventing serious sequelae, and eventually functional and cosmetic rehabilitation.
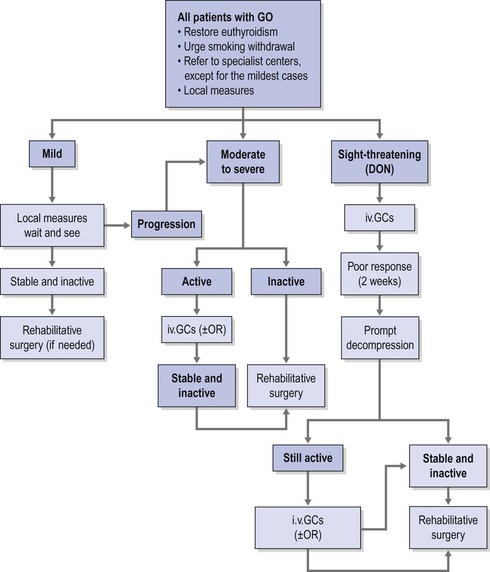
Therapeutic options consist of medical therapy, radiotherapy, surgery, or frequently a combination of these. Consensus as to indications and timing of these options has been reached by the EUGOGO consortium (Fig. 54.1)12,13.
Timing of surgery
The first rehabilitative step mainly consists of orbital bony decompression. It causes reduction in exophthalmos as well as reduction in upper and lower eyelid displacement14. It may positively influence extraocular muscle restrictions, but displacement and scarring of the soft orbital tissues caused by decompression surgery may also cause strabismus. Possible squint surgery should therefore follow orbital decompressions, but considering that vertical tropias may influence eyelid position, squint surgery should precede possible eyelid corrections. Finally, when necessary, the finishing touch can be given by eyebrow lift, forehead plasty, and blepharoplasty.
In short, surgical rehabilitation needs to respect the given order since the preceding step may influence the necessity and the extent of the step that follows. When all the steps are necessary, the entire rehabilitation may require between 1.5 and 2 years. In particular cases, exceptions are possible and the rehabilitation can be favorably speeded up by carrying out more than one procedure at the same time15. The traditional management algorithm has not been respected in only a few series16–20, and it has met with vigorous criticism21.
Orbital decompression
This positive feedback circle leads to an increase in the intraorbital pressure, which is first responsible for the progression of GO and later for its typical signs and symptoms5. Any surgical procedure aimed at decreasing the raised intraorbital pressure and its effects by means of enlargement of the bony orbit and/or removal of the orbital fat is defined as orbital decompression.
Orbital decompression is currently indicated for the treatment of optic neuropathy refractory to medical therapy, exposure keratopathy unresponsive to local measures and/or minor eyelid surgeries, disfiguring exophthalmos and symptoms. Eyeball subluxation (which may be a possible cause of acute optic neuropathy and exposure keratopathy) postural visual obscuration in patients with congestive inactive GO and recently onset choroidal folds due to eyeball indentation by enlarged extraocular muscles represent other functional indications for decompression surgery22.
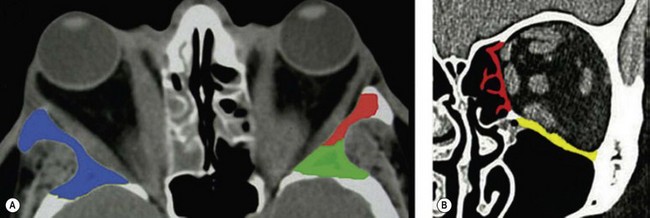
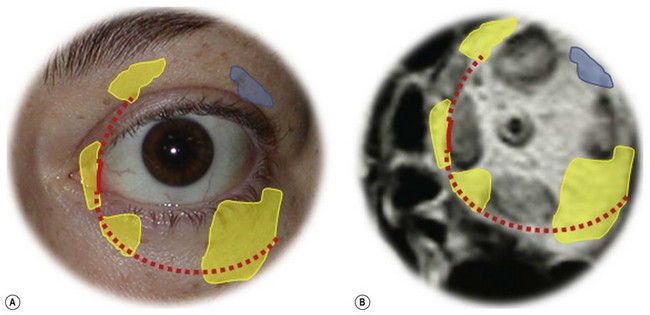
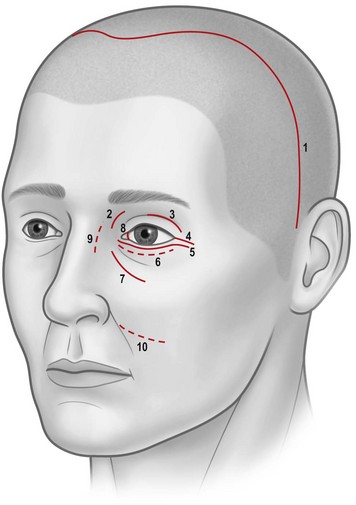
Osteotomies can involve the medial, and lateral orbital walls and the orbital floor (Fig. 54.2); lipectomies can be performed at the level of all the orbital quadrants (Fig. 54.3). Decompression surgery can be performed through several different surgical incisions (Fig. 54.4) preferably under general anesthesia.
The inferior fornix incision is an extremely popular approach to orbital decompression. It can be extended medially into a transcaruncular incision and can be associated with an incision at the lateral canthus that permits the lower lid to swing outwards, thus easing the exposure of the lateral wall. This latter association, first described by McCord in 1981, is known as ‘swinging eyelid’23. This combination of periorbital incision permits an easy approach to the orbital floor, medial, and lateral walls and lipectomies from the inferior orbital quadrants.
The coronal approach is a more invasive procedure which, however, offers the widest access to the lateral orbital wall24, and it may have distinctive advantages in a number of situations including the presence of remarkable periorbital swelling or conjunctival chemosis, the necessity of minimizing the number of periorbital incisions, or the necessity of extensive manipulation of the lateral wall (including its rim)25,26. Through a coronal incision, brow lift, and correction of frontal/glabellar rhytids, which are often necessary in patients with GO, can be performed simultaneously with orbital decompression, thus favorably speeding up the timing of rehabilitative surgery25,27.
Orbital decompression by transinferior fornix/transcaruncular/swinging eyelid: surgical technique


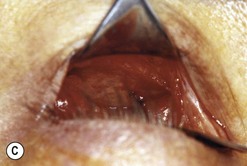

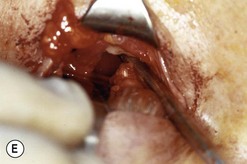

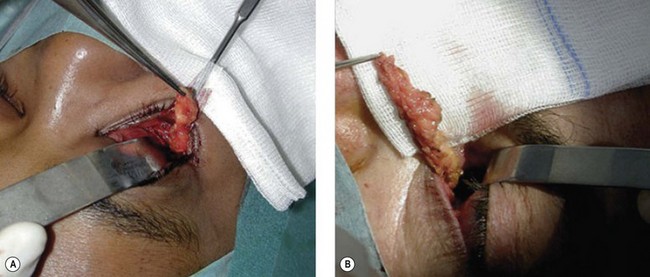
Fig. 54.5 Transinferior fornix decompression. Phases of surgery (A–F); for explanations see the main text.
Orbital decompression by upper skin crease approach: surgical technique
 of the upper skin crease if the upper medial fat compartment is not to be addressed. On occasion it can be joined to the lateral canthotomy of a possible swinging eyelid approach to implement the exposure of the surgical site (Fig. 54.7A).
of the upper skin crease if the upper medial fat compartment is not to be addressed. On occasion it can be joined to the lateral canthotomy of a possible swinging eyelid approach to implement the exposure of the surgical site (Fig. 54.7A).