Purpose
To design a surgical procedure for correcting globe dislocation in strabismus in high myopia (highly myopic strabismus).
Design
Prospective, interventional case series.
Methods
We examined 36 eyes of 21 patients with highly myopic strabismus and 27 eyes of 27 healthy volunteers as controls at Osaka City General Hospital between 2000 and 2006. Anatomic relationships between the muscle cone and globe were analyzed using magnetic resonance imaging. Ranges of globe movement and angles of ocular deviation were measured quantitatively as angles of maximum abduction and sursumduction and angles of ocular deviation, respectively, using the Goldmann perimeter and alternate prism cover tests. A surgical procedure involving muscle union of the superior rectus and lateral rectus muscles was performed in 23 eyes of 14 patients to restore the dislocated globe back to the muscle cone.
Results
After surgery, the angle of dislocation of the globe, defined as the angle formed by a line connecting the area centroid of the superior rectus muscle and the globe and a line connecting area centroid of the lateral rectus muscle and globe against the supertemporal wall of the orbit, was significantly decreased ( P < .001), and angles of maximum abduction and sursumduction and the angle of ocular deviation improved significantly ( P < .001).
Conclusions
This surgical procedure to restore the dislocated globe back into the muscle cone by uniting muscle bellies of the superior rectus and lateral rectus muscles is effective for highly myopic strabismus.
Strabismus in high myopia is an acquired strabismus in eyes with axial high myopia. This strabismus is characterized by restriction in both abduction and sursumduction and results in esotropia and hypotropia. At the most advanced stage, the affected eye is so tightly fixed in an esotropic and hypotropic position that movement in any other direction is impossible. This extreme condition has been called convergent strabismus fixus or myopic strabismus fixus . However, strabismus associated with high myopia does not always take the form of strabismus fixus. Severity varies from small-angle esotropia with mild restriction in abduction, in which the eye can be moved past the midline, to strabismus fixus. The strabismus is not always esotropic, with even exotropia and hypotropia reported. What these conditions have in common is axial high myopia and restrictive ocular motility. We propose the term highly myopic strabismus for this disease and use this term throughout this article.
Several reports have proposed a variety of causes for highly myopic strabismus. We noted 3 papers reporting inferior displacement of the lateral rectus (LR) muscle using different methods. Both Ohta and associates and Krzizok and Schroeder speculated that downward displacement of the LR muscle may disturb abduction. However, although downward shift of the LR muscle may weaken the abducting force, this itself does not explain how both abduction and sursumduction are restricted simultaneously in this disease, particularly in strabismus fixus. Furthermore, clear explanations on how the LR muscle becomes displaced have not been provided. Traditional surgical procedures include recession or tenotomy of the medial rectus muscle, recession of the nasal conjunctiva, ordinary recession and resection procedures, and the traction suture. Although these procedures are effective in some cases, esotropia often recurs within a few months. Having noted the downward displacement of the LR muscle in this disease, some authors have reported superior transposition of the insertions of the LR muscle, the medial rectus muscle, or both or superior fixation of the LR muscle belly. With regard to displacement of the superior rectus (SR) and LR muscles, Yamada and associates reported hemitransposition of SR and LR muscles. However, these procedures were effective only in limited cases.
We previously showed supertemporal dislocation of the posterior portion of the elongated globe out from the muscle cone. Aoki and associates reported similar findings. Based on these observations, we performed a surgical procedure uniting the muscle bellies of the SR and LR muscles in patients with highly myopic strabismus. This procedure was aimed at restoring the dislocated globe back into the muscle cone. We then evaluated the surgical outcomes and investigated anatomic changes from before and after surgery.
Methods
This research was designed as an interventional case series. Thirty-six eyes of 21 patients with highly myopic strabismus were examined at Osaka City General Hospital between 2000 and 2006. Mean (± standard deviation) patient age was 63.8 ± 8.3 years. Criteria for inclusion in this study were acquired strabismus and axial high myopia. Patients who had undergone previous strabismus surgery were excluded, and this history was confirmed by interview with the patient. High myopia was defined as an axial length of 27.0 mm or more. The 36 eyes all were elongated axially, and mean axial length of the globe was 31.9 ± 2.1 mm. Refractive values are not shown, because 13 eyes already had undergone cataract surgery. Three patients had bilateral strabismus fixus, and 2 had unilateral strabismus fixus. The 28 eyes of the remaining 16 patients showed various extents of restricted abduction. Among the 36 eyes of the 21 patients, we operated on 23 eyes of 14 patients who agreed to undergo our new surgical treatment. As controls, 27 eyes of 27 healthy volunteers (mean age, 43.4 ± 16.7 years) who showed no restriction in ocular motility or strabismus were examined. The control group was classified into a non–high-myopia group and a high myopia group. In the control group, mean axial length of the globe was 26.2 ± 2.8 mm; 18 eyes had non–high myopia (mean axial length, 24.6 ± 1.0 mm), and 9 eyes had high myopia (mean axial length, 29.5 ± 2.1 mm). Axial length of the eye was measured by AL-2000 echography (Tomey, Tokyo, Japan).
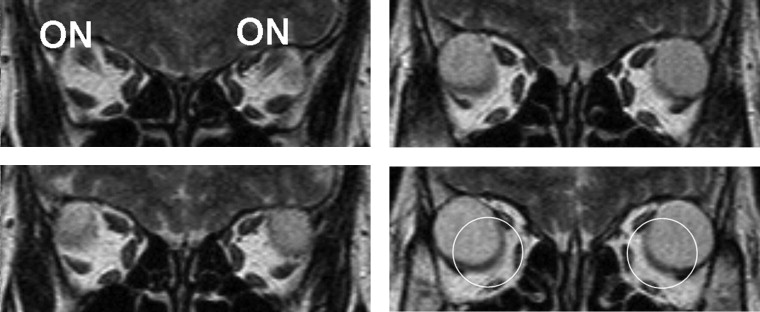
All patients and healthy volunteers were examined with a 1.0T Magnetom Impact or Magnetom Harmony system (Siemens, Erlangen, Germany). Axial and coronal T2-weighted spin-echo imaging was performed with a slice thickness of 3 mm. All subjects were instructed to remain still in the infraducted eye position. We had to avoid the influence of gaze position on anatomic relationships between the globe and extraocular muscles. We therefore needed to control gaze at the same position in all subjects. Because 10 patients could not maintain the eyes in the primary position, particularly those with strabismus fixus, we used infraduction to analyze the results of magnetic resonance imaging (MRI) for every subject under the same conditions. All MRI data were transferred directly onto a personal computer as 256 × 256-pixel bitmap images for further analysis.
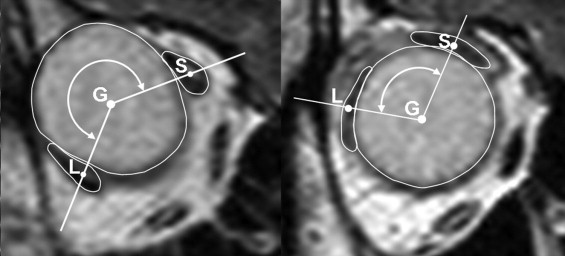
To analyze the orbital structures, we used coronal MRI at the third slice (9 mm) anterior to the optic nerve–globe junction in each orbit to avoid the influence of globe shape, such as staphyloma. For example, the top left slice in Figure 1 was nearest to the junction of the globe and optic nerve. The bottom right image in Figure 1 therefore was chosen for analysis. To investigate quantitatively the anatomic relationships between the globe and the SR and LR muscles, we calculated the coordinates of the centers of the globe, SR muscle, and LR muscle using Scion Image software (Scion Corporation, Frederick, Maryland, USA). Before calculation, the margins of the globe and LR and SR muscles were traced on MRI images with a pen tablet (Wacom, Tokyo, Japan), and the area centroid of each object was determined using the XY center tool of the Scion Image software. Points were referred to as G, S, and L for the globe, SR muscle, and LR muscle, respectively ( Figure 2 ). Straight lines were drawn from G to S and L, respectively. The angle between the line GS and the line GL, that is, angle LGS (including the supertemporal quadrant of the orbit), was calculated and referred to as the angle of dislocation of the globe . When this angle exceeded 180 degrees, more than half of the cross-section of the globe was located outside the muscle cone through an opening between the SR and LR muscles.
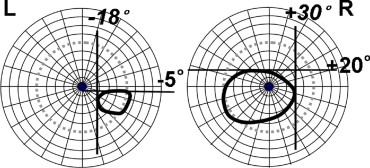
The range of full duction movements was measured using a Goldmann perimeter. Patients were instructed to track a V4 object within a Goldmann perimeter with the untested eye occluded, and gaze limits of all directions were recorded on a recording sheet to obtain a unilateral fixation field. Maximum angles of abduction and sursumduction were obtained in each eye, as illustrated in Figure 3 . In 5 patients who barely recognized the V4 object because of low vision, tracking the moving object continuously was difficult. In these patients, the fixation field was determined by observing the corneal light reflex through the observing telescope. First, these 5 patients were instructed to fix on a full duction position, and then position was measured by moving the V4 object so that the corneal light reflex was observed at the exact center of the cornea.
The angle of ocular deviation was measured, in principle, with the alternate prism cover test at 0.33 m. Fourteen patients underwent measurement using this method. In 4 patients for whom neither eye could abduct past the midline, the Krimsky test was used with prisms placed in front of both eyes. All eyes in which visual acuity was too poor to fixate on a visual target displayed strabismus fixus. In 3 patients with strabismus fixus in both eyes, ocular deviation was calculated by adding the maximum angles of abduction of both eyes.
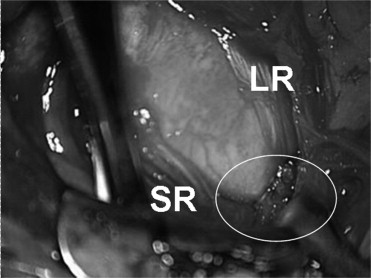
Surgery involved 2 procedures. The first was aimed at creating a junction between the muscle bellies of the SR and LR muscles (muscle union). This junction was made approximately 15 mm behind the insertions using a polyester suture ( Figure 4 ). The other surgical procedure involved recession of the medial rectus muscle. Recession was performed when recovery of the movable range of the eyeball had been insufficient after uniting the SR and LR muscles. To evaluate the surgical effects, we compared the following variables before and after surgery: (1) angle of dislocation of the globe; (2) maximum angles of abduction and sursumduction; (3) angle of ocular deviation; and (4) preoperative and postoperative forced duction tests.

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


