Surgical Management of Locally Invasive Thyroid Cancer
Ashok R. Shaha
INTRODUCTION
The incidence of thyroid cancer is increasing rapidly worldwide. Approximately 56,000 new patients with thyroid cancer will be seen in the United States in the year 2012. Although the major rise in incidence of thyroid cancer is seen in patients with small cancers, below 2 cm, there also appears to be a slight rise in the incidence of advanced thyroid cancer. There is an increased detection of incidental thyroid nodules seen on imaging studies done for other purposes such as ultrasound (US), carotid Doppler, computed tomography (CT), magnetic resonance imaging (MRI), and positron emission tomography (PET) scans, which may account for this apparent increase in thyroid cancer.
Despite increased detection rates, the mortality from thyroid cancer has remained essentially unchanged over the past two decades. Approximately 1,400 patients die of thyroid cancer every year in the United States, a majority of whom have aggressive well-differentiated, anaplastic, or medullary thyroid cancer. Although death from well-differentiated thyroid cancer is quite rare, these cancers may invade the surrounding structures in the neck, such as trachea, recurrent laryngeal nerve (RLN), esophagus, and larynx. Patients with locally invasive thyroid cancer usually have a long history of the presence of thyroid cancer. However, certain forms of biologically aggressive thyroid cancer such as poorly differentiated tall cell variant or insular thyroid cancer may grow rapidly and be locally invasive.
Thyroid cancer is characterized by slow growth. The prognostic features in thyroid cancer are well recognized through reports from the Mayo Clinic, Lahey Clinic, Memorial Sloan-Kettering Cancer Center which include age, gender, grade of the cancer, size of the cancer, extrathyroidal extension, and distant metastases. Thyroid cancer is generally considered to be more aggressive in patients above the age of 45. In patients above the age of 60 to 65, thyroid cancer is much more aggressive and the incidence of the poorly differentiated form is much higher.
The prognostic factors are crucial in the evaluation, management, and prognosis of patients with thyroid cancer. Based on the prognostic factors, the risk group stratifications such as low-and high-risk groups are well described by Blake Cady from the Lahey Clinic and by Ian Hay from the Mayo Clinic. The low-risk thyroid cancer group includes younger patients with smaller cancers, while high-risk groups include patients above the age of 45 with more aggressive and advanced form of thyroid cancer.
The data from Memorial Sloan-Kettering Cancer Center were further analyzed leading to the stratification of low-, intermediate-, and high-risk groups. Our patients were divided into low risk (younger patients with small cancers) or high risk (older patients with larger tumors or a more aggressive form of thyroid cancer). An intermediate-risk group was described, which includes younger patients with more aggressive forms of thyroid cancer or older patients with smaller (non aggressive) cancers. There clearly is a survival difference in these three risk categories, and the treatment decisions should be individualized based on risk group analysis. Generally, patients in the low-risk group of thyroid cancer require appropriate and satisfactory surgical excision only, while the high-risk group requires aggressive surgery and additional treatment including radioactive iodine ablation and external beam radiation therapy in a selected group of patients. While the treatment of patients in
the intermediate-risk group should be individualized based on the aggressiveness of the primary cancer, this would generally include younger patients having more aggressive forms of thyroid cancer requiring adjuvant treatment such as radioactive iodine ablation, while older patients with small cancers would require surgical excision only.
the intermediate-risk group should be individualized based on the aggressiveness of the primary cancer, this would generally include younger patients having more aggressive forms of thyroid cancer requiring adjuvant treatment such as radioactive iodine ablation, while older patients with small cancers would require surgical excision only.
HISTORY
The history and physical examination are very important in the evaluation of the patient with locally invasive thyroid cancer. The presence and duration of symptoms such as dysphagia, weight loss, shortness of breath, and hoarseness are crucial in appreciating the locally aggressive nature of the disease. Subtle symptoms such as sore throat and mild dysphagia will require further detailed investigation. Occasionally, the patient may give a history of a thyroid nodule being present for a long time with previous benign or indeterminate needle biopsies. The presence of a mass in the neck arouses suspicion of metastasis to the cervical lymph nodes. These patients will require further evaluation to make the diagnosis and determine the extent of the cancer.
PHYSICAL EXAMINATION
A detailed physical examination of the entire neck remains a critically important aspect in the evaluation of the patient suspected of having locally invasive thyroid cancer. The central compartment must be examined to determine the size and configuration of a mass when present. The degree of fixation of the mass to the skin and/or the trachea must be noted. The entire neck should be palpated to determine the presence of metastasis to the lymph nodes. Mirror or fiberoptic laryngoscopy must be carried out to determine whether mobility of the vocal cord/s is impaired. The finding of a mass fixed to the central compartment in the presence of a paralyzed vocal cord suggests locally invasive thyroid cancer.
INDICATIONS
Locally aggressive thyroid cancer invading the surrounding structures in the central compartment of the neck
Recurrent thyroid cancer with local invasion
Patients presenting with vocal cord paralysis or a fixed mass in the central compartment
Cancer adherent to or invading the trachea, larynx, or esophagus
Bulky primary cancer with invasion of the strap muscles
CONTRANDICATIONS
Massive cancer involving the central compartment and encasing the carotid artery/s
Extensive cancer involving the mediastinum and occasionally the sternum
Massive cancer causing bilateral vocal cord paralysis and airway obstruction
Cancer invading the prevertebral fascia and paravertebral musculature
Massive distant metastases with major loss of pulmonary reserve
Massive tracheal invasion in close proximity to the carina
PREOPERATIVE PLANNING
Thyroid function tests will confirm the patient to be euthyroid before the surgery. However, thyroglobulin may be of help as a baseline tumor marker. Calcitonin and carcinoembryonic antigen (CEA) are important tumor markers if medullary thyroid cancer is suspected.
Imaging Studies
US is a useful technique in the evaluation of the extent of the cancer, and features suggestive of malignancy such as irregular margin, microcalcification, and hypervascularity are extremely valuable.
Cross-sectional imaging in suspected locally aggressive thyroid cancer is a critical aspect in the evaluation of the extent of the cancer and its invasion into or adherence to the surrounding structures in the central compartment. CT scan with contrast is the best imaging study for the evaluation of the extent of the cancer. While the use of contrast will delay radioactive iodine ablation by 2 to 3 months, if the operating surgeon feels that the information obtained from CT with contrast is crucial in selecting the best surgical procedure for the invasive thyroid cancer, the CT should be performed with no hesitation.
MRI is generally not necessary; however, if the cancer is inseparable from the trachea, MRI is quite helpful to evaluate the relation of the cancer to the trachea. If there is any involvement of the tracheal wall or tracheal lumen, US should be performed for more detailed evaluation of the primary cancer and cervical lymph nodes.
Other imaging studies such as PET scan and bone scans are individualized. For consistency in poorly differentiated cancer, the PET scan may be of value to evaluate the distant organs such as mediastinum, lung, or liver. Routine chest radiography or CT scan may not be helpful in determining the presence of pulmonary metastasis, which is best evaluated in well-differentiated thyroid cancer with a radioactive iodine scan.
Pathology
If the patient has been biopsied elsewhere or has had previous surgery for cancer of the thyroid, the slides should be obtained and reviewed by a head and neck pathologist. If a tissue diagnosis has not been obtained, appropriate biopsies should be done to establish the correct diagnosis. Any suspicious lymph nodes in the neck may require preoperative fine needle aspiration biopsy with cytology or thyroglobulin wash from the aspirant.
SURGICAL TECHNIQUE
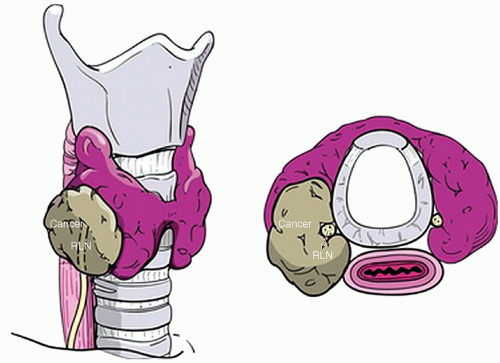
In long-standing or biologically aggressive cancer of the thyroid, the wall of the trachea may be directly invaded with extension of the cancer into the lumen. The recurrent laryngeal nerve (RLN) is directly related to the posterior capsule of the thyroid gland, and even though direct invasion of the RLN is rare, the nerve may be embedded in the cancer and it may be extremely difficult or impossible to separate from the cancer requiring sacrifice of the portion of nerve for tumor clearance (Fig. 18.1). Occasionally, cancer in the lymph nodes in the paratracheal area may directly invade the RLN leading to preoperative palsy and the need to resect a portion of the RLN.
The growth of the primary cancer or cancer in the lymph nodes in the tracheoesophageal sulcus may invade vital structures such as the RLN, trachea, or esophagus. The surgeon must be prepared to undertake appropriate surgical resection if these surrounding structures are involved by the primary cancer or metastatic lymph nodes. Involvement of the esophagus is quite rare, and most of the time, the cancer is adherent to the esophageal musculature leading to the need for resection of the esophageal muscles rather than the mucosa itself. However, if the cancer involves the esophageal mucosa, a much more radical resection is required and reconstruction may require a microvascular free flap or a gastric pull up. Cancer involving the region of the cricoid cartilage or cricopharyngeal muscles may be difficult to evaluate even intraoperatively on gross evaluation. The management of recurrent cancer involving this region of the cricothyroid area makes for extremely complex surgical decision making as laryngectomy may be necessary for surgical resection with cancer-free margins. Involvement of other vital structures such as the carotid artery, vagus, and phrenic nerves and sympathetic trunk is quite rare.
The majority of these patients will require a multidisciplinary approach with active involvement of specialists in endocrinology, nuclear medicine, and medical oncology with special expertise in the management of thyroid cancer with targeted therapies. The laryngologist and speech language pathologist play an important
role in the management of voice problems. The RLN may be directly in contact with cancer, and resection of the RLN or any tedious separation may jeopardize the function of the RLN either temporary or permanently. The superior laryngeal nerve (SLN) is rarely directly involved by the cancer, but surgical intervention may lead to iatrogenic trauma to the SLN, leading to a change in voice and inability to raise the voice, pitch, and tone. The parathyroid glands are adherent to the posterior portion of the thyroid capsule. In locally aggressive thyroid cancer, these glands may be inseparable from the cancer or may be involved in the thyroid capsule leading to unintentional loss of one or more parathyroid glands, resulting in temporary or permanent hypoparathyroidism. Consideration should be given to parathyroid autotransplantation.
role in the management of voice problems. The RLN may be directly in contact with cancer, and resection of the RLN or any tedious separation may jeopardize the function of the RLN either temporary or permanently. The superior laryngeal nerve (SLN) is rarely directly involved by the cancer, but surgical intervention may lead to iatrogenic trauma to the SLN, leading to a change in voice and inability to raise the voice, pitch, and tone. The parathyroid glands are adherent to the posterior portion of the thyroid capsule. In locally aggressive thyroid cancer, these glands may be inseparable from the cancer or may be involved in the thyroid capsule leading to unintentional loss of one or more parathyroid glands, resulting in temporary or permanent hypoparathyroidism. Consideration should be given to parathyroid autotransplantation.
Anesthesia Considerations
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree