CHAPTER 53 Surgical approaches to the orbit
Introduction
Historically, orbital surgery has been performed by general surgeons, ophthalmic surgeons and, in particular, neurosurgeons; indeed, Walter Dandy – the highly influential neurosurgeon – suggested that, ‘all orbital surgery should be performed through the transcranial route’ and that ‘such surgery results in less morbidity than the commonly-used orbital approach’1. During the second half of the 20th century there was a shift towards less traumatic techniques for orbitotomy, avoiding craniotomy when a disease was solely intraorbital – this leading to the development of incisions and approaches with much better esthetic results. Clearly, a neurosurgical approach remains imperative where a disease straddles the cranio-orbital junction (such as with lesions passing through the superior orbital fissure or optic canal), and a maxillofacial or head-and-neck surgeon is best experienced to deal with orbital diseases involving the paranasal sinuses or extending widely outside the orbit.
Practical and anatomical considerations
The risk of injury to orbital function varies significantly at different depths within the orbit, there being variations within each zone. The risk of collateral injury is low during surgery in the anterior one-third of the orbit, alongside the globe – the risk probably being greatest in the trochlear area and to the palpebral lobe of the lacrimal gland. The most feared risk whilst operating in the middle-third of the orbit is the (relatively rare) visual loss due to ischemia of the optic nerve or optic nerve head, but the ciliary ganglion is probably the most susceptible structure in this sector – a persistent mydriasis being a not uncommon inconvenience after removal of retrobulbar tumors. Due to crowding of highly important structures in the orbital apex, operating in the posterior third of the orbit carries a high risk of complication – many being serious or permanent2; complete visual loss is quite common with removal of ‘peanut’ tumors wedged in the apex, especially where the tumor lies below the optic nerve, alongside the ophthalmic artery. Complete ophthalmoplegia is common after operating near the superior orbital fissure, this often recovering dramatically at about 3 months after surgery, but sometimes leaving a selective neuropraxia.
Preoperative and postoperative counseling
Apart from difficult access or the encroachment of fat into the operative field, it is intraoperative hemorrhage that creates the greatest difficulty and risk during surgery within the orbital depths; heat generated by the use of bipolar diathermy increases inflammation, the latter probably being contributory to early postoperative visual loss due to vasospasm at the orbital apex2. It is, therefore, very important to take a thorough history for any medications that might affect hemostasis3 – this including over 40 brand-named versions of amino-salicylic acid (ASA) and also many foodstuff and ‘herbal’ remedies. All herbal remedies, garlic, ginger, ginseng and gingko should be avoided completely before surgery. If safe to do so, patients should be encouraged to avoid ASA for at least 3–4 weeks before orbital surgery, non-steroidal anti-inflammatory drugs for at least 2 weeks, and other anti-platelet medications for at least 10–12 days. Special arrangements will be required for patients requiring warfarin anticoagulation for metallic heart valves and for patients with recently implanted arterial stents4. Medical conditions, such as systemic hypertension or diabetes, should be well controlled in all patients listed for routine orbital surgery, and a preoperative assessment by the anesthetist is appropriate where hypotensive general anesthesia will be required for surgery.
The six principal orbitotomies
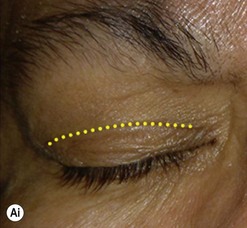
Anterior orbitotomy through the upper eyelid skin crease
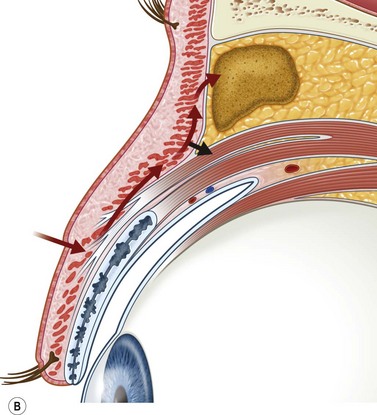
Incisions in the upper eyelid skin crease heal without visible scar and provide access to the upper two-thirds of the orbit, if necessary right back to the superior orbital fissure and orbital apex (Fig. 53.1A). Intraconal lesions lying above or medial to the optic nerve are reached by retracting the superior rectus/levator muscle complex either medially or laterally during the surgery.