Supranuclear ocular motor disorders can be caused by lesions in the brainstem (excluding the cranial nerve nuclei or fascicles), cerebellum, or cerebral hemispheres. Internuclear ocular motor disorders, by definition, are caused by damage to brainstem pathways that coordinate the movements of the two eyes. In this chapter, we discuss the features and causes of supranuclear and internuclear ocular motor disorders.
Ocular Motor Syndromes Caused by Lesions of the Medulla
The medulla contains a number of structures that are important in the control of eye movements: vestibular nuclei, perihypoglossal nuclei, medullary reticular formation, inferior olive, and restiform body (inferior cerebellar peduncle) (Fig. 17.1). The perihypoglossal nuclei consist of the nucleus prepositus hypoglossi (NPH), which lies in the floor of the fourth ventricle, the intercalatus nucleus, and the nucleus of Roller. These nuclei have rich connections with other ocular motor structures. The NPH and the adjacent medial vestibular nucleus (MVN) are of critical importance for holding horizontal positions of gaze (the neural integrator). These structures also participate in vertical gaze holding, although more rostral structures, especially the interstitial nucleus of Cajal (INC), provide the primary tonic contribution for vertical and torsional eye movements. Lesions of the paramedian structures of the medulla often produce nystagmus—commonly upbeat, but sometimes horizontal with a gaze-evoked component.
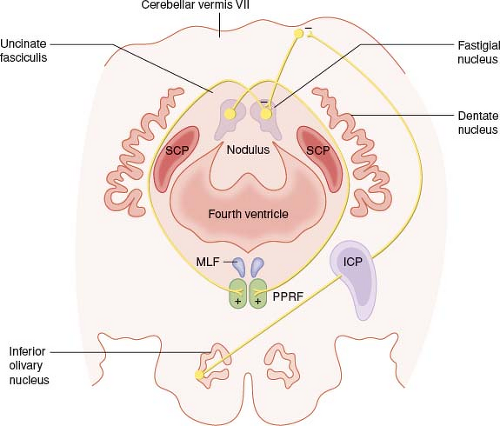
Lesions of the inferior olivary nucleus (ION) or its connections may produce the oculopalatal myoclonus syndrome (oculopalatal tremor). It is thought to occur due to an interruption in the Guillain–Mollaret triangle, which connects the red nucleus to
the ipsilateral ION (via central tegmental tract), to the contralateral dentate nucleus (via inferior cerebellar peduncle), back to the red nucleus (via superior cerebellar peduncle). This condition usually develops weeks to months after a brainstem or cerebellar infarction, although it may also occur with degenerative conditions or posttrauma (diffuse axonal injury). The delay in presentation occurs due to chronic deafferentation of the ION, which leads to a vacuolar degenerative hypertrophy and resulting disordered control of the ION (see Fig. 17.2). The term myoclonus is misleading, because the movements of affected muscles are to-and-fro and are approximately synchronized, typically at a rate of 2 to 4 cycles/sec.
the ipsilateral ION (via central tegmental tract), to the contralateral dentate nucleus (via inferior cerebellar peduncle), back to the red nucleus (via superior cerebellar peduncle). This condition usually develops weeks to months after a brainstem or cerebellar infarction, although it may also occur with degenerative conditions or posttrauma (diffuse axonal injury). The delay in presentation occurs due to chronic deafferentation of the ION, which leads to a vacuolar degenerative hypertrophy and resulting disordered control of the ION (see Fig. 17.2). The term myoclonus is misleading, because the movements of affected muscles are to-and-fro and are approximately synchronized, typically at a rate of 2 to 4 cycles/sec.
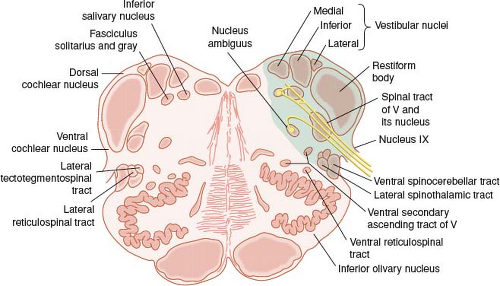 Figure 17.1 Schematic drawing of the medulla oblongata. The specific neural structures that are commonly damaged in Wallenberg syndrome are shaded. |
A majority of cases present with vertical pendular oscillations that often have a vertical and torsional component. The oscillations can resemble seesaw nystagmus but lack the alternation in elevation seen in the latter. These oscillations are associated with rhythmic undulations of the soft palate (see Video 17.1). Relatively high-dose gabapentin (1,200 to 2,400 mg daily) is commonly tried to improve the eye movements.
Occasionally, acute disease processes are restricted to the vestibular nuclei. For example, vertigo may be the sole symptom of an exacerbation of multiple sclerosis (MS) and of brainstem ischemia. Nystagmus caused by disease of the vestibular nuclei may be purely horizontal, vertical, or torsional. Mixed patterns also may occur. Moreover, nystagmus from a central vestibular lesion can mimic that caused by peripheral vestibular disease. Dolichoectasia of the basilar artery may produce a variety of combinations of central and peripheral vestibular syndromes. Microvascular compression of the vestibulocochlear nerve may also give rise to paroxysmal vertigo.
Wallenberg Syndrome (Lateral Medullary Infarction)
Typically, lesions of the vestibular nuclei also affect neighboring structures, especially the cerebellar peduncles and perihypoglossal nuclei. The best recognized syndrome involving the vestibular nuclei is caused by a lateral medullary infarction (Wallenberg syndrome) (see Fig. 17.1). The typical findings of Wallenberg syndrome are ipsilateral impairment of pain and temperature sensation over the face, central Horner syndrome, limb ataxia, and a bulbar disturbance causing dysarthria and dysphagia. Contralaterally, pain and temperature sensation are impaired over the trunk and limbs. Vertical diplopia due to a skew deviation (see below) may also occur, often with an altered subjective visual vertical (ocular tilt reaction). The facial nerve may also be affected if the infarct extends more rostrally. The disorder is most commonly caused by occlusion of the ipsilateral vertebral artery; occasionally, the posterior inferior cerebellar artery (PICA) is selectively involved (Fig. 17.3). Dissection of the vertebral artery (either spontaneous or traumatic, such as following chiropractic manipulation) is occasionally the cause. Rarely, demyelinating disease produces this syndrome.
Lateropulsion, a compelling sensation of being pulled toward the side of the lesion, is often a prominent complaint of patients with Wallenberg syndrome and is also evident in the ocular motor findings. If the patient is asked to fixate straight ahead and then gently close the lids, the eyes deviate conjugately toward the side of the lesion. This is reflected by the corrective
saccades that the patient must make on eye opening to reacquire the target. Lateropulsion may even appear with a blink.
saccades that the patient must make on eye opening to reacquire the target. Lateropulsion may even appear with a blink.
Saccadic eye movements are also affected by lateropulsion (Fig. 17.4). Horizontally, saccades directed toward the side of the lesion usually overshoot the target, and saccades directed away from the side of the lesion undershoot the target; this is referred to as ipsipulsion of saccades and should be differentiated from the contrapulsion of saccades that occurs with infarcts from occlusion of the superior cerebellar artery (SCA). Quick phases of nystagmus are similarly affected in Wallenberg syndrome, so saccades directed away from the side of the lesion are smaller than those directed toward the lesion. On attempting a purely vertical refixation, the patient produces an oblique saccade directed toward the side of the lesion. Corrective saccades then bring the eyes back to the target.
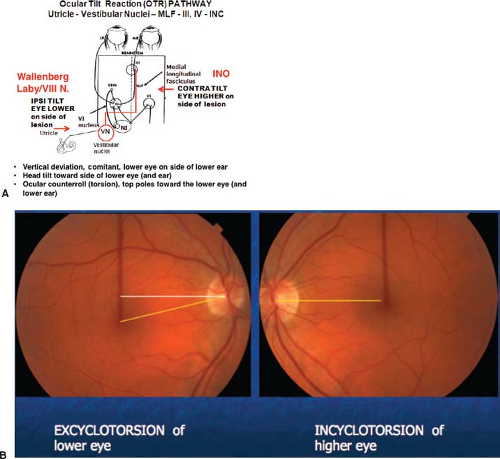
When present, spontaneous nystagmus in Wallenberg syndrome is usually horizontal or mixed horizontal–torsional with a small vertical component. In primary position, the slow phase is directed toward the side of the lesion (“beats toward the better ear”), although it may reverse direction in eccentric positions, suggesting coexistent abnormalities of the gaze-holding mechanism. Lid nystagmus (synkinetic lid twitches with horizontal quick phases) can also occur. The ocular tilt reaction (OTR) commonly occurs in Wallenberg syndrome, including a skew deviation, with an ipsilateral hypotropia. There is a conjugate yet asymmetric degree of cyclotorsion of both eyes—the higher eye incyclotorts, while the hypotropic eye excylotorts more significantly. Some patients show ipsilateral head tilt (toward the lower eye). The skew deviation and head tilt arise from imbalance in pathways mediating otolith responses (Fig. 17.5). The
subjective sensations of tilt or inversion of the world probably also reflect involvement of central projections from the gravireceptors, the utricle and saccule.
subjective sensations of tilt or inversion of the world probably also reflect involvement of central projections from the gravireceptors, the utricle and saccule.
Syndrome of the Anterior Inferior Cerebellar Artery
The anterior inferior cerebellar artery (AICA) supplies portions of the vestibular nuclei, adjacent dorsolateral brainstem, and inferior lateral cerebellum. In addition, the AICA is the origin of the labyrinthine artery in most persons and also sends a twig to the cerebellar flocculus in the cerebellopontine angle. Consequently, ischemia in the distribution of the AICA may cause vertigo, vomiting, hearing loss, facial palsy, and ipsilateral limb ataxia, along with gaze holding and pursuit deficits as well as vestibular nystagmus. The ocular motor signs reflect a combination of involvement of the labyrinth, vestibular nuclei, and the flocculus.
Syndrome of the Superior Cerebellar Artery
Infarction in the territory of the SCA causes ataxia of gait and limbs and vertigo (Fig. 17.6). A characteristic abnormality is saccadic contrapulsion. This consists of an overshooting of contralateral saccades and an undershooting of ipsilateral saccades. Attempted vertical saccades are oblique, with a horizontal component away from the side of the lesion. Thus, this saccadic disorder is the opposite of the saccadic ipsipulsion seen in Wallenberg syndrome and probably reflects interruption of outputs from the fastigial nucleus running in the uncinate fasciculus next to the superior cerebellar peduncle. Infarction restricted to
the posterior-inferior vermis can selectively impair pursuit and optokinetic eye movements.
the posterior-inferior vermis can selectively impair pursuit and optokinetic eye movements.
Skew Deviation and the Ocular Tilt Reaction
Skew deviation is a vertical misalignment of the visual axes caused by a disturbance of prenuclear inputs—there is an imbalance in otolithic inputs (i.e., otolith–ocular pathways). Torsional and horizontal deviations may be associated findings. The hypertropia may be the same in all positions of gaze (comitant), or it may vary and may even alternate (e.g., right hypertropia on right gaze, left hypertropia on left gaze) (incomitant or noncomitant). When skew deviation is incomitant—and especially in the pattern of an individual muscle palsy—it can be differentiated from a vertical extraocular muscle palsy by the coexistence of signs of central neurologic dysfunction, and attention to the direction of cyclotorsion (see Fig. 17.7). The utricular–ocular imbalance can often be overridden by altered patterns of otolith stimulation (upright-supine test) affirming the supranuclear origin of the misalignment. Recent studies have shown that in patients with a purely supranuclear deficit (no associated cranial nerve involvement), that the amplitude of vertical and torsional misalignment measured when upright, reduces by at least one-half when the patient is placed in the supine position.
Skew deviation occurs with a variety of abnormalities in the vestibular periphery, brainstem, or cerebellum and rarely as a reversible finding with raised intracranial pressure (ICP) from supratentorial tumors or pseudotumor cerebri. In infants, a skew deviation may be the harbinger of a subsequent horizontal strabismus.
Utricular projections from the vestibular nuclei probably cross the midline and ascend in the medial longitudinal fasciculus (MLF). Therefore, unilateral internuclear ophthalmoplegia (INO) is often associated with a skew deviation. The INO usually is on the side of the hypertropic eye, possibly because lesions of one MLF cause an imbalance of ascending otolithic inputs (Fig. 17.5).
In the midbrain, otolith projections contact the oculomotor and trochlear nerve nuclei, as well as the INC. Mesencephalic lesions in or around the INC thus may cause skew deviation and the OTR. When the head tilt is sustained (tonic), it is contralateral to the side of the lesion; in addition, there is usually a hypertropia that is ipsilateral to the lesion and a conjugate cyclotorsion that is characterized by intorsion of the ipsilateral eye. (Fig. 17.5). Associated defects of vertical eye movements and oculomotor or trochlear nerve function are common, including seesaw, pendular, or upbeat nystagmus.
Rarely, skew deviation slowly alternates or varies in magnitude over the course of a few minutes. The periodicity of the phenomenon is reminiscent of periodic alternating nystagmus (PAN), and the two phenomena can, in fact, coexist. Patients with this condition usually have midbrain lesions, while patients with PAN typically have lesions of the cerebellar nodulus.
Ocular Motor Syndromes Caused by Lesions of the Cerebellum
Clinicians are appropriately cautious in attributing eye movement abnormalities specifically to cerebellar dysfunction, because the brainstem is so frequently damaged in patients with lesions of the cerebellum. Nevertheless, most clinical and experimental studies provide convincing evidence that cerebellar lesions alone can cause specific ocular motor abnormalities (Figs. 17.8 and 17.9). In essence, three principal syndromes can be identified: the syndrome of the dorsal vermis and underlying posterior fastigial nuclei, the syndrome of the flocculus and paraflocculus, and the syndrome of the nodulus and ventral uvula. The main features of each of these syndromes are summarized in Fig. 17.10.
Location of Lesions and Their Manifestations
Experimental lesions of the dorsal vermis (lobules VI and VII) and of the underlying fastigial nuclei (called the fastigial oculomotor region or FOR) cause saccadic dysmetria, typically hypometria, when the vermis alone is involved, and hypermetria when the deep nuclei are affected (see Figs. 17.8 to 17.10). Bilateral lesions of the deep nuclei may sometimes lead to macrosaccadic oscillations, as a result of an extreme degree of hypermetria.
Experimental lesions of the flocculus and paraflocculus cause gaze-evoked nystagmus, rebound nystagmus, and downbeat nystagmus (see Fig. 17.8). Unilateral lesions produce ipsilateral deficits in pursuit and gaze holding. The flocculus sends climbing fibers via the inferior cerebellar peduncle to support the horizontal and vertical neural integrators. Without this input, the integrators’ output is not sustained (“leaky”) resulting in impaired gaze holding (gaze-evoked nystagmus and postsaccadic drift).
Experimental lesions of the nodulus lead to unwanted perseveration of vestibular responses resulting from a dysregulation of the “velocity storage mechanism.” This predisposes the animal to the development of periodic alternating nystagmus, failure of tilt suppression of postrotatory nystagmus, and loss of habituation. Positional nystagmus usually occurs with lesions of the nodulus.
Another ocular motor sign attributable to a focal cerebellar lesion is torsional nystagmus during vertical pursuit. Patients with lesions in the middle cerebellar peduncle show this phenomenon. The direction of the torsional nystagmus changes with the direction of the pursuit, with the eye velocity of the slow phase of the torsional nystagmus being directly proportional to the eye velocity of the slow phase of pursuit.
The cerebellum is also important in long-term adaptive functions that keep eye movements
appropriate to the visual stimulus. For example, adaptation of the gain of the VOR is impaired in patients with cerebellar lesions. This adaptive or “repair shop” function of the cerebellum probably accounts for both the enduring nature of the ocular motor deficits that accompany diffuse cerebellar lesions and, perhaps, the somewhat variable effects of cerebellar lesions. Thus, inherent, idiosyncratic abnormalities in brainstem or peripheral ocular motor mechanisms that are normally “repaired” by the cerebellum may reappear after cerebellar lesions.
appropriate to the visual stimulus. For example, adaptation of the gain of the VOR is impaired in patients with cerebellar lesions. This adaptive or “repair shop” function of the cerebellum probably accounts for both the enduring nature of the ocular motor deficits that accompany diffuse cerebellar lesions and, perhaps, the somewhat variable effects of cerebellar lesions. Thus, inherent, idiosyncratic abnormalities in brainstem or peripheral ocular motor mechanisms that are normally “repaired” by the cerebellum may reappear after cerebellar lesions.
Etiologies
Developmental Anomalies
The Arnold-Chiari malformation is an anomaly of the hindbrain involving the caudal cerebellum (including the vestibulocerebellum, flocculus, paraflocculus [tonsils], uvula, and nodulus) and the caudal medulla. In the type 1 malformation, the cerebellar tonsils are displaced caudally into the foramen magnum, and the medulla is elongated. A meningomyelocele usually is not present. Such patients often present with symptoms
in adult life. In the type 2 malformation, both the fourth ventricle and the inferior vermis extend below the foramen magnum, the brainstem and spinal cord are thin, and a lumbar meningomyelocele is usually present. Patients with a type 2 malformation usually present in childhood, but in milder cases, the onset of symptoms is delayed until adulthood. Presenting symptoms include oscillopsia that is brought on or exacerbated by head movements, and Valsalva-induced dizziness, vertigo, cervical pain, and headaches. A variety of ocular motor abnormalities, especially downbeat nystagmus (both spontaneous and positional), occur in patients with the Chiari malformation (Table 17.1). Diagnosis is by MRI, with sagittal views of the craniocervical junction being most useful (Fig. 17.11). Patients often improve after suboccipital decompression, although it may take months for the eye movement abnormalities to diminish. A similar ocular motor syndrome may be observed in patients with other lesions located at the craniocervical junction.
in adult life. In the type 2 malformation, both the fourth ventricle and the inferior vermis extend below the foramen magnum, the brainstem and spinal cord are thin, and a lumbar meningomyelocele is usually present. Patients with a type 2 malformation usually present in childhood, but in milder cases, the onset of symptoms is delayed until adulthood. Presenting symptoms include oscillopsia that is brought on or exacerbated by head movements, and Valsalva-induced dizziness, vertigo, cervical pain, and headaches. A variety of ocular motor abnormalities, especially downbeat nystagmus (both spontaneous and positional), occur in patients with the Chiari malformation (Table 17.1). Diagnosis is by MRI, with sagittal views of the craniocervical junction being most useful (Fig. 17.11). Patients often improve after suboccipital decompression, although it may take months for the eye movement abnormalities to diminish. A similar ocular motor syndrome may be observed in patients with other lesions located at the craniocervical junction.
The Dandy–Walker syndrome consists of a malformation of the cerebellar vermis, a membranous cyst of the fourth ventricle, and malformations of the cerebellar cortex and deep cerebellar nuclei. Patients with this condition often show a mild saccadic dysmetria, although some patients have normal eye movements. Ocular motor abnormalities, including nystagmus and strabismus, also occur in patients with agenesis of the vermis or hypoplasia of the entire cerebellum.
Degenerative Diseases
Many degenerative processes can affect the cerebellum or its connections and produce cerebellar eye signs. These disorders include the cerebellar cortical degenerations, ataxia telangiectasia, and various spinocerebellar and olivopontocerebellar degenerations
(OPCDs). Moreover, many of these conditions also affect brainstem structures. Thus, other, presumably noncerebellar, ocular motor signs may be present (e.g., slow saccades, prolonged saccadic latencies, decreased or absent vestibulo-ocular responses, and ophthalmoplegia).
(OPCDs). Moreover, many of these conditions also affect brainstem structures. Thus, other, presumably noncerebellar, ocular motor signs may be present (e.g., slow saccades, prolonged saccadic latencies, decreased or absent vestibulo-ocular responses, and ophthalmoplegia).
 Figure 17.10 Key clinical signs of damage to various cerebellar structures. (Original courtesy of David S. Zee, MD; modified and adapted to current format.) |
Paraneoplastic cerebellar degeneration is a rare remote effect of cancer, usually occurring with breast, ovarian, or small-cell lung cancer, and typically associated with serum and cerebrospinal fluid anti-Yo antibodies. The onset of symptoms is usually acute or subacute, with the development of severe midline and appendicular ataxia, dysarthria, and downbeat nystagmus. Pathologic studies indicate total loss of Purkinje cells in patients with this condition. Such patients have lost all output from the cerebellar cortex, and the common finding of primary position downbeat nystagmus thus tends to confirm that asymmetric, inhibitory projections of the cerebellum to the central connections of the semicircular canals can be the cause of this nystagmus. A cerebellar syndrome may also complicate treatment of cancer or leukemia with cytosine arabinoside.
Table 17.1 Eye Signs in the Chiari Malformation | |
|---|---|
|
Mass Lesions
Cerebellar hemorrhage, tumors, infarcts, abscesses, cysts, and extra-axial hematomas may all cause cerebellar eye signs by direct damage to the cerebellar parenchyma. Cerebellar lesions, however, may also compress the brainstem and produce additional signs. Vertical or horizontal gaze disorders can occur, depending on whether
the direction of compression is rostral or forward, respectively. The oculomotor, trochlear, and abducens nerves may also be affected. Ocular motor dysfunction may also be caused by secondary obstructive hydrocephalus and increased ICP.
the direction of compression is rostral or forward, respectively. The oculomotor, trochlear, and abducens nerves may also be affected. Ocular motor dysfunction may also be caused by secondary obstructive hydrocephalus and increased ICP.
Vestibular schwannomas (acoustic neuromas) may compress the cerebellar flocculus (which lies in the cerebellopontine angle) and produce eye signs of vestibulocerebellar lesions, including Bruns nystagmus in which there is a coarse (high amplitude) nystagmus beating to the side of the lesion (reflecting a gaze-holding deficit) and a fine (high frequency) nystagmus beating away from the side of the lesion (reflecting a vestibular imbalance). Acute cerebellar hemorrhage frequently causes nystagmus, gaze palsy (usually toward the side of the lesion), abducens nerve palsy, and skew deviation.
Ocular Motor Syndromes Caused by Lesions of the Pons
Lesions of the Internuclear System: Internuclear Ophthalmoplegia
Among the fibers that comprise the MLF, many carry a conjugate horizontal eye movement command from abducens internuclear neurons in the pons to the medial rectus subdivision of the contralateral oculomotor nuclear complex in the midbrain. Other fibers in the MLF carry signals for holding vertical and torsional eye position, for vertical smooth pursuit, and for the vertical VOR.
Manifestations
Lesions of the MLF produce INO (Fig. 17.12). When the lesion is unilateral, the INO is characterized by weakness of adduction ipsilateral to the side of the lesion (Fig. 17.13). This weakness can vary from a complete loss of adduction beyond the midline to a mild decrease in the velocity of adduction without any limitation in range of motion. The fibers subserving horizontal gaze in the MLF each carry commands for all types of conjugate eye movements. Thus, vestibular slow phases, pursuit and optokinetic following movements, and saccades and quick phases of nystagmus are all affected by the MLF lesion.
When patients with INO are able to converge, despite absence of voluntary adduction, a caudal lesion with preservation of the medial rectus subdivision of the oculomotor nuclear complex can be assumed. Patients with INO and intact convergence were said to have a posterior internuclear ophthalmoplegia by Cogan. Although the presence of intact convergence is important in such cases, the absence of convergence in the setting of an INO (the “anterior” INO of Cogan) does not necessarily imply a rostral lesion involving the medial rectus nuclear subdivision. Some patients simply are not able to produce a strong convergence effort, and the vertical disparity that occurs when a unilateral INO is associated with
a skew deviation (see below) also may interfere with convergence effort.
a skew deviation (see below) also may interfere with convergence effort.
The second cardinal sign of an INO is nystagmus on abduction in the contralateral eye. This nystagmus consists of a centripetal (inward) drift, followed by a corrective saccade that may be hypermetric, hypometric, or orthometric. It is present in nearly all patients with INO. The cause of abduction nystagmus must relate either to lesions outside the MLF or to an adaptive response to the initial adduction weakness. In patients with “pseudo-INO” due to disorders of the neuromuscular junction, abducting nystagmus typically does not accompany the deficit of adduction.
 Figure 17.13 Unilateral, right internuclear ophthalmoplegia in a 32-year-old man with multiple sclerosis. Note complete lack of adduction in the right eye on attempted left horizontal gaze. |
Lesions that damage the MLF may also damage the abducens nucleus, fascicle, or both on either side of the brainstem (see Fig. 17.14). Lesions that damage the MLF on one side and the ipsilateral abducens nucleus produce the one-and-a-half syndrome (see below), whereas lesions that damage the ipsilateral abducens fascicle produce horizontal ophthalmoplegia in the ipsilateral eye from the combination of an INO and an abducens nerve palsy. Damage to the MLF on one side and to the contralateral abducens nerve fascicle will produce abduction weakness of the contralateral eye combined with adduction weakness of the ipsilateral eye. In this setting, there will be a “pseudo-horizontal gaze palsy” on attempted horizontal gaze away from the side of the MLF lesion. The diagnosis may be suspected in a patient who appears to have a horizontal gaze palsy that is asymmetric, with one eye (usually the adducting eye) being much more limited than the other.
Etiologies
Table 17.2 summarizes some etiologies of INO. In general, a unilateral INO is most commonly caused by ischemia, although even in these cases there is often subtle involvement of the other side. Bilateral INO is commonly caused by demyelination. Although MRI frequently shows a lesion in the MLF in patients with INO (see Fig. 17.12), there are many exceptions where
the diagnosis is suspected and confirmed by clinical examination alone.
the diagnosis is suspected and confirmed by clinical examination alone.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree