Suprahyoid Pharyngotomy
Robert L. Ferris
INTRODUCTION
Suprahyoid pharyngotomy is a safe and efficient approach to excise carefully selected benign and malignant tumors arising in the base of the tongue and the posterior wall of the oropharynx. This technique provides excellent exposure for excision of the tumor while maintaining good function and excellent cosmesis. However, accurate assessment of the tumor in preoperative planning and meticulous attention to detail intraoperatively are the secrets for success, as in most surgical practice.
Traditionally, surgical approaches to these sites include segmental resection of the mandible with partial glossectomy, lateral pharyngotomy, and mandibulotomy. These procedures, however, may produce cosmetic deformities and interfere with deglutition, often resulting in disabling aspiration. In 1895, Jeremitsch became the first surgeon to use the suprahyoid approach. His decision was based on observation of a patient who had attempted suicide. During the attempt, a laceration was produced that approximated a pharyngotomy. Jeremitsch noted that bleeding was minimal, no nerves were severed, and the patient healed favorably.
The suprahyoid approach for T1/T2 squamous cell carcinomas of the base of the tongue has been employed for many years with normal speech, good cosmesis, swallowing without aspiration, and an excellent cure rate. The use of this approach has also been reported in the management of benign and malignant salivary gland tumors of the base of the tongue, excision of lingual thyroid, and the treatment of juvenile angiofibroma of the nasopharynx. This approach is also very efficacious in the management of limited lesions of the posterior pharyngeal wall, and limited lesions of the epiglottis. Tumors of the base of the tongue should be posterior to the circumvallate papillae; otherwise, a functional defect will be created.
HISTORY
A detailed history, clinical examination, and imaging studies are essential and may provide additional insights into the etiology of the lesion. Patients presenting with an oropharyngeal neoplasm have a number of presenting symptoms, such as an asymptomatic mass in the neck, change in speech and swallowing, pain, hemoptysis, otalgia, and trismus. In the past, a majority of the patients who presented with squamous carcinoma had a pertinent history of tobacco and alcohol use. Subsequently, with the emergence of human papilloma virus, many of these patients no longer have the traditional risk factors. The patient should be questioned regarding nutritional status and weight loss.
PHYSICAL EXAMINATION
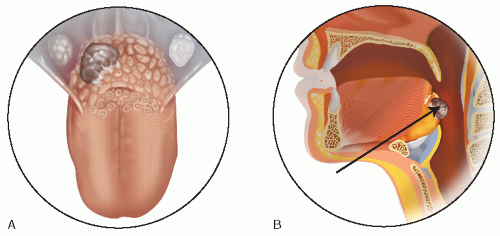
A thorough head and neck examination should include a transoral view of the oral cavity and oropharynx. The superior surface of the cancer may be seen in cooperative patients using a tongue blade to depress the base of tongue (BOT) (Fig. 8.1). Fiberoptic endoscopy should also be performed to assess the lateral and inferior extent of the tumor mass, as well as its bulk and involvement of surrounding structures. The neck should be palpated carefully, particularly ipsilateral to the tumor, with a focus on level II, the most common site for lymph node metastasis for cancers of the oropharynx. Clinical staging using physical examination should be corroborated with radiographic imaging to ensure correct patient selection.
INDICATIONS
T1/T2 squamous cell cancer of the base of the tongue as well as other small malignant or benign tumors of the posterior wall of the oro- or hypopharynx may be excised with this technique. Primary closure of the mucosa of the posterior pharyngeal wall to prevertebral fascia or reconstruction with a split-thickness skin or dermal graft can be used for reconstruction of the defect.
CONTRAINDICATIONS
Excision of a cancer larger than T2 is not recommended because to obtain clear margins for a larger tumor, the entire posterior wall, including the muscles of deglutition, will be resected, resulting in dysphagia and aspiration problems. Resection of the base of the tongue anterior to the circumvallate papillae is a relative contraindication to this approach, because the defect would be difficult to close primarily, the anterior margin of resection may be compromised, and dysphagia and aspiration are predictable complications. Involvement of the lateral pharyngeal wall or tonsil may require extension of the approach, such as adding a lateral pharyngotomy to provide adequate exposure.
PREOPERATIVE PLANNING
Correct preoperative staging is essential to determine whether suprahyoid pharyngotomy is the best surgical approach for limited squamous cell carcinoma, adenocarcinoma, benign tumors of the base of the tongue, or tumors including squamous cell carcinoma of the posterior pharyngeal wall. Physical examination, especially palpation, remains the most important aspect of the evaluation. Magnetic resonance imaging (MRI) has proved to be the most sensitive modality for evaluating tumors involving the base of the tongue because it provides excellent soft tissue definition, and fine-cut computed tomography (CT) scanning also provides useful preoperative information (Fig. 8.2). Gross invasion of the preepiglottic space and the depth of infiltration into the base of the tongue may be determined by obtaining sagittal MRI scans of the tongue base-larynx complex. This information is of importance because patients with involvement of the preepiglottic space, with or without involvement of the epiglottis, are not candidates for this technique. The high signal intensity of the preepiglottic adipose tissue usually can be distinguished from the dense fibers of the hyoepiglottic ligament, tongue base musculature, lingual lymphoid tissue, and cancer.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree