Superior Limbic Keratoconjunctivitis
Thanh Hoang-Xuan
Superior limbic keratoconjunctivitis (SLK) is characterized by chronic inflammation of the ocular surface, which can be easily overlooked (still too often the case) if one does not carefully examine the eye while keeping in mind the clinical suspicion of the possibility of SLK. The patient may then continue to suffer highly incapacitating symptoms unnecessarily (effective treatments are available) and be exposed to inappropriate drug therapy with its attendant adverse effects. The etiopathogenesis of SLK is unclear.
The initial description is attributed to Frederick Theodore (1), who in 1961 reported the first cases of an entity that, in 1963 (2), he named superior limbic keratoconjunctivitis. His 11 patients had chronically recurrent lesions of the superior bulbar and palpebral conjunctivas and adjacent cornea, taking the form of superficial punctuate keratitis, which often was complicated by filamentary keratitis (2). A similar form of keratitis had in fact been described 8 years earlier by Braley and Alexander (3). At first, SLK and Thygeson’s keratitis were considered to be different forms of the same entity (4,5), but Theodore subsequently completed the description of SLK on the basis of new cases (6,7).
EPIDEMIOLOGY
Although SLK can occur in both sexes and at all ages, it is most frequent in the middle-aged and in women, the latter accounting for 70% of cases (8). All cases reported so far have been sporadic, with the exception of affected twins (9). SLK is usually bilateral (70% of cases), but can be asymmetrical. Hyperthyroidism is found in 20% to 50% of patients with SLK (2,8,10, 11, 12, 13, 14, 15).
CLINICAL ASPECTS
The diagnosis of SLK is often overlooked and thus delayed, yet the signs are highly evocative if one simply remembers to look for them. SLK is generally missed because the symptoms are often nonspecific and the nearly pathognomonic ocular lesions are hidden by the upper eyelid. The natural course of SLK is chronic, remitting/relapsing, and lasting many years; exacerbations are followed by increasingly lengthy remissions, and spontaneous recovery is the rule (2,6). Although SLK has a good visual prognosis (the central cornea is spared), the symptoms during exacerbations are too incapacitating to allow patients to wait, untreated, for spontaneous recovery.
The lack of specific ocular symptoms explains the frequent delay in diagnosis. The ocular manifestations generally consist of discomfort, foreign-body sensation, burning sensation, and photophobia. The intensity of symptoms is highly variable. Dry-eye syndrome and meibomian gland dysfunction are usually suspected. SLK should be suspected when the patient presents with superior bulbar conjunctival hyperemia that mainly affects the limbus and the adjacent bulbar conjunctiva. Blepharospasm and pseudoptosis can be found in severe cases with filamentous keratitis, in which mucous discharge is generally present.
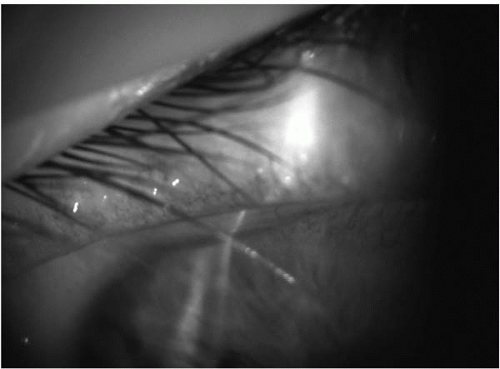
The ocular lesions are remarkable since they are limited to the upper part of the eye. Typically, one finds moderate papillary hyperplasia of the superior tarsal conjunctiva (Fig. 32-1) and hyperemia of the superior bulbar conjunctiva, generally forming a large vertical band. The bulbar conjunctiva may appear corrugated, and it is excessively mobile as one rubs the globe through the upper lid; the redness fades gradually in intensity from the limbus to the superior bulbar conjunctiva, which appears thickened and redundant (Fig. 32-2). Raber (16) reported scarring of the palpebral conjunctiva in three patients. However, the eye can have a near-normal aspect in some cases. One major diagnostic feature of SLK is the uptake of fluorescein, rose bengal, or lissamine green dye by the superior limbal conjunctiva and the upper part of the cornea in a highly characteristic way, confined to a rectangular or trapezoidal area of the bulbar conjunctiva in a punctate pattern. There is usually a superior corneal micropannus associated with the epithelial keratitis. Severe forms are associated with corneal filaments in one-third to one-half of cases (Fig. 32-3)
(6,8,17). About one-quarter of patients have lacrimal deficiency (Schirmer’s test) (8). One generally obvious feature is the lack of adherence between the superior bulbar conjunctiva and the sclera. This sign can be found by mobilizing the bulbar conjunctiva on the eyeball, either directly with a Merocel sponge after instilling an anesthetic eye drop, or indirectly with the finger through the upper eyelid (Figs. 32-1 and 32-4). This reveals conjunctival folds, parallel to the limbus, forming a sort of conjunctivochalasis. Some authors have also described concomitant inferior conjunctivochalasis (18).
(6,8,17). About one-quarter of patients have lacrimal deficiency (Schirmer’s test) (8). One generally obvious feature is the lack of adherence between the superior bulbar conjunctiva and the sclera. This sign can be found by mobilizing the bulbar conjunctiva on the eyeball, either directly with a Merocel sponge after instilling an anesthetic eye drop, or indirectly with the finger through the upper eyelid (Figs. 32-1 and 32-4). This reveals conjunctival folds, parallel to the limbus, forming a sort of conjunctivochalasis. Some authors have also described concomitant inferior conjunctivochalasis (18).
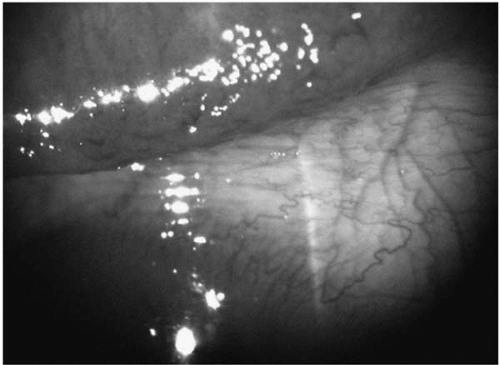 FIGURE 32-1. On instilling a drop of lissamine green in superior limbic keratoconjunctivitis, papillary hypertrophy of the superior tarsal conjunctiva is better seen, as well as the horizontal folds of the superior bulbar conjunctiva due to the poor adherence of the latter to the sclera. Also note the lucid appearance of the edematous superior limbal conjunctiva.(see color image) |
PATHOLOGY
Histologic and ultrastructural examination of the conjunctiva shows squamous metaplasia of the superior bulbar conjunctival epithelium, with a loss of goblet cells and acanthotic degeneration of epithelial cells (8,19, 20, 21). The latter have a condensed nuclear chromatin whose appearance on impression cytology is highly characteristic (“snake-like” chromatin) (22), together with cytoplasmic glycogen overload (21). The conjunctival stroma, which is edematous and contains abundant dilated lymphatics, is moderately infiltrated by inflammatory cells (23). Ultrastructurally, epithelial cells from the bulbar conjunctiva contain secondary intracytoplasmic lysosomes, keratohyalin granules, and increased numbers of condensed microfilaments that strangle the nucleus, conferring a polylobar or polynuclear aspect (21,23,24). In contrast, the palpebral conjunctiva is rich in goblet cells and its epithelium is normal. Its chorion contains abundant inflammatory cells (neutrophils, lymphocytes, and plasma cells) (15).
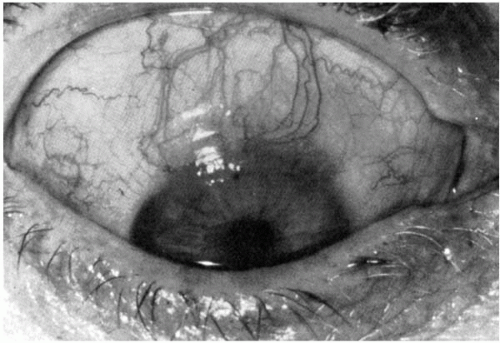 FIGURE 32-2. Hyperemia and thickening of the bulbar conjunctiva at the upper limbus in superior limbic keratoconjunctivitis. |
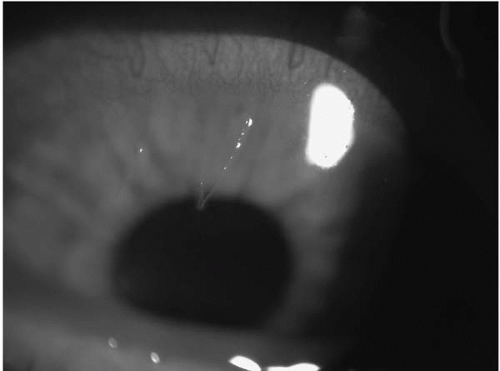 FIGURE 32-3. Filaments at the upper cornea in superior limbic keratoconjunctivitis.(see color image) |
DIFFERENTIAL DIAGNOSIS
Symptoms in patients with forms in which filamentary keratitis is absent can resemble those of miscellaneous disorders such as chlamydial conjunctivitis, Thygeson’s superficial punctate keratitis, the limbal form of vernal keratoconjunctivitis, and phlyctenular keratoconjunctivitis. In contrast, there are almost no differential diagnoses when all the characteristic signs of SLK are present. Of note, a case of sebaceous carcinoma extending to the superior bulbar conjunctival epithelium and masquerading as SLK has been reported (25). In fact, only early-stage contact lens-induced keratoconjunctivitis resembles SLK, but filaments are extremely rare in the former condition. In advanced forms, contact lens-induced keratoconjunctivitis differs from SLK by its more severe epithelial keratitis, its more diffuse and severe conjunctival inflammation, and the decreased vision (26). Bloomfield and associates (20) reported a case of bilateral vascularized stromal opacification with pannus formation, necessitating keratoplasty (the patient refused to stop using her contact lenses). Generally, contact lens withdrawal leads to recovery (26, 27, 28). Contact lens-induced keratoconjunctivitis is attributed by some authors to an allergic hypersensitivity reaction to lipoprotein deposits on the lens or to the preservatives—especially thimerosal—contained in the contact lens care solutions (26). Fuerst et al. (27) reported finding no cases of hypersensitivity to preservatives in their patients with contact lens-induced keratoconjunctivitis. According to Carpel (29), contact lens-induced keratoconjunctivitis is due to the mechanical effect of the lens rubbing on the superior bulbar conjunctiva and cornea.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree