Purpose
In Descemet membrane endothelial keratoplasty (DMEK), lamellar splitting of the Descemet membrane (DM) may occur during stripping of host DM, leaving residual DM on the recipient’s DMEK interface. The purpose of this study was to determine the incidence rate of lamellar splitting of DM during DMEK and to describe the ultrastructure of DM in these eyes.
Design
Retrospective consecutive case series.
Methods
setting : Institutional, single-center. patient population : Total of 664 eyes with Fuchs endothelial corneal dystrophy (FECD) scheduled for primary DMEK. intervention : DMEK. main outcome measures : The incidence rate of lamellar DM splitting in the recipients’ eyes; ultrastructural alterations of stripped DM specimens (transmission electron microscopy); preoperative best-corrected visual acuity (BCVA), central corneal thickness (CCT), and prevalence of diabetes mellitus.
Results
Sixty-three of 664 eyes (9.5%) with FECD showed lamellar splitting of DM resulting in the dissociation of 2 separate layers. Transmission electron microscopy revealed accumulations of banded and wide-spaced collagen between the thicker posterior banded layer and the thin anterior banded layer, which is adhesive to the corneal stroma. Lamellar splitting occurred along these abnormal collagen inclusions, demarcating the borderline between both layers of DM.
Conclusions
Lamellar DM splitting occurs during DM stripping in almost 10% of eyes with FECD. This phenomenon appears to be caused by abnormal collagenous material deposits at the borderline between anterior and posterior layers of DM.
Descemet membrane endothelial keratoplasty (DMEK) is a surgical technique that selectively replaces the diseased corneal endothelium in the treatment of corneal endothelial disorders, such as Fuchs endothelial corneal dystrophy (FECD), by transplantation of the endothelium–Descemet membrane (DM) complex. DM can be separated relatively easily from the adjacent stroma. During DMEK this separation is achieved by stripping the DM along its physiological interface between the interfacial matrix zone and posterior stromal collagen lamella in both the donor’s and host’s cornea. Although DM grafts can be manually prepared with a high level of reproducibility (98%), a small percentage of donor corneas (2%) reveal individual tissue properties that may complicate or prevent proper DM stripping owing to an exceptionally strong adhesion of DM to the posterior stroma, which results in lamellar splitting, mostly between the DM’s anterior banded and posterior nonbanded layers.
Lamellar splitting of DM can also occur when stripping the host’s DM, leaving residual DM on the recipient’s interface in Descemet stripping automated endothelial keratoplasty (DSAEK). Retained remnants of DM seem to be a major cause for graft detachment in the recipient’s eye after DSAEK. Despite its clinical relevance, this particular phenomenon has not been systematically analyzed. Although it has not been described in DMEK until now, the occurrence of DM splitting should be expected in DMEK surgery as well, because the descemetorrhexis method is the same in DMEK as in DSAEK. Tourtas and associates showed a higher graft detachment rate in eyes undergoing DMEK in which the descemetorrhexis is smaller than the graft diameter, resulting in an overlapping zone of the recipient’s DM and the graft. This situation is functionally similar to retained DM fragments, because both result in a DM-DM interface.
Graft detachments are still the main postoperative complication and challenge in DMEK surgery. Modification of the surgical technique (eg, using an oversized descemetorrhexis or a larger air bubble size) has reduced the rate of graft detachments.
The purpose of this study is to assess the incidence rate of lamellar splitting of host DM in a large consecutive series of eyes with FECD during primary DMEK and to investigate the ultrastructure of the stripped DM fragments.
Methods
In a retrospective, single-center, consecutive case series, 664 eyes with FECD scheduled for primary DMEK between July 2014 and July 2015 were assessed intraoperatively for the occurrence of lamellar splitting during DM stripping. The host DM was removed from the stroma under air using an inverted hook (Price Endothelial Keratoplasty Hook; Moria SA, Antony, France) in a central 9-mm area. Signs of lamellar splitting of DM were assessed by the surgeon. All surgeries were performed by a single surgeon (F.E.K.). All eyes that were phakic at the time of planned surgery underwent DMEK with simultaneous cataract surgery (triple DMEK) as previously described. This proceeding was chosen in order to avoid the necessity of secondary phacoemulsification, which might adversely affect endothelial function after DMEK.
The stripped DM tissue was collected and cryopreserved routinely for further studies in our department. Informed consent was obtained from all patients for both the surgery and the cryopreservation of DM tissue for further ultrastructural and molecular-biological analyses.
The study complied with the tenets of the Declaration of Helsinki and adhered to all state laws of the country. The Institutional Review Board of the University of Erlangen-Nürnberg, Germany waived the need for approval.
Clinical Evaluation
In order to investigate predisposing factors for DM splitting, we analyzed the following clinical parameters in a subset of eyes (63 eyes in each group): preoperative best-corrected visual acuity (BCVA) and central corneal thickness (CCT; Pentacam; Oculus, Wetzlar, Germany) as measures for the clinical stage of the endothelial dysfunction. Significant graft detachment requiring a repeated air injection was defined as the detachment of more than 1 quadrant of the graft with a gap of more than 1 corneal thickness. The medical history of diabetes was taken.
Transmission Electron Microscopy
Stripped DM specimens were fixed in 2.5% glutaraldehyde in 0.1 M phosphate buffer, postfixed in 2% buffered osmium tetroxide, dehydrated in graded alcohol concentrations, and embedded in epoxy resin according to standard protocols. Ultrathin sections were stained with uranyl acetate and lead citrate and examined with a transmission electron microscope (EM 906E; Carl Zeiss AG, Oberkochen, Germany).
Statistical Analysis
IBM SPSS software version 20.0 (SPSS, Armonk, New York, USA) was used for statistical analysis. Differences between groups were assessed by Mann-Whitney U test. Categorical data were analyzed with χ 2 test. The significance level was set at P = .05.
Results
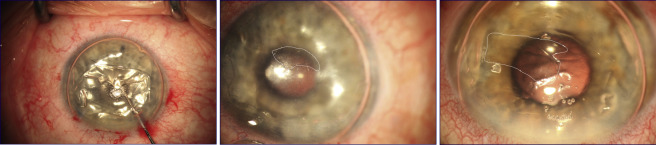
Lamellar splitting of DM occurred intraoperatively in 63 of 664 eyes (9.5%) with FECD during DM stripping. The lamellar splitting resulted in the dissociation of 2 separate DM layers: a posterior thicker lamella, which could be easily removed, and an anterior delicate brittle lamella, which adhered to the corneal stroma in total or at several spots. The occurrence of lamellar splitting could be recognized at the operation microscope by an altered light reflex and a fine demarcation line on the posterior corneal surface under air ( Figure 1 ). In these cases, descemetorrhexis required several attempts to completely remove the adhesive anterior DM layer. Eyes were examined meticulously at the operation microscope for remnants of DM under air, which were entirely removed in all eyes. The dissociated fragments of DM were separately fixed and processed for transmission electron microscopy.
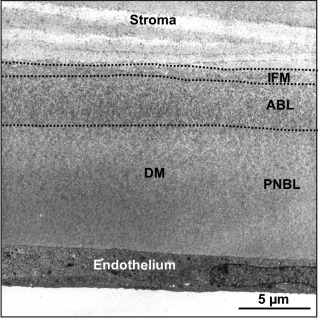
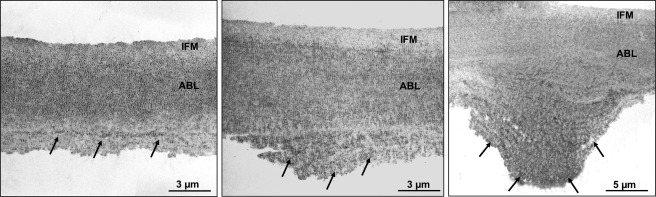
The normal Descemet membrane is composed of an anterior banded (fetal) layer, a posterior nonbanded (postnatal) layer, and a narrow transitional interfacial matrix zone mediating adhesion to the corneal stroma ( Figure 2 ). Transmission electron microscopy of selected specimens (n = 13), classified to exhibit pronounced splitting, revealed the adhesive anterior layer (4–8 μm thick) to comprise an anterior banded (fetal) layer of DM that contained abnormal accumulations of banded and wide-spaced collagen along its posterior aspects, only occasionally forming wart-like structures ( Figure 3 ).
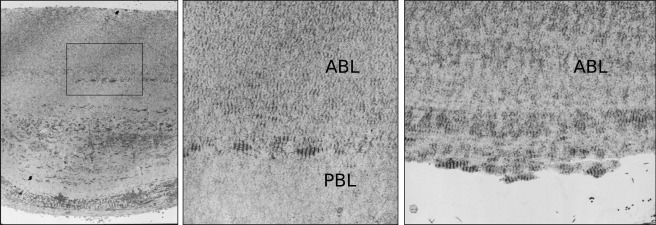
The posterior thicker layer, which was easily removed, was found to comprise an abnormal posterior banded (postnatal) layer of DM (10–20 μm thick) containing accumulations of banded and wide-spaced collagen throughout its entire width ( Figure 4 , Left). In areas allowing complete removal of DM, lamellar splitting was seen to occur between anterior and posterior banded layers along abnormal collagen material inclusions demarcating the borderline between both layers of DM ( Figure 4 , Middle/Right).
In order to analyze possible predisposing factors for DM splitting, we compared several clinical parameters of eyes with lamellar splitting (n = 63) to the first 63 consecutive control eyes with regular stripping out of 664 eyes. All eyes that were phakic at the time of surgery underwent triple DMEK: DMEK with simultaneous cataract surgery was performed in 41 of 63 eyes (65%) with lamellar splitting and in 32 of 63 eyes (51%) without lamellar splitting ( P = .074). There were no significant differences regarding age, preoperative BCVA, and preoperative CCT between FECD eyes with regular DM stripping and those with lamellar DM splitting ( Table ). Fourteen of 63 eyes (22%) with lamellar splitting and 11 of 63 eyes (17%) without lamellar splitting had the diagnosis of diabetes mellitus type 2 ( P = .328). Repeated air injections owing to graft detachments were necessary in 13 of 63 eyes (21%) with lamellar splitting and in 19 of 63 eyes (30%) without lamellar splitting ( P = .153).



