Septoplasty
Grant S. Gillman
INTRODUCTION
Accounts of surgical procedures designed to establish a normal anatomic nasal airway can be found as far back as the late 19th century. In fact, some of the most recognized names in surgery have been associated with descriptions of surgical techniques and innovations to improve nasal airway surgery, including Asch, Killian, Freer, Metzenbaum, Cottle, Converse, and Goldman among others.
Nonetheless, success and patient satisfaction rates reported within the literature often hover around 70%. This would suggest that the way we think about the problem and the teaching of the surgical correction of the nasal airway must be revisited, broadened, and continually honed.
Any number of structural deformities might affect the nasal septum. The obstruction might be cartilaginous, bony, or both. One might see tilts to the septum, curves, spurs, twists, angulations, telescoping segments, or any combination of these. Septal deviations might occur within a nasal framework that is externally straight, crooked, twisted, or collapsed. The airway might be compromised at the internal nasal valve, the external nasal valve, both, or neither. Considered in this light, it is simplistic to think that there might be one operation to correct all nasal airway problems. Furthermore, it becomes self-evident that routinely applying a single “standard” operation to all patients presenting with nasal obstruction and a deviated septum is doomed to fail in a significant number of cases from the outset. In essence, there is no “one-size-fits-all” solution to this variable, complex, and often underappreciated challenge.
“Septoplasty” is best thought of as a reconstructive procedure. Only then does one begin to do away with the notion of any single “standard” excisional procedure and instead proceed more creatively to design an operation tailored to the particular needs of and unique deformity in each patient. At the same time, this very construct makes it virtually impossible to describe how to address all possible circumstances that the surgeon might encounter. At the very least, however, a foundation for more thoughtful, considered surgery will provide a basis upon which surgical experience can be developed, and with greater surgical experience, more consistent outcomes and more grateful patients will inevitably follow. With that in mind, I will endeavor to provide some general guidelines for the more basic or routine deformities. Equally importantly, I will endeavor to provide some recommendations on how to identify circumstances that are less routine and that would warrant more advanced surgical intervention in order to minimize failure and maximize success rates.
HISTORY
Relevant documentation for the patient presenting with complaints of nasal airway obstruction should include the following:
Duration of the symptoms
A history of previous nasal surgery
History of nasal trauma
Identification of the more subjectively symptomatic side, if there is one
The presence or absence of environmental allergies or triggers for nasal congestion. The patient with allergic rhinitis and a deviated septum must understand that surgery can only relieve the obstructive structural component and that ongoing treatment of the inflammatory (allergic) congestion component will be necessary if one is to optimize the nasal airway. Discussing this prior to surgery (and not afterward) will set appropriate expectations and should better facilitate compliance with postoperative medical management.
Any trial of and response to oral antihistamines, oral decongestants, nasal steroid sprays, nasal antihistamines and nasal dilating strips. This can help alert the clinician to possible allergic rhinitis and nasal valve issues respectively.
Use of over-the-counter nasal decongestant sprays
Any history of recurrent or chronic sinusitis
Any history of recurrent or prolonged epistaxis
Any history of sleep-disordered breathing/sleep apnea
The patient’s impression of his/her sense of smell
History of cocaine use (if suspected)
PHYSICAL EXAMINATION
First and foremost, the physical examination of the patient presenting with nasal airway obstruction should be an open-minded evaluation of all possible sources of obstruction. I begin with observation of the patient from both a frontal view and base view, without a speculum in place, with the patient breathing normally and naturally through the nose in order to identify any instability of the nasal sidewall or dynamic inspiratory collapse of the nasal valve. From the base view, one can also identify caudal septal deflections and asymmetry of the nostrils.
I then proceed to anterior rhinoscopy. The importance of a careful and very deliberate examination of the nasal valve cannot be overstated. Unrecognized nasal valve compromise is a common reason for which surgeons might fail to correct a nasal airway issue with a septoplasty—particularly valve compromise in the region of either the dorsal or caudal septal struts. If a speculum is passed into the nose too far and too quickly, the examiner can easily overlook or bypass pathology of the nasal valve. As such, anterior rhinoscopy must be a patient, thoughtful and critical appraisal of all potential sites of obstruction. Deviations of the septum should be described in as specific and detailed a fashion as possible (see section on Preoperative Planning).
If a septal perforation is identified, it should be documented and pointed out to the patient. I routinely do nasal endoscopy so that I do not inadvertently overlook a less obvious source of obstruction beyond a more readily apparent septal deflection.
An ear curette or the wooden stick end of a cotton-tipped applicator can be used either to stabilize the collapsing nasal sidewall (upper or lower lateral cartilage) if present or to lateralize an already collapsed (medialized) sidewall segment during inspiration. This can determine whether or not such a maneuver is beneficial to the patient with suspected nasal valve compromise or instability of the nasal sidewall.
With a gloved hand straddling the columella between the thumb and index finger, I palpate the caudal septum of every patient. I am often surprised by the frequency of involvement of the caudal segment of the quadrangular cartilage. Subtle caudal septal deflections can easily be “hidden” behind the columella (and are therefore less apparent on visual evaluation). Nonetheless, such deflections can have a significant impact on the airway if this segment of the cartilage is bowing to one side or the other and impinging on the nasal valve angle or displaced off the anterior nasal spine and maxillary crest. Furthermore, by palpating the septum I can appreciate whether the underlying cartilage is weak and flimsy, or firm and more supportive.
In any patient who has had prior surgery, I palpate further back along the septum with a cotton swab in an effort to determine how much or how little septal cartilage is still present to work with.
To summarize, the physical examination of the patient with a deviated septum should focus on the broader configuration of the cartilaginous and bony septum itself, with particular attention paid to the dorsal septum/internal nasal valve, the caudal septum/external nasal valve, the stability of the nasal sidewall, and the presence or absence of alternative sources of nasal airway obstruction such as a mass, polyp, or adenoid hypertrophy.
INDICATIONS
The primary indication for nasal septoplasty surgery is to improve the nasal airway and therefore the diseasespecific quality of life in the patient with a symptomatic nasal septal deviation.
Other indications might include
Facilitating access to the middle meatus in endoscopic sinus surgery
Enabling the management of epistaxis occurring posterior to a deflected septal segment
Facilitating access to the pituitary through the sphenoid sinus
Facilitating harvest of septal cartilage for reconstructive purposes, as in nasal reconstruction
Contributing as part of a more comprehensive approach to reducing upper airway resistance in the patient with sleep apnea/sleep-disordered breathing
Relieving headaches or facial pain presumed to originate from septal contact points (controversial)
CONTRAINDICATIONS
The primary contraindication to septal surgery would be a patient in whom medical comorbidities make that patient unsuitable for a general anesthetic. Patients taking anticoagulants that cannot be held or those with any bleeding disorder would merit deferral of surgery. Active and frequent overuse of any topical over-the-counter nasal decongestant sprays and/or cocaine abuse would contraindicate surgical intervention at that time.
Lastly, patients whose goals or expectations regarding surgical outcomes are completely discordant with the measurable objective of the surgical procedure (e.g., those seeking resolution of postnasal drip, cure of a headache in the absence of any symptomatic nasal obstruction, or elimination of chronic cough) are likewise not good candidates for surgery as it may well be impossible to meet their unrealistic expectations.
PREOPERATIVE PLANNING
Upon completion of the physical examination, the surgeon should be able to describe or classify the septal deformity in detail. Limited descriptions such as “deviated nasal septum (DNS), left” or “nasoseptal deviation (NSD), right” are so vague in specifics as to be meaningless for they offer little guidance for the operation. It would be akin to saying simply “cancer, head and neck” or “disease, middle ear,” which would provide no direction to the head and neck surgeon or otologist, respectively.
If all septal deflections were fundamentally similar and one generic operation could be used for all patients, then perhaps such nondescript narratives would suffice. If, on the other hand, we go back to the concept that the correction of septal deflections is a calculated reconstructive procedure individualized for each particular patient, then detailing observations such as angulations, curvatures, spurs, findings within the valve region, and caudal septal irregularities will inevitably begin to focus a more targeted surgical strategy, which in turn should result in improved outcomes.
Imaging is not routinely necessary to diagnose septal or nasal valve pathology but is warranted if there is any suspicion of an alternative obstructive or inflammatory nasal mass.
In order to succeed, the surgeon must begin by knowing when the “routine” septoplasty will fail. The preoperative identification of more complex, high-risk circumstances or sites of potential failure is therefore paramount. With the physical examination complete, the surgeon should ask the following questions:
Is there a problem with the nasal valve?
Is there a dorsal deviation?
Is there a caudal septal deviation?
Are there complex deformities in regions critical to nasal support that cannot be treated with excisional techniques and may require reconstruction or reimplantation of cartilage?
Can the patient’s problem be corrected endonasally, or does the patient really need a functional external approach septorhinoplasty?
And finally—given all this information, is the correction of this patient’s deformity within the surgeon’s skill set, or should this be referred on to someone with the requisite experience needed for this particular case?
Informed Consent
Informed consent should, at a minimum, include mention of the risks of:
Excessive bleeding.
Wound infection.
Sinusitis secondary to placement of the splints.
The need for secondary/revision surgery, that is, insufficient improvement of the nasal airway.
Septal perforation.
Inadvertent changes to the appearance of the nose—particularly in the region of the supratip/dorsal septum. Infrequently “settling” can occur in this area, particularly with more involved manipulation of the caudal septum.
Anosmia (very rare).
SURGICAL TECHNIQUE
The patient is seen preoperatively in the holding area to review the goals of the operative procedure and the postoperative care and to verify elements of the physical examination that are best done in the awake patient such as nasal sidewall stability with inspiration. After consent is signed, the patient is instructed to use a nasal decongestant spray (e.g., oxymetazoline)—two sprays to each side of the nose, about 15 minutes prior to being taken back to the operating room.
Following the induction of general anesthesia, an oral RAE tube, secured down the midline, is used since the preformed contour allows it to sit easily and tension free in the midline. A standard endotracheal tube, on the other hand, is generally taped to one side or the other and can exert at least some pull on the nasal base and columella toward that side, which is felt to be counterproductive to the goal of establishing a centered nasal septum. A single dose of an intravenous antibiotic is given prior to making the incision.
I then once again use a nasal speculum to examine the nose to confirm the observations from the initial office consultation, and I palpate the caudal septum to reevaluate its strength, stability, and orientation.
Beginning posteriorly, I inject the nasal septum (and turbinates if reductions are planned) bilaterally with 1% lidocaine with 1:100,000 epinephrine. In order to benefit from the vasoconstrictive effect of the epinephrine, it is more important to widely distribute the local anesthetic through multiple points of injection than it is to concern oneself with attempting to forcefully distribute the local anesthesia via a single injection site at the caudal septum. The volume of the injection can also be used constructively to inflate or hydrodissect the septal mucosa from within deep grooves, angles, or crevices if present. Once the intranasal injections are completed, oxymetazoline-soaked pledgets are placed in each side of the nose. The operating table is then turned and the patient positioned appropriately for surgery and prepped and draped in a sterile fashion.
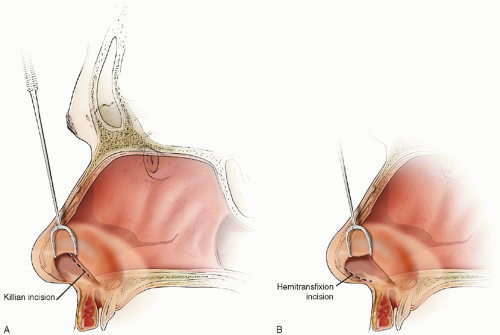
Through a hemitransfixion incision (Fig. 2.1) made at the free edge of the caudal septum, complete bilateral submucoperichondrial and submucoperiosteal flaps are elevated. As a right-handed surgeon, I prefer to start with a left hemitransfixion incision, but if the caudal septal edge is moderately or significantly displaced to the right side making it relatively inaccessible from the left, then a right-sided incision is made without hesitation. Flap elevation can be done using a Woodson, Freer, Cottle or suction elevator. I prefer to begin with a Woodson elevator (very sharp edges, very useful for getting into the proper plane of dissection and for teasing tethered mucosa from fracture lines or deep grooves), and I transition to a Cottle elevator further posteriorly in the nose when it becomes difficult to see over the curve of the spatulated end of the Woodson elevator.
Some surgeons prefer a Killian incision (an incision through septal mucoperichondrium parallel and 5 to 8 mm cephalic to the hemitransfixion incision just above the mucocutaneous junction) arguing that it preserves the mucosal attachments and blood supply to the caudal septum (Fig. 2.1). For septal deflections requiring any kind of manipulation or adjustment of the caudal septum, however, this access is limiting. More importantly, oftentimes subtle (but clinically relevant) abnormalities of the caudal septum are not fully apparent until complete exposure is achieved. By choosing to limit exposure of the caudal septum through a Killian incision, the surgeon risks leaving an unappreciated caudal septal deflection unaddressed. Furthermore, if one is planning on elevating complete flaps from both sides of the septum (which I do routinely), a hemitransfixion incision allows one to transition around the caudal edge of the septum with greater ease.
There are three reasons to routinely elevate bilateral mucoperichondrial flaps off of the septum as opposed to working through the elevation of one side only.
Exposure. If we are to aspire to maximizing success rates, no matter what the operation, all surgeons would agree that the operation in question is better done by optimizing the exposure. Achieving the best possible exposure of the surgical field is a fundamental principle of surgery. The septoplasty operation is no different. Why begin by compromising exposure? A better 3-D look at the septum from two sides will surely enhance one’s appreciation of what structural abnormalities are present within the nasal airway if for no other reason than by allowing the brain to interpret curves, angles, and shifts from two views. By enabling oneself to visually examine the underlying cartilaginous septum, the bony septum, and the position of the maxillary crest from both sides throughout the entire course of the operation, one can better identify, better diagnose, more easily adjust, and more accurately evaluate septal alignment and the effect of changes made.
Release. The position and configuration of the nasal septum are influenced by multiple intrinsic and extrinsic forces. Deformations, angulations, telescoped segments, curves, and spurs that are inherent to the septum itself would be thought of as “intrinsic” deforming forces. Forces extrinsic to the actual cartilage and bone of the septum that might affect the position of the septum include displaced nasal bones, collapsed or twisted upper lateral cartilages that attach to the dorsal septum, and the firmly adherent nasal mucoperichondrium and mucoperiosteum.
The nasal mucosal envelope is a very tightly bound sleeve that drapes from the floor of the nose, over the lateral aspect of the maxillary crest and along the septum to the roof of the nasal cavity before turning laterally to the nasal sidewall. There is little laxity to the mucosa, as evidenced by the difficulty encountered by the surgeon trying to mobilize mucosa to close even small septal perforations.
When the septal cartilage is displaced over the maxillary crest to one side, the mucosa of the opposite side follows the cartilage and is therefore tightly draped OVER the dorsal aspect of the crest—essentially occupying or preventing access to the midline space (Fig. 2.2). At its extreme, this is visualized as the deep groove one often sees over the crest on the side opposite the obstructed nasal airway. Completely elevating the mucosa from both sides of the septum, therefore, allows for maximal release of tension across the entirety of the septum and opens up the midline space completely (by coming right off the maxillary crest), thereby making it possible for the surgically corrected septum to move into that space. Consider the treatment of scar contractures—one of the fundamental principles of surgical management is scar release
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree