Secondary Intraocular Lens Implantation in Children: In-the-Bag and Ciliary Sulcus Fixation
Rupal H. Trivedi
M. Edward Wilson
The use of primary intraocular lenses (IOLs) for pediatric aphakia has become increasingly common in recent years and is now a well-accepted approach for children beyond infancy. Nevertheless, the implantation of an IOL at the time of cataract surgery in children during infancy remains controversial.1 The Infant Aphakia Treatment Study (IATS) was a multicenter randomized controlled trial comparing (1) primary IOL implantation (with glasses for residual hyperopia) with (2) primary aphakia with contact lens correction for unilateral cataracts operated from 1 through 7 months of age. In the report detailing the 1-year IATS results, the authors stated that caution should be exercised when performing IOL implantation in children aged 7 months or younger given the higher incidence of adverse events and the absence of an improved short-term visual outcome compared with contact lens use.1 Many of these aphakic eyes will later require secondary IOL implantation. Secondary implantation of an IOL is generally recommended when traditional spectacle or contact lens correction of aphakia is unsuccessful. In addition, many parents electively choose secondary IOL implantation for their aphakic children when eye growth slows after age 4 years. Silsoft contact lenses are well tolerated in very young children, but the material is less well tolerated as children get older. The silicone contact lenses develop more deposits and the lens coating breaks down more quickly when worn in older children. Rather than change to a nonsilicone contact lens material, some parents will opt to have a secondary IOL implanted at that point.
To the best of our knowledge, the first IOL implantation in a child was performed as a secondary implantation in 1952. Dr. Edward Epstein performed this secondary IOL implantation for a traumatic cataract in a 12-year-old girl. A cruciate needling was performed on a cataractous lens on April 2, 1952. The lens became hydrated, and much of the cortex was absorbed. On June 26, 1952, the residual cortex was washed out and a Ridley IOL was inserted. Forty-six years later, the best-corrected visual acuity was 20/20, and the IOL remained centered and optically clear (cited in Ref.2). While proceeding with secondary IOL implantation, surgeons face some important questions. Should I implant in this eye? If yes, what is the best site for fixation and what type of lens material should I use? This chapter reviews the literature on bag-fixated and sulcus-fixated secondary IOL implantation. In the absence of sufficient capsular support, anterior chamber, sutured, or iris-fixated IOL may be used (see Chapter 32).
AGE AT IMPLANTATION
In an article published by us in 2005, the average age at secondary implantation was 7.8 ± 5.0 years with median of 7.2 and range of 0.5 to 18.9 years (n = 77).3 We are now implanting secondary IOLs at relatively younger ages. Most commonly, secondary IOL implantation in our patients was performed between the ages of 2 and 4 years, a period when contact lens compliance can be difficult to achieve, and yet, there is still hope to reverse amblyopia. Due to the relatively slower growth of eyes after this age, IOL power calculations are also more predictable. Many of these children receive secondary IOL implantation before they enter school. Another smaller peak was observed in our group of patients who were 12 to 14 years of age. Most of these were bilaterally aphakic patients who requested IOL implantation for convenience (eliminating contact lens care) or for an improvement on the poor appearance and optical disadvantages of aphakic spectacles. Other series have noted mean ages of 8 years (range 2-16 years),4 10.3 years (1-22 years),5 7.4 years (1.1-15.4 years),6 and 2.1 years (1.5-2.5 years).7 If sufficient capsular support for bag or sulcus fixation is present,
we now offer secondary IOL implantation soon after we notice that contact lens/spectacle wear is becoming difficult or fails. However, when inadequate capsular support is present for sulcus fixation in a child, implantation of an IOL is not recommended unless every contact lens and spectacle option has been fully explored.
we now offer secondary IOL implantation soon after we notice that contact lens/spectacle wear is becoming difficult or fails. However, when inadequate capsular support is present for sulcus fixation in a child, implantation of an IOL is not recommended unless every contact lens and spectacle option has been fully explored.
EXAMINATION
A complete ophthalmic examination including visual acuity, slit-lamp biomicroscopy, and fundus examination after mydriasis should be performed. In children who do not permit a reliable office examination, an examination under anesthesia should be performed.
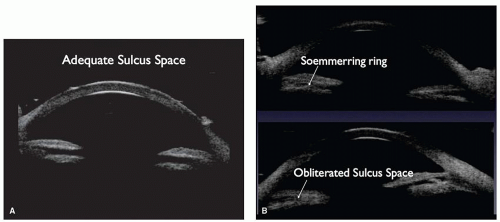
It is important to document central corneal thickness, horizontal corneal diameter, keratometry, globe axial length, intraocular pressure (IOP), and a thorough evaluation of the status of the optic nerve, macula, and retinal periphery. The shape and size of the pupil, any transillumination defects or damage to the iris, the presence of posterior synechia, any vitreous in the anterior chamber, and any other associated ocular anomalies should be documented. Ultrasound biomicroscopy (UBM) may help to detect residual capsular support and image the ciliary sulcus when viewing it directly is difficult (Fig. 31.1).
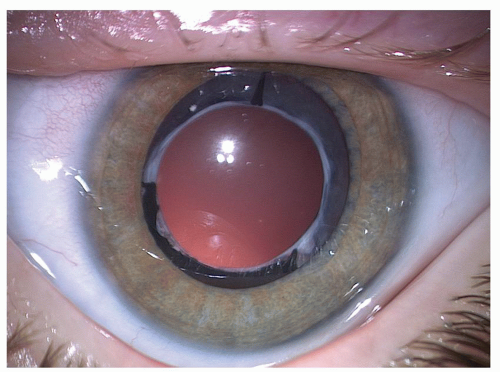
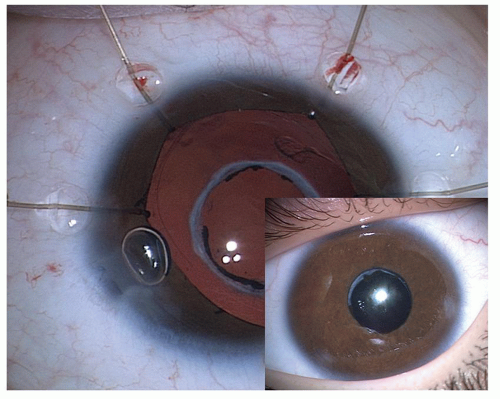
The technical success of secondary implantation depends mainly on how much capsular support was left behind at the time of primary cataract surgery (Fig. 31.2). Three hundred sixty-degree visibility of the fused edge of the posterior and anterior capsulectomy from the previous surgery increases the chances of achieving successful posterior segment implantation of an IOL. In the office, if the posterior capsule is not initially visible at the slit lamp, having the patient look in extremes of gaze while maintaining the slit-lamp chin position may allow capsular remnant to be seen under the iris. Sometimes, examination through a peripheral iridectomy (if present) is useful to look for capsular remnants. The presence of posterior synechia is evidence of at least some capsular support since adhesion between iris and capsule is what creates the synechia. There are times, however, when uncertainty about how much capsular support is present remains until surgery when a push-pull instrument or hook (Fig. 31.3) can be used to look directly under the iris in all quadrants.
SITE OF FIXATION
Most aphakic children have had a primary posterior capsulectomy and vitrectomy. It is rare to find an aphakic child with an intact posterior capsule. Aphakic children with residual capsule often have synechia between the anterior and posterior capsule. The surgeon has the option of placing an IOL in the ciliary sulcus after lysing iridocapsular adhesions or attempting capsular bag placement after reopening the capsular bag. If capsular support is available, the IOL should be placed in the posterior segment either in-the-bag or in the ciliary sulcus. The most desirable position for the IOL is within the reopened capsular bag. However, if the capsular leaflets are sealed to one another without reproliferated cortex (Soemmering ring), ciliary sulcus fixation is the better choice.8 The technique of in-the-bag secondary IOL implantation in children was reported in 1999 by one of us (MEW).9 Our updated experience with this technique was published in 2005 and 2011.3,10 Grewal and Basti11 reported a modification of the technique, where the authors suggested initiating a new anterior capsulectomy using a
cystitome to incise the anterior capsule close to its attachment to the posterior capsule. A pair of curved microscissors is used to cut circumferentially, completing the capsulectomy, and a dispersive ophthalmic viscosurgical device (OVD) is used to viscoexpress Soemmering ring material from the capsular bag. A two-handed maneuver was used to manually divide the Soemmering ring. Later, slow-motion phacoemulsification was used to emulsify and remove the pieces. Viscoexpression of the fragments of Soemmering ring was done. The residual capsular bag was filled with OVD, and a three-piece IOL was injected and dialed in. The authors concluded that this technique allows complete evacuation of Soemmering ring and placement of secondary IOL in the bag.11
cystitome to incise the anterior capsule close to its attachment to the posterior capsule. A pair of curved microscissors is used to cut circumferentially, completing the capsulectomy, and a dispersive ophthalmic viscosurgical device (OVD) is used to viscoexpress Soemmering ring material from the capsular bag. A two-handed maneuver was used to manually divide the Soemmering ring. Later, slow-motion phacoemulsification was used to emulsify and remove the pieces. Viscoexpression of the fragments of Soemmering ring was done. The residual capsular bag was filled with OVD, and a three-piece IOL was injected and dialed in. The authors concluded that this technique allows complete evacuation of Soemmering ring and placement of secondary IOL in the bag.11
In-the-bag fixation is more consistently achieved in eyes made primarily aphakic during early infancy. This age at surgery relates to the tendency for a more exuberant Soemmering ring formation in those operated in the first 6 months of life. The Soemmering ring lens cortex fills the capsular bag equator and prevents the anterior and posterior capsule remnants from sealing to one another and closing the capsular bag remnant. Removing the contents of the Soemmering ring and replacing them with OVD allows in-the-bag IOL placement to occur more predictably. An odds ratio analysis revealed that within our study group, eyes originally operated before 6 months of age were 8.7 times more likely to receive a secondary in-the-bag than those of patients who were rendered aphakic after the age of 6 months.3 In a subsequent study, we noticed that all of the eyes that received in-the-bag IOL insertion had a cataract extraction within the first 4 months of life.10 We hypothesized, as stated above, that young children have much more equatorial epithelial cell proliferation after surgery, even when cortical cleanup is felt to be complete. The few remaining lens epithelial cells are able to produce a dense ring of cortex that becomes trapped between the lens equator and fused anterior and posterior capsulectomy edges; a potential space for in-the-bag placement of an IOL is thus maintained.3 In eyes undergoing cataract surgery later in life, perhaps less dense Soemmering ring leads to fusion of anterior and posterior capsular leaflets. This scarred fibrous fusion may make the anterior and posterior capsule remnants inseparable, and the in-the-bag option may not be feasible.3 At times, these fused leaflets can be viscodissected apart, but attempting this degree of dissection can risk disruption of what would otherwise be a stable platform for ciliary sulcus IOL fixation.
Ciliary sulcus fixation is the best second alternative site for fixation of the IOL in the presence of available capsular support.3,5,8,9,10,12,13 Several case series have been reported, indicating that a lens placed in the ciliary sulcus is reasonably safe and effective over the short term. Awad et al.4




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree