Md. Shahid Alam
Dr. Md. Shahid Alam did his masters in Ophthalmology from the prestigious Aligarh Muslim University. He completed his long term fellowship training in Orbit and oculoplastics from Sankara Nethralaya. Presently he is working as an associate consultant in the department of orbit oculoplasty reconstructive and aesthetic services, Sankara Nethralaya, Chennai. His area of interest is orbital and adnexal oncology and ocular trauma.

Akshay Gopinathan Nair
Akshay Gopinathan Nair received his medical degree from Maharashtra University of Health Sciences, India and completed his residency training in ophthalmology from Sankara Nethralaya in Chennai, India. Following this, he underwent fellowship training in ophthalmic plastic surgery, ocular oncology and facial aesthetics at L V Prasad Eye Institute, Hyderabad, India and New York Eye & Ear Infirmary of Mount Sinai, USA. Dr. Nair has over 50 peer-reviewed publications, 8 book chapters in ophthalmology. His areas of special interest are ocular surface and eyelid tumours, ophthalmic imaging and neuroimaging. Dr. Nair is a faculty member at Lokmanya Tilak Municipal Medical College, Mumbai, India and is also affiliated with Advanced Eye Hospital & Institute and Aditya Jyot Eye Hospital in Mumbai.

Bipasha Mukherjee
Dr. Bipasha Mukherjee is a fellow in Orbit & Oculoplasty from Aravind Eye Hospitals, India, and ICO fellow from University Hospital of Limoges, France, under Prof. Jean-Paul Adenis. She has undergone clinical observerships with stalwarts like Jack Rootman, Richard Collins, Geoff Rose, Mark Duffy, and Robert Goldberg.
She currently heads the department of Orbit, Oculoplasty, Aesthetic & Reconstructive services in Medical Research Foundation, Chennai. She has numerous presentations in national and international conferences and publications in peer-reviewed journals and text books. Her areas of interest include diseases of the orbit and adnexa including tumors, lacrimal surgery, socket reconstruction, traumatic lid and adnexal injuries, training residents and fellows, and photography.
Introduction
Sebaceous gland carcinoma (SGC), sebaceous cell carcinoma, and meibomian gland carcinoma are all terms used in the literature to describe a malignant neoplasm of sebaceous origin, commonly found in the eyelids and adnexa [1]. It was first described as a malignant ocular entity of the ocular adnexa as early as the nineteenth century [2]. Straatsma presented the first series of 16 patients with sebaceous carcinoma in 1956 [3]. The tumor is notorious, for mimicking various benign and malignant clinical entities and for its aggressive local behavior and the potential to metastasize regionally to lymph nodes and to distant organs.
Origin
The most common location for SGC is within the meibomian glands of the upper eyelids followed by the lower eyelids [2]. The upper eyelid is involved more frequently because of more number of meibomian glands. It can also arise from the gland of Zeis and the sebaceous glands associated with the caruncle.
Incidence and Demographics
Sebaceous gland carcinoma accounts for almost 5 % of all eyelid malignancies in the United States [1]. A higher incidence has been reported in Asian and Indian population [1, 4]. Ni and associates reported that sebaceous carcinoma accounted for 33 % of all malignant eyelid tumors in China [5].
Sebaceous carcinoma occurs more commonly in females than males, and the average age of detection is between 60 and 69 years. There is a second younger age of incidence in children who develop sebaceous carcinoma as a secondary cancer after radiation for bilateral inherited retinoblastoma [6].
Risk factors: the following are some of the risk factors for the development of sebaceous gland carcinoma of the ocular adnexa:
- (a)
Irradiation: There are reports of cases of sebaceous gland carcinoma occurring in patients who received radiotherapy for retinoblastoma in the past. A review of nine such cases revealed that all cases were hereditary, and sebaceous carcinoma occurred after a mean duration of 11 years of exposure [7].
- (b)
Human papillomavirus (HPV) infection: HPV infection and integration of DNA have been implicated in many cancers including sebaceous gland carcinoma. Hayashi et al. found HPV infection in 61.9 % of sebaceous carcinoma specimens [8].
- (c)
Immunosuppression: Like many other malignancies, immunosuppression is a risk factor for development of sebaceous gland carcinoma too. In patients infected with HIV, the tumor occurs at a younger age and is more aggressive. There is a report of sebaceous carcinoma occurring in two patients infected with HIV. Both the patients were in their 30s and developed aggressive tumor over 6–9 months of duration, requiring exenteration in one of them [9]. Autoimmune diseases also represent a suppressed immune system. There is a report of a case of multiple scalp sebaceous adenomas and solitary sebaceous carcinoma occurring in a patient of multiple sclerosis [10].
- (d)
Muir-Torre syndrome: There are occasional reports of patients with Muir-Torre syndrome developing periocular sebaceous carcinoma [11].
- (e)
Diuretics: A relationship between the use of thiazide diuretics and sebaceous carcinoma has been postulated in a report of 20 cases [12]. However, there is no firm evidence of relationship between the two.
Clinical Features
Sebaceous gland carcinoma most commonly presents as a solitary painless nodule, arising from the meibomian glands of the upper eyelid followed by that of the lower eyelid [1, 13] (Fig. 45.1). Since the epidermis of the eyelid skin is not involved in the initial stages, there are chances of misdiagnosing as a chalazion. As the tumor starts invading the epidermis, it gives a yellow cast because of the lipid deposition. It also begins to disrupt the lid architecture and leads to loss of eyelashes which can be seen even in the earlier stages in a mass arising from the glands of Zeis [14]. Other suspicious signs include telangiectasia, ulceration, and bleeding (Fig. 45.2).



Fig. 45.1
Sebaceous gland carcinoma (SGC) of the lower lid presenting as a lid nodule, which on eversion showed an irregular, elevated mass

Fig. 45.2
SGC presenting as a yellowish, nodular mass arising from the lower eyelid with surface ulceration
The second most frequent presentation is a diffuse unilateral thickening of the eyelid [1]. This variant can spread intraepithelially (pagetoid spread) into the fornices and the bulbar conjunctiva. It is often misdiagnosed as blepharitis or blepharoconjunctivitis. Any middle-aged or elderly patient presenting with long-standing unilateral blepharitis or blepharoconjunctivitis not responding to standard treatment is a candidate for lid biopsy. This intraepithelial (pagetoid) invasion of the overlying conjunctival epithelium has been reported in up to 40–80 % of cases of SGC [15] (Fig. 45.3).


Fig. 45.3
SGC with pagetoid spread: note the diffuse epithelial involvement over the ocular surface
Rarely, SGC can present as a pedunculated lesion, just like a cutaneous horn [16] (Fig. 45.4). In neglected cases, sebaceous gland carcinoma can involve the orbital structures, eyelids, and conjunctiva and rarely can also mimic a lacrimal gland mass (Fig. 45.5).

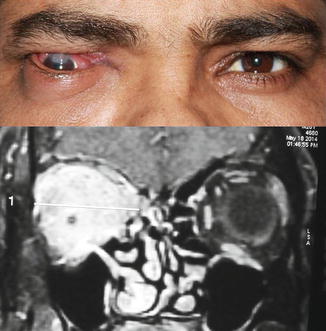

Fig. 45.4
SGC of the upper lid presenting as a cutaneous horn with ulceration at the tip
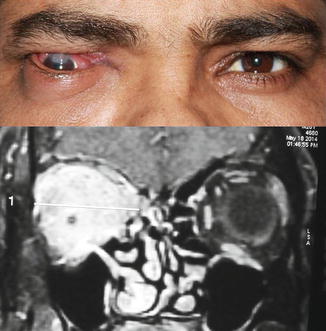
Fig. 45.5
SGC of the right eyelid with orbital invasion presented with proptosis and restricted ocular motility. An MRI (below) shows the orbital component of the tumor as a hyperintense mass lesion
Differential Diagnosis [1]
- 1.
Basal cell carcinoma, squamous cell carcinoma, sweat gland tumors, and pilomatrixoma
- 2.
Eyelid lymphomas
- 3.



