Purpose
To report the surgical outcome of “sealing the gap” in treating symblepharon caused by various etiologies other than recurrent pterygium.
Design
Retrospective, interventional case series.
Methods
Sixteen eyes of 14 patients with pathogenic symblepharon were consecutively operated by conjunctival recession, sealing the gap between recessed conjunctiva and Tenon capsule with a running 9-0 nylon suture, and covering of the bare sclera with amniotic membrane. For severe symblepharon where there was conjunctival shortening, oral mucosa graft was added. Outcome measures include ocular surface inflammation, fornix reformation, and restoration of ocular motility.
Results
The underlying causes of symblepharon included Stevens-Johnson syndrome (n = 6), chemical burn (n = 5), ocular cicatricial pemphigoid (n = 1), thermal burn (n = 1), following excision of conjunctival squamous cell carcinoma (n = 1), conjunctival scarring following exposed buckle (n = 1), and immune dysregulation (n = 1). Twelve eyes (75%) had an average of 1.6 ± 0.9 previous surgeries. Before surgery, ocular motility restriction was significantly correlated with the severity of symblepharon. During the follow-up period of 17.1 ± 13.6 months, 13 eyes (81.3%) achieved complete success, 2 eyes (12.5%) achieved partial success, and 1 eye with immune dysregulation had failure (6.3%). There was no correlation between the success rate and the severity of symblepharon. After surgery, the ocular motility and inflammation were significantly improved. Visual acuity had improved in 2 of 15 eyes.
Conclusions
Sealing the gap between the conjunctiva and Tenon capsule is an important step in the surgical management of pathogenic symblepharon. This method not only avoids the use of mitomycin C, but also creates a strong barrier to prevent recurrence, restore ocular surface integrity, reform a deep fornix, and regain full ocular motility.
Symblepharon refers to any adhesion between the palpebral and bulbar conjunctiva that develops following diverse etiologies such as trauma, chemical injuries, infections, and immune dysregulation. The pathogenic effects of symblepharon depend on its location and severity. In general, mild symblepharon located near the lacrimal gland orifices may cause blockage and lead to dry eye, while that located at the inferior fornix may obliterate the tear reservoir and interfere with effective replenishment of tears in the meniscus and the ocular surface. In severe cases, symblepharon may cause inadequate blinking, lagophthalmos, and ocular motility restriction.
No treatment is necessary if symblepharon does not carry the aforementioned pathogenic elements. However, patients with pathogenic symblepharon, as defined above, should be treated to avoid sight-threatening corneal complications as a result of cumulative insults and chronic inflammation. A variety of surgical approaches have been reported for the treatment of symblepharon. Tissue substitutes such as conjunctiva, oral mucosa graft, or amniotic membrane were used for ocular surface reconstruction after symblepharon lysis. Anchoring sutures were also useful to secure the released conjunctiva deep into the fornix. Various materials have been evaluated to keep the potentially adhesive surfaces apart after surgery and to reduce recurrences such as symblepharon ring, silicone sheet implant, nylon foil–anchored polytetrafluoroetyhlene (Gore-Tex), mitomycin C (MMC), bevacizumab, or postoperative application of β-irradiation. Despite all these efforts, the recurrence rates remained highly variable from 6.2% to 40% ( Table 1 ).
| Source | Technique | Eyes (N) | Underlying Cause | Symblepharon Severity | Mean (SD) Follow-up (mo) | Minimal Follow-up (mo) | Recurrence Rate |
|---|---|---|---|---|---|---|---|
| Tseng 1997 | AMT | 5 | OCP (n = 2), TB (n = 1), RP (n = 1), TEN (n = 1) | 14.54 | 5.5 | 40% | |
| Patel 2012 | AMT | 10 | 6 | 20% | |||
| Katircioglu 2003 | AMT + AS | 6 | Alkali burn | Severe (n = 3), moderate (n = 2), mild (n = 1) | 10 | 4 | 16.67% |
| Solomon 2003 | AMT + AS | 17 | Autoimmune disorders (n = 9), after ocular surgery (n = 4), after ocular trauma (n = 4) | One location (n = 11), 2 locations (n = 5), 3 locations (n = 1) | 37 | 9 | 17.65% |
| Jain 2004 | AMT + AS | 20 | RP (n = 5), acid burns (n = 1), alkali burns (n = 5), SJS (n = 4), TB (n = 3), and congenital symblepharon (n = 2) | Stage II or III | 12 | 12 | 40% |
| Tseng 2005 | MMC + AMT + AS | 18 | CB/TB (n = 7), RP (n = 5), SJS (4 eyes), OCP (n = 2) | One location (n = 6), 2 locations (n = 12) | 14.16 | 6 | 18.75% |
| Kheirkhah 2008 | MMC + CAU/OMG + AMT + AS | 61 | SJS (n = 26), CB (n = 19), chronic cicatricial conjunctivitis of unknown cause (n = 9), RP (n = 3), MMP (n = 2), pseudopemphigoid (n = 1), lid sebaceous carcinoma (n = 1) | Grade I (n = 17), grade II (n = 26), grade III (n = 9), grade IV (n = 9) | 25 | 12 | 14.8% |
| Kheirkhah 2013 | MMC + OMG + AMT + AS | 32 | CB (n =16), TB (n = 7), SJS (n = 5), OCP (n = 2), xeroderma pigmentosum (n = 1), graft-vs-host disease (n = 1) | Grade III (n = 19), grade IV (n = 13) | 16.4 | 6 | 6.2% |
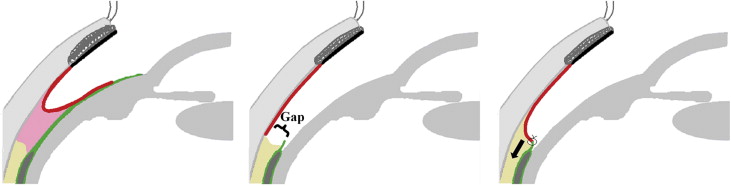
For managing symblepharon caused by multi-recurrent pterygia, we have recently reported a significant improvement of the surgical outcome in restoring caruncle morphology and full ocular motility by adding an extra step termed “sealing the gap,” with or without conjunctival autograft or oral mucosa graft, which is added for eyes with a severe shortage of remaining conjunctival tissue, measured from the tip of the symblepharon to the remaining caruncle. This technique can be achieved by anchoring sutures as mentioned above or by a running 9-O nylon suture. Herein, we reported our clinical experience in adding this extra step, “sealing the gap,” using such a running suture ( Figure 1 ) to manage symblepharon caused by various etiologies other than recurrent pterygia.
Methods
This retrospective interventional case series study was approved by the Institutional Review Board of Baptist Hospital of Miami/South Miami Hospital Inc, Miami, Florida. A total of 16 eyes of 14 patients who underwent surgical correction of symblepharon with the technique of “sealing the gap” from July 19th, 2010 through February 27th, 2015 were included in this study. Before surgery, possible advantages and disadvantages of the procedures were explained fully to the patients and their written informed consents were obtained. The advantages and disadvantages of the off-label use of fibrin glue in ophthalmology were also discussed. Demographic information, clinical presentation, prior surgeries, and outcomes are summarized in Table 2 .
| Eye No. | Sex | Age (y) | Underlying Cause | Prior Surgery, No. | Grading | OMG a | Outcome | Postoperative Inflammation | Visual Acuity | Ocular Motility Restriction | Follow-up (mo) | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pre | Post | Pre | Post | ||||||||||
| 1 | F | 57 | Chronic cicatricial conjunctivitis | SL + MMC + AS, 1 | I a 1+ | − | CS | 0 | 20/20 | 20/20 | 0 | 0 | 6 |
| 2 | M | 41 | Conjunctival scar | AMT, 3 | I a 2+ | − | CS | 0 | 20/25 | 20/25 | 0 | 0 | 19 |
| 3 | F | 21 | SJS | LR, 1 | II a 1+ | − | CS | 1+ | CF | CF | 0 | 0 | 8 |
| 4 | F | 44 | SJS | AMT,1 AMT + OMG, 1 LR, 1 | II a 1+ | − | CS | 0 | HM | HM | 0 | 0 | 33 |
| 5 | F | 23 | SJS | AMT, 1 | II c 0 | − | CS | 1+ | HM | HM | 0 | 0 | 45 |
| 6 | M | 75 | CB | KLAL,1 | II c 0 | − | CS | 0 | HM | HM | 0 | 0 | 7 |
| 7 | M | 72 | CB | CAU + AMT, 1 | III a 0 | + | CS | 0 | CF | CF | 0 | 0 | 7 |
| 8 | F | 15 | CB | LR, 1 | III a 3+ | − | CS | 0 | CF | 20/400 | 0 | 0 | 9 |
| 9 | F | 23 | SJS | AMT, 1 | III c 1+ | − | F | 1+ | 20/30 | 20/30 | 0 | 0 | 45 |
| 10 | F | 2 | TB | AMT, 1 SL + AMT + AS,1 | III c 0 | + | CS | 0 | Not checked | Not checked | 2− | 0 | 18 |
| 11 | F | 83 | OCP | LR, 1 | III c 1+ | − | CS | 0 | HM | HM | 2− | 0 | 4 |
| 12 | M | 55 | SJS | III c 1+ | − | CS | 0 | HM | HM | 1− | 0 | 11 | |
| 13 | M | 55 | SJS | III c 1+ | − | PS | 0 | HM | HM | 2− | 0 | 9 | |
| 14 | F | 74 | Conjunctival tumor | Excision of tumor + SL, 2 CAU + AMT, 1 | III c 1+ | − | CS | 1+ | 20/30 | 20/30 | 2− | 0 | 6 |
| 15 | M | 49 | CB | IV b 0 | + | CS | 0 | 20/30 | 20/20 | 3− | 0 | 24 | |
| 16 | F | 51 | CB | IV c 2+ | + | PS | 1+ | CF | CF | 3− | 0 | 22 | |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


