Rosacea
Sonia H. Yoo
Andre C. Romano
Rosacea is a chronic, idiopathic, inflammatory disorder affecting both the facial skin and the eye. The cutaneous manifestations include flushing, telangiectasia, and papules or pustules. The lesions are distributed in the flush areas (cheeks, forehead, nose, chin, and the upper chest). The typical facial feature of advanced rosacea is rhinophyma, or bulbous nose appearance caused by sebaceous gland hypertrophy.
Ocular involvement is less easily recognized than the skin changes seen in rosacea and often remains undiagnosed despite potentially serious sequelae. The most common symptoms of ocular rosacea are nonspecific and include a foreign body, gritty, or dry sensation, or burning, tearing, or redness (1). Ocular signs range from lid margin telangiectasia, meibomian gland dysfunction, and blepharoconjunctivitis, to vision-impairing corneal involvement such as neovascularization, thinning, and, in rare instances, perforation.
Cutaneous rosacea primarily affects adults between the ages of 40 and 50 years, but can also occur during childhood (2,3). It is reported to involve women twice as often as men (4), but cases with ocular manifestations are about evenly divided between the sexes, or show only a small female preponderance (5). Although there is a widespread clinical impression that rosacea affects fair-skinned people of northern European heritage, rosacea affects people of all races.
CLINICAL FEATURES
Dermatologic Findings
Flushing, telangiectasia, papules or pustules, and a later stage of sebaceous gland hypertrophy characterize skin involvement in rosacea. The lesions are distributed across the cheeks, forehead, nose, chin, and the upper chest. Initially, the hyperemia may be episodic and can be triggered by hot beverages, tobacco, alcohol, spicy foods, and emotional stress. Various mediators including substance P, histamine, serotonin, and prostaglandins have been implicated in this mechanism (6,7). The chronicity of this stage leads to dilation of small vessels and lymphatics (telangiectasia), followed by asymptomatic papular, and, less frequently, pustular lesions resembling acne vulgaris. Rosacea is distinguished from acne vulgaris by the absence of comedones, by its confinement to flush areas, and by older age than those affected by acne vulgaris. In addition, hypertrophic changes seen in rosacea are not features of acne vulgaris. Rhinophyma, or bulbous nose, is the last stage of the disease, and is due to slowly progressive sebaceous gland hypertrophy (Fig. 34-1).
Ophthalmic Findings
The incidence of ocular involvement in rosacea varies widely from 3% to 58% in the literature (8,9). We believe that it is underappreciated and underreported because of mild cases going undiagnosed. The most frequent manifestations are meibomian gland dysfunction, telangiectasia of the lid margin, conjunctival hyperemia, and blepharoconjunctivitis.
Meibomian gland dysfunction may progress to obstructed gland orifices and lead to an irregular, hyperemic, thickened and telangiectatic lid margin (Fig. 34-2). Finally, hyperkeratinization of the ducts may displace glands posteriorly and make them less visible than in healthy subjects. The consequence is a quantitatively and qualitatively poor tear film.
Lemp et al. (10) reported that 36.7% of 60 rosacea patients had subnormal tear production compared to only 4.2% of 120 controls using Schirmer’s test without anesthesia.
The altered lipid layer of the precorneal tear film leads to a rapid tear breakup time producing dry spots. These are demonstrated best with rose bengal or fluorescein staining, especially in the interpalpebral fissure where punctate keratitis may be seen (Fig. 34-3). The loss of the stabilizing effect on the tear film accounts for the most common complaints of ocular rosacea, which are burning, tearing, and foreign-body sensation.
Other frequent signs that affect the eyelids include chalasia and hordeolum. Posterior or internal hordeola often represent infection or inflammation in a meibomian gland. Fifty-seven percent of patients scheduled for excision of chalazia over 19 years of age and 64% of patients over the age of 29 were found to have rosacea (11).
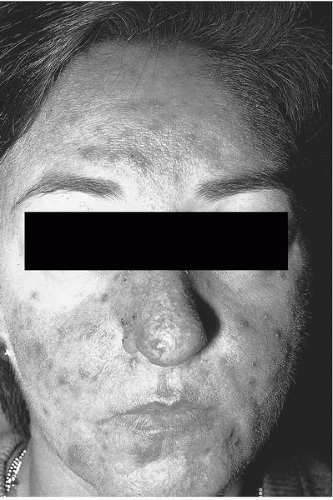 FIGURE 34-1. Rosacea dermatitis. Note the typical features of facial rosacea which include (1) facial erythema, (2) papules and pustules, and (3) rhinophyma.(see color image) |
Two types of conjunctivitis are associated with rosacea: diffuse hyperemia and a nodular conjunctivitis. In the diffuse form of conjunctivitis, the vessels of the tarsal and bulbar conjunctiva are engorged. A scant, watery secretion is usually found; a mucopurulent discharge suggests a superimposed bacterial conjunctivitis. The nodular conjunctivitis is much less common. Small, gray, highly vascularized nodules appear on the bulbar conjunctiva, especially near the limbus in the interpalpebral area. These phlyctenular lesions appear quickly, undergo superficial ulceration, and then disappear quickly. Fibrosis is the most serious conjunctival complication. It can lead to fornix foreshortening and symblepharon formation, can cause corneal complications, and can produce confusion by suggesting the possibility of ocular cicatricial pemphigoid (1).
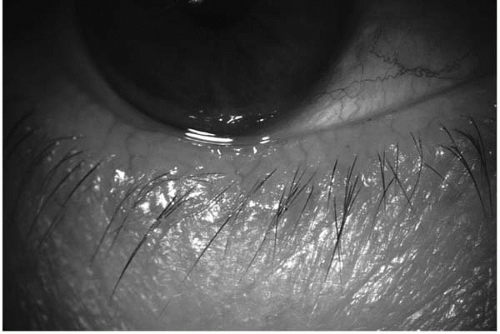 FIGURE 34-2. Thickened, hyperemic, telangiectatic lid margin.(see color image) |
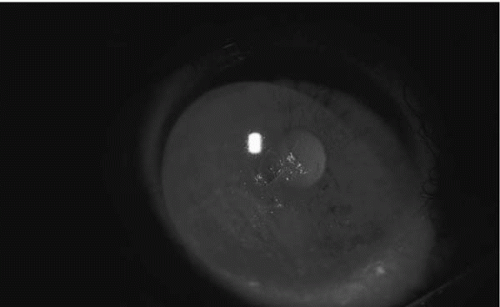 FIGURE 34-3. Superficial punctate keratitis and epithelial irregularity secondary to unstable tear film in rosacea. Sodium fluorescein dye helps to visualize punctate staining. |
Corneal changes in rosacea result from the combination of lid and conjunctival disease. The initial manifestation is a marginal vascular infiltration (12). Dilated vessels at the limbus advance into the superficial cornea predominantly inferiorly, which may be accompanied by punctate keratitis.
Subepithelial infiltrates are a more severe manifestation of rosacea keratitis (12). Small, round or oval, sharply delineated infiltrates may be seen near the limbus, and may appear larger toward the center of the cornea, mainly in the lower half. These infiltrates are highly vascularized with a spade- or wedge-shape (Fig. 34-4). Inflammatory episodes may lead to infiltrations of the deeper stroma, ulceration, thinning or, rarely, perforation (1,13). Scleritis, episcleritis,
and conjunctival granulomas are less common findings in ocular rosacea (13).
and conjunctival granulomas are less common findings in ocular rosacea (13).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


