92 Robots in ENT/Head and Neck Surgery
92.1 Introduction
Transoral robotic surgery (TORS) was initially conceived for oropharyngeal cancer. The traditional treatment for this primary site, until the turn of the millennium, had been open surgery. The emergence of transoral laser microsurgery (TLM) offered the prospect of a surgical procedure with less morbidity. Publication of several reports of good oncological control with TLM combined with low morbidity led to interest in primary surgery for this site being rejuvenated. While TLM has shown undoubted oncological efficacy in this setting, most of work on TLM primarily pertained to tumours of the tonsil. Because of difficulties with resecting cancers of the tongue base via an endoscope, a microscope and coaxially mounted laser, the tongue base continued to be an orphan site with very few reports presenting data on TLM outcomes for this sub-site. Even for tonsil cancers, surgeons and multi-disciplinary teams were slow to adopt TLM for several reasons. The technique is difficult to teach which resulted in a shallow learning curve. TLM involves cutting through the tumour to identify its depth, with further sampling of the defect to confirm clear margins; thus, pathological margin assessment of the transected specimen was beset with controversies and frequently resulted in patients receiving double or triple modality treatment.
The manoeuvrability and optics of robotic systems, the prospect of en bloc resection and rapid adoption of robotic technology at other primary sites were attractive to head and neck surgeons. TORS offered the optimal balance of transoral access with limited morbidity, en bloc resection and a more rapid learning curve.
This chapter will address the rationale and evidence base supporting TORS for primary and recurrent cancers of the head and neck, and the emerging role of TORS in the investigation of the unknown primary tumour. This chapter will also briefly discuss the trials that are ongoing currently in this field.
92.2 Rationale for Incorporating TORS into the Treatment of Oropharyngeal Malignancies
92.2.1 HPV-Related Squamous Cell Cancers
The rising incidence of human papillomavirus (HPV)-related squamous cell carcinoma (SCC) at this primary site has been a key driving force in transoral surgery for oropharyngeal cancer. Affecting a relatively younger patient group, HPV-related SCC responds well to treatment; thus, survivorship issues become important. It is well recognised that radical doses of chemo-radiotherapy (CRT) used to treat head and neck cancer (with the aim of organ preservation) cause significant morbidity for patients in the short and long term. In patients receiving CRT, top complaints at various time points are consistently xerostomia and dysphagia, both seen after CRT. In a meta-analysis of 230 patients included in three large trials (RTOG 91–11, RTOG 97–03 and RTOG 99–14), 43% of patients were found to still be experiencing grade 3 or higher toxicity in the long term. Prospective observational studies suggest that both the above side effects can be reduced or avoided with a primary TORS approach. In a systematic review involving 20 case series, including eight intensity-modulated radiotherapy (IMRT) studies (1,287 patients) and 12 TORS studies (772 patients), while the oncological outcomes were comparable, the adverse events profile was different: oesophageal stenosis (4.8%) and osteoradionecrosis (2.6%) for IMRT, haemorrhage (2.4%) and fistula (2.5%) for TORS. Incorporation of TORS into the treatment strategy allows clinicians to tailor adjuvant therapy in patients who would otherwise receive standard CRT.
92.2.2 Non–HPV-Related Squamous Cell Cancers
These cancers typically have a worse prognosis than HPV-positive SCC. All available level 1 evidence for this group of patients supports non-surgical treatment. The French 94–01 phase III multi-centre randomised trial recruited 226 patients, comparing radiotherapy alone with radiotherapy and concomitant chemotherapy. Although explicit HPV testing was not done, the patient cohort with large primary sites and small nodal disease is indicative of HPV-negative tumours. They posted 5-year overall survival (22.4 vs. 15.8% [ρ = 0.05]) and locoregional control (47.6 vs. 24.7% [ρ = 0.002]) favouring the latter arm. Several prospective datasets where HPV-negative cancers have been treated by TORS and adjuvant radiation indicate high control rates, from 80 to 94%. However, selection bias in these studies is inevitable. As discussed above, the morbidity and mortality rates attributed to open surgery do not apply to surgical practices in the current day, and especially to transoral surgery; data on 30-day mortality from the U.K. national head and neck database indicate a mortality of less than 1%. For these reasons, more multi-disciplinary teams (MDTs) are in favour of incorporating a transoral resection for these tumours where feasible.
92.3 Non-Squamous Cancers
Minor salivary gland tumours are the most common non-squamous cancers seen in this anatomical site. The primary management is surgery. Following careful assessment, if access is found to be optimal, as is often the case with these tumours, transoral resection with or without adjuvant radiation offers equivalent control rates with less disruption of anatomy, and thus quicker recovery.
92.4 Robotic Technology
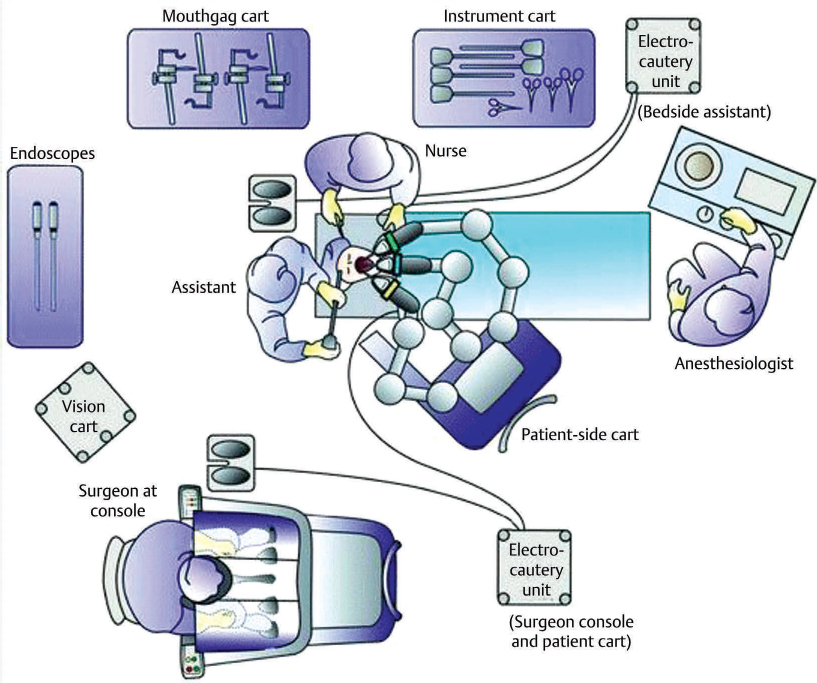
Although several robotic systems are currently available, the most commonly used system is the da Vinci, marketed by Intuitive, and will be described in this chapter. TORS represents a stepwise evolution in transoral surgery, the foundations for which have been laid by TLM. However, unlike TLM, tumours need not be in the ‘line of sight’ of the surgeon, a desirable attribute when resecting tumours of the base of tongue, supraglottis or hypopharynx. The hardware in the da Vinci system allows telescopes to achieve excellent three-dimensional visualisation of patient and tumour anatomy, and operating instruments to be controlled remotely within this visual field with excellent manoeuvrability. Robotic surgery with the Intuitive system is performed via a patient side cart comprising of the telescope and two (of the three available) robotic arms mounted on a mobile platform, which are docked into the patient’s mouth. The operator remotely controls these three instruments from a surgeon console across the operating room ( Fig. 92.1); the robot eliminates tremor and allows hand movements in 7 degrees of freedom which would be impossible with the human wrist.
Fig. 92.1); the robot eliminates tremor and allows hand movements in 7 degrees of freedom which would be impossible with the human wrist.
92.5 Theatre Setup for TORS
An examination under anaesthetic is performed at a separate sitting to assess the size, extent and resectability of the primary tumour. For the robotic resection, patients are positioned supine and mouth opening is maintained with an appropriate retractor, the choice depending on the site of tumour. Two commonly used retractors include the Boyle Davis or Feyh–Kastenbauer retractor; the latter has been extensively modified to incorporate a range of concave tongue blades that increase the intra-oral space and it possesses a larger frame that allows easier intra-oral docking of the robotic arms with less instrument clashes. The patients’ face and eyes are appropriately protected to avoid accidental injury. The operating telescope is inserted into the patients’ mouth and two instruments (at least one of which is an energy device to cut tissues and the other a grasper to retract tissues) are positioned either side of this ( Fig. 92.2).
Fig. 92.2).
An assistant at the head of the patient helps with smoke evacuation, suction, application of ligatures and retraction. This allows four independently controlled instruments to be used simultaneously in the intra-oral environment, providing unparalleled manoeuvrability.
92.6 TORS for Oropharynx and Supraglottic Cancers
Tonsil cancer The principle of TORS surgery is en bloc resection with a clear margin. The foundations for en bloc resection of tonsil cancers via a transoral route had been laid back in the 1950s when P. C. Huet described this procedure. This involved transoral resection of the tonsil and the superior constrictor muscle deep to the para pharyngeal space. TORS radical tonsillectomy is one of the first procedures that is undertaken by surgeons in the early stages of their TORS practice. The first report of TORS radical tonsillectomy was published in 2007 in a cohort of 27 adult patients with tonsil tumours staged T1 to T3, with a negative margin of 93%, 0% mortality and an acceptable complication rate of 4% gastrostomy-dependent at 6 months. A global multi-institutional study that collated outcomes for 410 patients from 11 centres demonstrated 2-year locoregional control rates of 91.8% and disease-free survival of 91%. TORS is currently used and approved by the Food and Drug Administration (FDA) for T1 and T2 cancers in the United States.