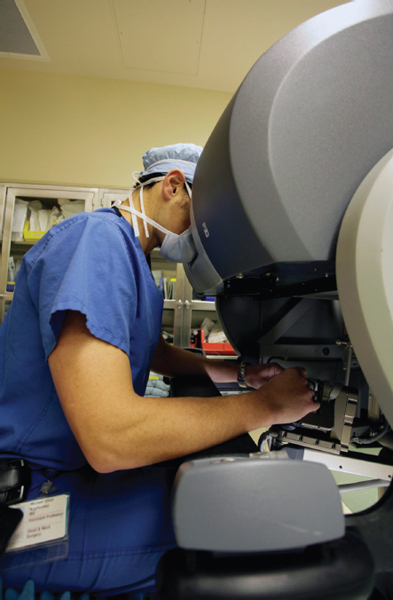
36 Robotics in Endoscopic Skull Base Surgery The coining of the term “robot” is attributed to the Czechoslovakian Joseph Capek who lent it to his brother Karel Capek for use in a play Rossum’s Universal Robots in 1920. The term was used to describe automated nonhuman laborers and is derived from the Czech word for “forced labor”—robota. Since that time the idea of automated machines designed to perform tasks has transformed from fiction to reality. The current definition of robot is as follows: a machine capable of carrying out a complex series of actions automatically, especially one programmable by a computer. Robotic surgery may be further defined as active, semiactive, or passive. Active robotics implies that the robot performs a programmed task independent of a human operator, but semiactive robotics require an operator input at certain set points to carry out an automated action. In passive robotics, the robot functions only at the specific direction of human action. In medicine, the use of robots has evolved dramatically over the past two decades, from machines designed to help precisely hold and guide instruments to advanced physician-controlled telerobotic devices that allow surgeons to perform complex endoscopic surgery from local or remote locations (even across oceans).1,2 The da Vinci surgical system (Intuitive Surgical Inc., Sunnyvale, California, United States) is currently the only commercially available surgical robot in the United States. The system consists of the patient-side cart with three or four arms (Fig. 36.1). One arm holds the endoscope and other arms hold instruments for surgical manipulation, including cutting, suturing, cautery, clip application, and grasping. Lasers are also often attached to a grasper for laser surgery. The endoscope consists of dual-mounted right and left high-definition telescopes, which project images to the viewing port for the respective eye on the surgical console. This produces a three-dimensional view with pristine clarity and allows for precision dissection in a microscopic environment. The surgical arms are equipped with EndoWrist technology, which provides 7 degrees of freedom and mimics the movement of the human wrist (traditional endoscopic surgery only allows 4 degrees of freedom). The patient-side cart is controlled by a surgeon from a separate console (Fig. 36.2). While viewing the field through the three-dimensional projection system the surgeon may articulate the arms and adjust the endoscopic view using the control handles. The computer tracks the surgeon’s movements and filters out tremors. In addition, an assistant should be available at the operative table to adjust the instruments, clean the endoscope, and occasionally to provide additional suction and cautery. The leading uses for surgical robotics at this time are in the disciplines of urology, gynecologic surgery, and cardiothoracic surgery, yet there has been a surge of interest in this technology in the field of otolaryngology, which shares similar concerns about limited surgical access in areas of vital structures.3,4 Figure 36.1 The surgical robot seen docked during a transoral robotic surgery. The use of surgical robotics in otorhinolaryngology began with simple automated drill guides used to precisely drill out the stapes footplate.5 Coinciding advances in technology and interest in minimally invasive surgery fueled the study of the surgeon-operated robot for further indications in the head and neck. Success in studies in porcine, mannequin, and cadaver models led to a variety of applications in live patients for surgery of the upper airway and neck.2,3,6–9 Although not completely abated, initial concerns about operative time, complications, and cost have been dampened as reports of great outcomes have led to surgical robotics being, in some centers, relatively commonplace for a myriad of otolaryngologic indications. Figure 36.2 The surgeon console for the robot system. As endoscopic minimally invasive head and neck surgery has evolved around the common natural routes of exposure, the most rapidly advancing discipline has been transoral robotic surgery (TORS) for carcinoma of the upper airway. TORS provides the unique advantage of visualization and precise instrumentation in difficult-to-access areas without large external incisions, and applications now include resections of carcinoma in the oral cavity, oropharynx, supraglottis, glottis, and hypopharynx.3,10–14 Long-term results are yet to be reported, and TORS has not been compared with other treatment strategies in any randomized controlled trials. However, the mounting literatures on the feasibility, oncologic, and functional outcomes are very encouraging.3,11–16 The use of the surgical robot for minimally invasive head and neck surgery has also extended beyond the transoral route and includes neck surgery for thyroid gland resection and neck dissection.2 One of the least studied but most fertile areas for study and application of surgical robotics in the head and neck is for minimally invasive skull base surgery. The following sections will provide a discussion of the current studied applications of robotics at the skull base, advantages and disadvantages compared with more traditional minimally invasive surgery, and some of the authors’ experiences. The most direct route for endoscopic skull base surgery is via the transnasal route, and endoscopic approaches via this route have been increasingly used for surgical access and treatment of neoplastic and nonneoplastic lesions of the anterior and central skull base.17 Examples of nonneoplastic conditions include cerebrospinal fluid (CSF) leaks, mucoceles, encephaloceles, cholesterol granulomas, and allergic and invasive fungal sinusitis.18–26 Endoscopic surgery is also used with increasing frequency for surgical resection of tumors of the sinonasal tract, such as inverted papilloma, angiofibroma, osteomas, and other benign fibro-osseous lesions, and even in selected patients with malignant sinonasal tumors.27–39 The endoscopic approach has become one of the standard surgical techniques for transsphenoidal access to the sella turcica, and it is considered by many centers the preferred surgical approach for treatment of pituitary adenomas.40–48 More recently, there has been an emerging trend to expand the use of transnasal endoscopic approaches in the surgical treatment of suprasellar, petroclival, infratemporal, and other intracranial skull base tumors.49–52 The main advantage of transnasal endoscopic skull base approaches is to provide more direct access to the anterior and central skull base while avoiding craniofacial incisions and extensive bone removal commonly used in open surgical approaches.17 Advances in optical clarity of endoscopic telescopes and high-definition video technology have allowed surgeons to have a magnified view of the skull base, which is not possible with the operating microscope. The wider angle of vision and the ability to use angled lenses also increase the range of the endoscopic visual surgical field compared with the “line of sight” visual field gained by surgical loupes or microscopes.42 Other technological advances that have allowed for the development of this surgical technique include powered instrumentation, improved preoperative imaging quality, and intraoperative image-guidance technologies. Both neurosurgical and otolaryngological disciplines are now using endoscopic and open with endoscopic-assisted surgery to access lesions from the cribriform plate anteriorly to the craniocervical junction posteriorly, as well as the infratemporal fossa laterally.53 A full discussion of these approaches to the skull base is located elsewhere in this text. However, for the purpose of this chapter, it is important to reiterate that endoscopic resection of both neoplastic and nonneoplastic lesions of the skull base has been shown to provide equal outcomes in terms of control of the primary lesion with reduced morbidity in carefully selected patients.27,28,54–56 What follows is a discussion of how some of the inherent technical advantages of surgical robotics may overcome some of the limitations of traditional endoscopic surgery and are leading to this modality defining a role as a viable and useful method for minimally invasive endoscopic skull base surgery. One of the major limitations of traditional endoscopic surgery is optical visibility. The two-dimensional visualization provided by single-channel optical systems in current endoscopes lacks three-dimensional vision; thus, depth perception relies more on tactile than on visual cues. Visual depth perception is particularly important when operating on critical intracranial neurovascular structures, especially when working in a deep and limited space. Current endoscopic techniques also have several ergonomic limitations. Bimanual surgery is only feasible if the endoscope is held by an assistant or a mechanical holder. A surgical assistant is preferred because of the constant need to adjust the position (depth and angle) of the endoscope during endoscopic surgery. This not only limits the direct control of the endoscope by the primary surgeon but also requires the assistance of a relatively experienced endoscopic surgeon who can seam-lessly follow the primary surgeon in every step of the operation. Also, both surgeons have to work within a confined space that, in some cases, limits ergonomic freedom. In addition, as the surgical field gets deeper, longer instruments are needed; with lack of proper arm support, precision may be limited by fine tremor, especially when using fine instrumentation for delicate dissection of critical neurovascular structures. Finally and perhaps the most significant limitation of current transnasal endoscopic techniques is the inability to suture and provide watertight dural closure or reconstruction of dural defects. Endoscopic repair of dural defects relies on nonvascularized fat, mucosal or allogeneic grafts, or vascularized septal or nasal rotational mucosal flaps.23,57,58 These reconstructions are then covered with fibrin sealants and supported by either absorbable or nonabsorbable packing. Although these methods may provide an adequate reconstruction of minor dural tears or defects, their ability to provide safe and reliable reconstruction of larger dural defects remains untested.18,19 Preliminary results suggest that endoscopic repair of larger defects (greater than 2 cm) confers a higher CSF leak rate and complication rate compared with the more standard dural reconstruction using pedicled (axial) flaps, such as the pericranial flap or microvascular free flaps.53,59 Adequate and reliable dural reconstruction is critical in minimizing the morbidity of skull base resections, particularly in patients who received or will undergo high-dose radiation therapy. The line of site microscopic approach via transnasal or limited incisions does alleviate some of the optical, ergonomic, and reconstructive limitations. Three-dimensional view with a good optical clarity is possible, but the field of view is limited. Further, bimanual instrumentation is afforded by this approach, which may make suturing of dural defects possible. However, there are limitations in obtaining wide exposure of the surgical site and precision is limited by natural human tremor amplified by the fulcrum of the long instruments required to access the skull base.
Surgical Robotics
Robotics in Otorhinolaryngology
Minimally Invasive Skull Base Surgery
Technical Advantages and Disadvantages of Surgical Robotics in Skull Base Surgery
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree