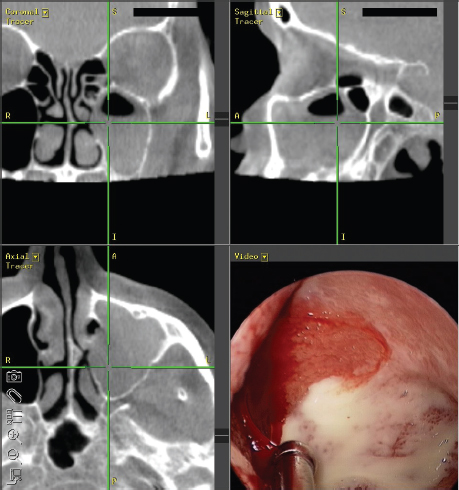
5 Rhinosinusitis Rhinosinusitis (RS) is a group of disorders characterized by symptomatic inflammation of the nose and paranasal sinuses. These disorders affect approximately 15% of the Western population, have substantial effects on the quality of life, and impose a great financial burden to society. Therefore, an appropriate and cost-effective treatment of RS is critical. There are dramatically different forms of RS. To foster effective treatment and research, several major expert panels have convened to put forth standardized definitions and management guidelines for RS, such as the Rhinosinusitis Task Force,1 European Position Paper on Rhinosinusitis and Nasal Polyps (EP3OS),2 the Joint Task Force of Practice Parameters,3 and Clinical Practice Guideline: Adult Sinusitis (CPG:AS).4 For simplicity, this chapter will use the guidelines defined in the CPG:AS and/or EP3OS. Note that fungal RS, including fungus ball, allergic fungal rhinosinusitis (AFRS), acute invasive fungal sinusitis, and chronic fungal RS will be discussed in subsequent chapters. By definition, RS must involve both (1) inflammation of the paranasal sinuses and nasal cavity and (2) related signs/symptoms. If both criteria are not met, the diagnosis is not RS. The term rhinosinusitis is preferred over the term sinusitis, though they are often used interchangeably. RS describes the concomitant inflammation of the contiguous nasal and sinus mucosa, as sinus mucosa is rarely clinically inflamed in the absence of nasal inflammation. The signs and symptoms of RS generally include purulent nasal drainage, nasal obstruction, and facial pain, pressure, or fullness. It has been debated whether physical examination and history are sufficient to establish the diagnosis of RS, without endoscopy and/or radiographic evidence. Particularly with chronic rhinosinusitis (CRS), when management decisions include costly options of prolonged medical therapy and surgery, objective evidence of the condition is favorable. Key diagnostic criteria will be discussed later in the chapter. RS definitions are generally classified on the basis of symptom duration. RS is defined as “acute” (ARS) (less than 4 weeks), “subacute” (4 to 12 weeks), or “chronic” (CRS) (more than 12 weeks).1 Another category of RS, called “recurrent ARS,” refers to three to four episodes of ARS occurring within 1 year with complete interval resolution of symptoms.3,4 Different expert panels use slight variations in these durations and definitions. Typically, ARS denotes symptoms lasting less than 4 weeks, but some definitions use 12 weeks as the cutoff; for example, the most recent EP3OS guidelines define ARS as symptom duration of less than 12 weeks.2 Subacute RS is an additional subcategory used by some systems, and refer to intermediate RS symptom duration as noted above. While CRS typically refers to RS symptoms lasting longer than 12 weeks, some definitions have used 8 weeks as the threshold. CRS is also classified by phenotypical subtype, with the presence or absence of polyps. Chronic rhinosinusitis with nasal polyposis (CRSwNP) is characterized by nasal polyps (Fig. 5.1) and eosinophilic inflammation initiated and sustained by interleukin (IL)-5 and eotaxin. Chronic rhinosinusitis without nasal polyposis (CRSsNP) is characterized by the absence of polyps and neutrophilic inflammation. AFRS is characterized by eosinophilic mucin and noninvasive fungal elements. An additional level of subclassification, based on the severity of symptoms, allows for tailored management strategies of RS. The EP3OS guidelines classify severity based on a visual analog scale that has been statistically validated for use in RS. On this scale, patients rate their symptoms from 0 (“not troublesome”) to 10 (“worst thinkable troublesome”). Scores from 0 to 3 are considered mild, 4 to 7 moderate, and 8 to 10 severe.2 Figure 5.1 Endoscopic view of chronic rhinosinusitis with nasal polyposis, right nasal cavity. Multiple staging systems exist to stratify severity of CRS based on symptoms, endoscopic findings, computed tomography (CT) scan findings, or a combination thereof. The variety of systems likely reflects the failure of any single system to accurately stratify patients. For most of the staging systems, the criteria are too complex for routine clinical use. The Lund-McKay system is based solely on CT findings and is the most widely used system. Each individual sinus (frontal, maxillary, anterior ethmoid, posterior ethmoid, and sphenoid) is scored as follows: 0 = clear, 1 = partial opacification, and 2 = total opacification. The ostiomeatal complex is unique because it is scored in a binary manner as follows: 0 = clear and 2 = occluded.5 In ARS, an inflammatory reaction to a viral upper respiratory tract infection characterizes most cases. Odontogenic sources also account for a minority of cases of maxillary sinusitis (Fig. 5.2). The pathophysiology of ARS involves interplay between a predisposing condition (e.g., allergic rhinitis, septal deformity, immune deficiency, and environmental factors), infection, and consequent inflammatory response in the sinonasal mucosa. The inflammatory response involves edema, fluid extravasation, and mucus production. The inflammatory cascade involves T-helper type 1 cytokine polarization associated with tumor necrosis factor-b and interferon-g. Proinflammatory cytokines such as IL-1b, IL-6, and IL-8 are potent chemoattractive agents for neutrophils.6 Mucosal inflammation may lead to obstruction of normal sinus outflow tracts. This obstruction impedes normal ventilation and drainage leading to a lower partial pressure of oxygen, decreased ciliary clearance, and stasis of secretions. A secondary bacterial infection may develop. However, more than 90% of the time ARS is viral. Rhinovirus, coronavirus, influenza, respiratory syncytial virus, and parainfluenza virus are the common instigators.6,7 The common bacteria in adult acute bacterial rhinosinusitis (ABRS) are Streptococcus pneumoniae (20 to 45%), Haemophilus influenzae (20 to 35%), Moraxella catarrhalis (2 to 10%), other streptococci (0 to 10%), and Staphylococcus aureus (0 to 10%).7 S. aureus was considered a contaminant in the past, but meta-analysis suggests that it is a true pathogen in approximately 10% of ABRS cases in adults.8 Anaerobes may also be implicated. Widespread use of vaccination has resulted in changes in the bacteriology of ABRS. However, there is no strong evidence of a change in the incidence of ABRS after widespread use of conjugate pneumococcal vaccination. The l.f. type B vaccine reduced the incidence of invasive disease and likely played a role in ABRS. However, as the vaccination strains became less prevalent, other serotypes emerged as potential causes of invasive disease.9 Figure 5.2 Rhinosinusitis involving the left maxillary sinus, from an odontogenic source. This patient developed symptoms of rhinosinusitis, refractory to medical management, following dental implantation. ARS has been historically diagnosed on the basis of clinical history. However, some expert guidelines recommend special assessments to confirm the diagnoses. Other guidelines provide two sets of recommendations: one for primary care providers and another for otolaryngologists. The CPG:AS and EP3OS diagnostic criteria for ARS are listed in Table 5.1. Most otolaryngologists believe that nasal endoscopy is helpful to assess the middle meatus and sphenoethmoidal recess for purulence (Fig. 5.3), which should be cultured in severe disease. CT is the preferred imaging option in cases of severe disease, immunocompromised states, or suspected complications. Plain radiography is neither cost-effective nor useful. A critical step for the clinician is to differentiate ARS into ABRS and viral rhinosinusitis (VRS). This is clinically challenging and the distinction is made by duration of symptoms. VRS is suspected when symptoms last less than 10 days. ABRS is suspected when symptoms last more than 10 days or worsens after initial improvement.4 Table 5.1 Diagnostic Criteria for Acute Rhinosinusitis
Rhinosinusitis: Definition, Diagnosis, and Classification
Classification by Duration of Symptoms
Classification of Chronic Rhinosinusitis by Phenotypical Subtype: Presence or Absence of Polyps
Classification by Severity of Symptoms
Staging
Acute Rhinosinusitis
Pathophysiology and Microbiology
Diagnosis
Summary of CPG:AS Guidelines | Summary of EP3OS Guidelines |
Up to 4 wk of purulent nasal drainage accompanied by nasal obstruction, facial pain-pressure-fullness, or both • Purulent nasal discharge may be reported or observed on physical examination • Nasal obstruction may be reported as nasal obstruction, congestion, blockage, or stuffiness, or observed on physical examination | Up to 12 wk of two or more symptoms, one of which should be either nasal obstruction or discharge (anterior/posterior nasal drip): • ± Facial pain/pressure • ± Reduction or loss of smella • Endoscopic signs of polyps and/or mucopurulent discharge and/or edema/mucosal obstruction • CT mucosal changes |
Sources: Fokkens W, Lund V, Mullol J. European position paper on rhinosinusitis and nasal polyps 2007. Rhinol Suppl 2007;20:99.
Rosenfeld RM, Andes D, Bhattacharyya N, et al. Clinical practice guideline: adult sinusitis. Otolaryngol Head Neck Surg 2007;137(Suppl 3):S7.
Treatment
The goals of treatment of ARS are to alleviate or minimize symptoms, reduce inflammation, eradicate pathogens, and promote sinus drainage. The fundamental difficulty in treating ARS is determining which cases warrant antibiotics. Though only an estimated 1 to 2% of ARS has a bacterial etiology, survey data show overuse of antibiotics for 80 to 90% of ARS.10
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree