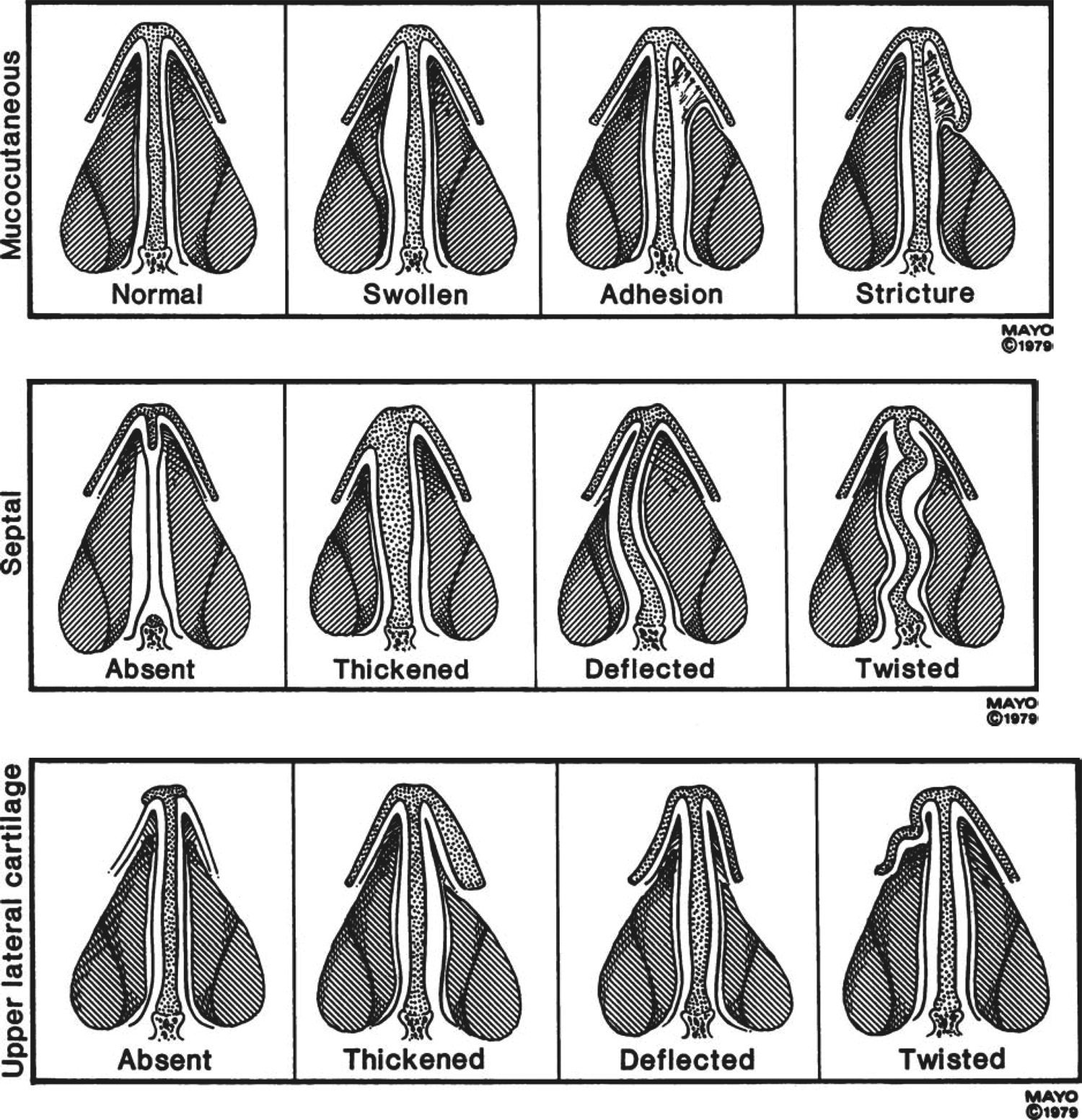
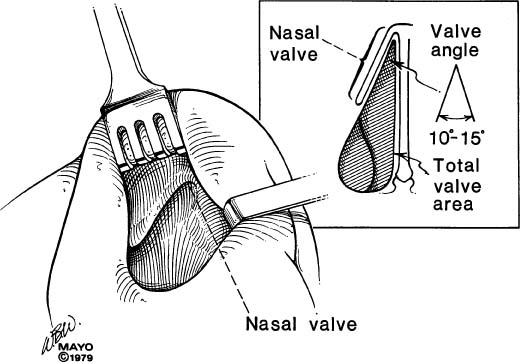
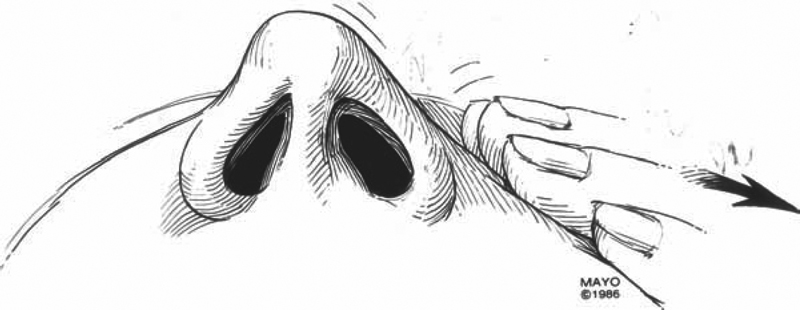
39 Revision Surgery of the Nasal Septum Nasal obstruction and difficulty breathing in a patient who has had a previous nasal operation present a major challenge to rhinologists. This chapter offers some suggestions regarding the diagnosis and surgical treatment of this problem. The key to successful revision surgery is to accurately diagnose the cause for surgical failure. The three categories of surgical failure are 1. Failure to properly diagnose and treat preexisting pathology of the septum (failures to correct a caudal end deformity [area 1] or valve pathology [area 2] are common findings) 2. Partial treatment of correctly diagnosed pathology 3. Sequelae, such as septal perforations, over-resection, scarring, adhesions, and atrophy, as a result of the previous operation The goal of the surgery is to “reconstitute normality.” The challenge is to decide what is normal. There are three options available to the surgeon to address this challenge, namely, by adding, removing, or repositioning septal structures as indicated by the preoperative and intraoperative evaluation and findings. Ideally, an evaluation of a patient with a history of previous surgery begins with the collection of surgical records, clinical notes, and preoperative photographs. These data contain clues as to the etiology of the surgical failure. Although surgical reports are frequently incomplete and lack surgical details, information such as materials used for repair, planes of dissection used, and difficulties encountered by the previous surgeon may be gleaned from these reports. Technical difficulties may have been encountered, such as excessive bleeding, torn mucosal flaps, or intraseptal scarring, and these notes may give an indication as to the cause for the residual nasal airway obstruction. The physical examination should emphasize three critical sites: the mucosa and soft tissue, the septum, and the valve region. Figure 39.1 demonstrates abnormalities of these three areas. Patient history and physical examination are the bedrock of clinical medicine and require attention to detail. Mucosal disorders such as allergic rhinitis, nasal atrophy, chronic rhinosinusitis, nasal polyposis, Wegener granulomatosis, and even hypothyroidism are commonly encountered and therefore must be properly diagnosed and treated. Most mucosal disorders are treated medically, although submucosal cauterization and radiofrequency ablation of enlarged turbinates are becoming common practices. The septum is inspected for obstructing bends, impactions, perforations, and structural integrity. The septum must be palpated with the gloved finger and a cotton-tipped applicator to discern where tissue is missing and/or displaced. No examination is complete without topical decongestion. The prior surgeon may have overlooked spurs or impactions, especially when a cosmetic procedure was performed without sufficient intranasal examination. The caudal end of the septum, anterior nasal spine, and premaxilla may not have been corrected. Palpation of the caudal end and the external nose is important in determining tip support. The amount of cartilage and bone remaining in the intraseptal space should be determined, because this tissue is often necessary for reconstructive purposes. Nasal deformities may occur as a result of an overzealous nasal septoplasty, most notably a saddle-type deformity resulting from the failure to leave an adequate dorsal strip. Nasal tip ptosis or weakness can result from manipulations of the caudal end and can result in functional and cosmetic deficits. Fig. 39.1 Common abnormalities of the intranasal soft tissues (top), septum (middle), and upper lateral cartilage (lower) that can contribute to nasal obstruction. Particular attention is given to the valve angle and the valve area (Fig. 39.2). This entire region is inspected for pathology. The examination begins without using a nasal speculum, as the tines of this instrument can obstruct important pathology in the nasal valve region. A nasal lobular elevator designed by Fausto Infante-Lopez (Fig. 39.3) is useful for inspection. Areas to be inspected include the septum, upper lateral cartilage, premaxillary wing, floor of the pyriform aperture, and head of the inferior turbinate. Dynamic evaluation is necessary, as collapse with inspiration may indicate a weakening of the upper lateral cartilage. A Cottle maneuver (Fig. 39.4) is used to determine the contribution of upper lateral collapse to nasal airway obstruction due to narrowing of the valve angle. Attention needs to be paid to both the internal and external valves formed by the nasal lobule and lower lateral cartilage. Fig. 39.2 Anatomy of the nasal valve. The junction between the caudal end of the upper lateral cartilage and the septum creates the valve angle. This angle is normally 10 to 15 degrees. The valve is best inspected by retracting the lobule without a nasal speculum. Pathology in the valve angle, septum, or head of the inferior turbinate can all contribute to valvular nasal obstruction. Fig. 39.3 The Fausto nasal lobule elevator. Preoperative tests include olfaction testing, rhinomanometry, and photographs. Allergy testing, acoustic rhinometry, and computed tomography (CT) scans can also be of aid to the surgeon. Rhinomanometry provides quantitative evidence of obstruction to nasal airflow. These pressure measurements allow the surgeon to calculate nasal airway resistance before and after decongestion, which helps determine the relative contributions of mucosal versus structural abnormalities toward nasal obstruction. These data are consistent enough to provide for postoperative comparison. CT scans are most helpful in determining concomitant sinus pathology and may also demonstrate residual skeletal, structural, and soft tissue abnormalities. Acoustic rhinometry may aid the surgeon in localizing an abnormality. We believe that photographs are necessary even for noncosmetic procedures. These serve to properly document the preoperative appearance of the nose to avoid any misunderstandings or legal consequences if a previously unnoticed cosmetic defect is noted by the patient postoperatively. Fig. 39.4 Demonstration of the Cottle maneuver. The cheek is pulled away from the midline, which pulls the upper lateral cartilage laterally, thus opening the valve angle. The patient is asked if this reduces the nasal obstruction; an affirmative answer indicates a positive test. Preoperatively, the surgeon must have a detailed discussion with the patient and his or her family regarding the goals and risks of the procedure as well as the possibility of additional surgery. The preoperative discussion is an opportunity for the surgeon to review photographs and tests, to explain the procedure, and to demonstrate the pathology by video endoscopy and CT scans. This is also an opportunity for the patient and family to ask questions. The surgeon must address the expected benefits of surgery, the chance for complete versus partial relief of symptoms, and cosmetic concerns. All of the standard risks should be discussed, including bleeding, infection, pain, and discomfort. The surgeon should explain the postoperative recovery and appointment schedule, including the timing of dressing and stent removal. Patients undergoing revision surgery should understand that a further revision is possible. The risks of septal perforation, nasal deformity, and persistent obstruction should also be discussed.
Evaluation
Physical Examination
Soft Tissue and Mucosal Changes
Nasal Septum
The Nasal Valve

Ancillary Testing
Preoperative Discussion
Surgical Treatment
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


