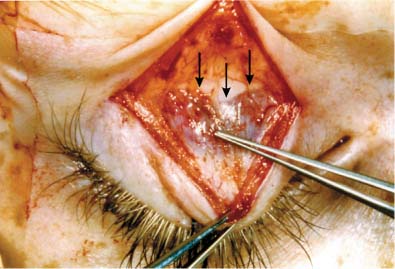
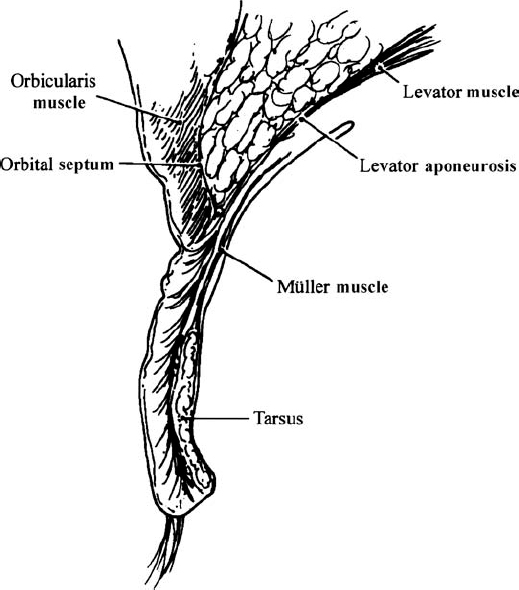
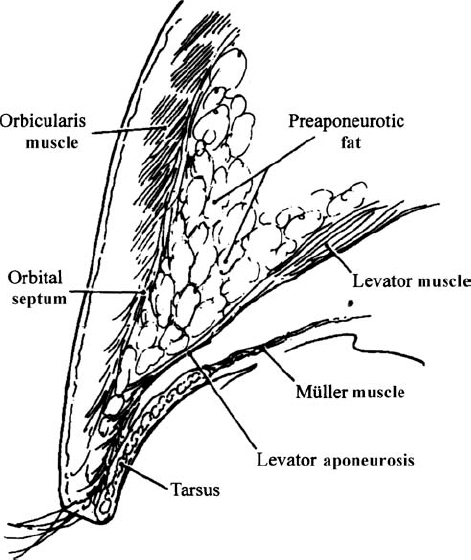
33 Revision Ptosis Surgery The surgical correction of blepharoptosis is one of the most challenging procedures in facial plastic surgery. Not only must the desired functional and aesthetic outcome of upper eyelid elevation be achieved, but adequate eyelid closure and corneal protection, vital to avoiding exposure keratoconjunctivitis and corneal ulceration, must also be maintained. Other complications of ptosis surgery include undercorrection, overcorrection, asymmetry, eyelid margin contour deformity, lash ptosis, entropion, ectropion, lagophthalmos, poor upper eyelid crease, superior rectus or superior oblique paresis, suture granuloma, infection, hemorrhage, and loss of vision. Historically, unpredictable results in ptosis surgery were common, and it is no surprise that revision surgery was often necessary. However, by taking a systematic approach with careful respect of eyelid anatomy, most complications after ptosis surgery can be improved or corrected. In this chapter, we describe our logical approach to revision ptosis surgery. Prior to any surgical intervention, thorough evaluation of and consultation with the patient are mandatory, especially when the patient has already had complications requiring revision surgery. Eyelid height, eyelid fold, margin contour, eyelid crease position, abnormalities (e.g., eyelid notching), and symmetry should be carefully noted during the preoperative evaluation (Fig. 33.1). The original cause for the ptosis should be determined (aponeurotic, traumatic, neurogenic, mechanical, or congenital). Slit-lamp examination of the cornea with assessment of tear production and eyelid closure should also be performed prior to surgery to determine if the patient is prone to developing a dry eye. Visual acuity documentation and preoperative photographs are very important for the record and for medicolegal documentation. If the ptosis is functional and to be covered by insurance, visual field examinations are also essential. Equally important is evaluating the prior surgical procedures performed on the eyelids. Was the prior ptosis surgery performed through an external or internal approach? Was the procedure combined with upper blepharoplasty and fat excision? Intraoperative complications should be noted. The eyelid should be everted to evaluate the condition of the tarsus and whether a prior shortening has been performed. If the eyelid initially achieved a good height after surgery and recurred with time, neurologic or neuromyopathic conditions should be considered. Careful and thorough discussion with the patient should occur prior to surgery so that he or she understands the goals and limitations of revision ptosis surgery. Successful and predictable results in ptosis surgery require precise knowledge of eyelid anatomy. Eyelid elevation is normally a function of the levator palpebrae muscle and the sympathetically innervated Müller muscle.1 In most cases of acquired ptosis, defects in the levator aponeurosis can be observed. These defects include disinsertion, dehiscence, and rarefaction of the levator aponeurosis (Fig. 33.2).2,3 They may result from age-related changes or be associated with orbital swelling or excessive eyelid squeezing. Successful surgical correction of ptosis should be directed toward strengthening the existing eyelid elevators.4 In revision ptosis surgery, where the normal eyelid anatomy may be distorted from prior surgery or scarring, identification of the levator aponeurosis is crucial for successful revision surgery. The preaponeurotic fat pad is key to identifying the levator aponeurosis, as the aponeurosis is immediately behind the fat pad, and scar tissue may obscure other natural landmarks. Fig. 33.1 A 52-year-old man after two attempted ptosis repairs of the right upper eyelid. Note the persistent ptosis and high, asymmetric eyelid crease on the right. *The authors have no financial interest in the techniques described herein. Fig. 33.2 Disinsertion of the levator aponeurosis as the cause of ptosis. Arrows outline the edge of the disinserted aponeurosis. Müller muscle is below the disinserted edge of the aponeurosis. The forces point to the peripheral arcade in Müller muscle, which helps identify this structure. The levator muscle originates above the anulus of Zinn in the apex of the orbit. It runs anteriorly in the orbit just inferior to the orbital roof.5 The levator becomes aponeurotic below the Whitnall ligament (superior transverse ligament), then descends posterior to the preaponeurotic fat pads and inserts onto the anterior surface of the tarsus.3 Anterior fibers of the aponeurosis attach to the skin through the pretarsal orbicularis muscle to form the eyelid crease. The Müller muscle originates from the levator ~12 mm above the tarsus and inserts onto the superior border of the tarsus. The orbital septum is a multilaminated fibrillar membrane that can be mistaken for the levator aponeurosis in ptosis surgery.6 The septum and its relationship with the levator aponeurosis is also the key anatomical distinction between the Caucasian eyelid and the Asian eyelid.7 In the Caucasian eyelid, the orbital septum fuses with the levator aponeurosis above the superior tarsal border (Fig. 33.3). At the inferior border of the fused septum/aponeurosis, anterior fibers pass through the orbicularis muscle and attach to the skin to form the eyelid crease. In the Asian eyelid, the orbital septum fuses with the levator aponeurosis below the superior tarsal border (Fig. 33.4). This allows preaponeurotic fat to extend inferiorly and produce a thickened, full-appearing eyelid. The inferior extension of the orbital septum also prohibits the superficial attachments of the levator aponeurosis from attaching to the skin. The eyelid crease is subsequently poorly developed or, if present, is much lower than in the Caucasian eyelid. Appreciation of the anatomical distinctions between the Caucasian and Asian eyelid is important for all surgeons performing ptosis surgery. Fig. 33.3 In the Caucasian eyelid, the orbital septum fuses with the levator aponeurosis above the superior tarsal border. Fig. 33.4 In the Asian eyelid, the orbital septum fuses with the levator aponeurosis below the superior tarsal border. In most cases of blepharoptosis, surgery directed toward tightening of the levator aponeurosis is required for successful correction.4 The exception would be for patients with poor levator function (<4 mm of levator excursion from downgaze to upgaze), such as in some cases of congenital ptosis.8 These patients usually require a superior tarsectomy or frontalis suspension for adequate correction of their blepharoptosis.9 Patients with moderate or good levator function achieve the best postoperative results with levator aponeurosis tightening.10 Many techniques have been described for the surgical correction of blepharoptosis. Bowman first described levator shortening through a transconjunctival approach in 1857.11 Eversbusch described the anterior approach to levator shortening in 1883.12 Some surgeons have advocated surgical correction of ptosis with resection and advancement of the Müller muscle and conjunctiva alone or with a superior tarsectomy.13,14 Unfortunately, the amount of eyelid elevation achieved is often limited and unreliable. We prefer an external approach to the levator aponeurosis in revision ptosis surgery as described by Anderson and Dixon in 1979.4 They presented a reliable and practical approach to aponeurosis surgery that could be easily modified for patients with congenital as well as acquired ptosis, except for those with poor levator function. The advantages of the external approach during revision ptosis surgery include (1) reestablishing and maintaining normal anatomical planes during dissection; (2) preserving all elevating structures, including the Müller muscle; (3) easy intraoperative adjustment of overcorrections and undercorrections; and (4) preserving tear-producing structures within the conjunctiva of the superior fornix.
Preoperative Assessment
Anatomical Review

Surgical Approach
Surgical Technique
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


