Purpose
To compare prospectively detection of progressive retinal nerve fiber layer thickness (RNFL) atrophy identified using time-domain optical coherence tomography with visual field progression using standard automated perimetry in glaucoma suspect and preperimetric glaucoma patients or perimetric glaucoma patients.
Design
Prospective, longitudinal clinical trial.
Methods
Eligible eyes with 2 years or more of follow-up underwent time-domain optical coherence tomography and standard automated perimetry every 6 months. The occurrence of visual field progression was defined as the first follow-up visit reaching a significant ( P < .05) negative visual field index slope over time. RNFL progression or improvement was defined as a significant negative or positive slope over time, respectively. Specificity was defined as the number of eyes with neither progression nor improvement, divided by the number of eyes without progression. Cox proportional hazard ratios were calculated using univariate and multivariate models with RNFL loss as a time-dependent covariate.
Results
Three hundred ten glaucoma suspect and preperimetric glaucoma eyes and 177 perimetric glaucoma eyes were included. Eighty-nine eyes showed visual field progression and 101 eyes showed RNFL progression. The average time to detect visual field progression in those 89 eyes was 35 ± 13 months, and the average time to detect RNFL progression in those 101 eyes was 36 ± 13 months. In multivariate Cox models, average and superior RNFL losses were associated with subsequent visual field index loss in the entire cohort (every 10-μm loss; hazard ratio, 1.38; P = .03; hazard ratio, 1.20; P = .01; respectively). Among the entire cohort of 487 eyes, 42 had significant visual field index improvement and 55 had significant RNFL improvement (specificity, 91.4% and 88.7%, respectively).
Conclusions
Structural progression is associated with functional progression in glaucoma suspect and glaucomatous eyes. Average and superior RNFL thickness may predict subsequent standard automated perimetry loss.
Glaucoma is a multifactorial optic neuropathy characterized by progressive neurodegeneration of retinal ganglion cells and their axons, characterized by retinal nerve fiber layer (RNFL) attenuation, a specific pattern of damage to the optic nerve head, and visual field loss. Although both structural and functional damage occur in glaucoma, controversy exists regarding whether substantial RNFL attenuation precedes functional loss measured by standard automated perimetry. It is widely recognized that both structure and function are useful to detect glaucoma progression, given discordance in the timing of detecting longitudinal changes in the optic nerve and visual field. The relationship between signal-to-noise ratio, stage of glaucomatous damage, and the technique and region of visual field studied have significant impacts on the comparison of structure and function for the progression of glaucoma.
Novel imaging technologies have been developed that are capable of quantifying early glaucomatous damage at the micron level using structural measures. Time-domain (TD) optical coherence tomography ([OCT]; Stratus OCT; Carl Zeiss Meditec, Dublin, California, USA) is a high-resolution, micron-scale, cross-sectional imaging method that provides quantitative assessments of the retina and optic nerve head and is capable of discriminating between normal and glaucomatous eyes and detecting longitudinal loss of RNFL thickness in glaucoma.
The visual field index (VFI) is a calculated index allocated to each visual field that determines the level of abnormality of the field. The VFI uses the pattern deviation (PD) probability map to identify the test locations that are considered either normal and scored as 100% or absolute defect and scored as 0%. The remaining test locations with relative loss on the PD plot are scored in as a percentage based on their total deviation value and age-corrected normal threshold. Because VFI uses PD probability maps, it is less affected by cataract. A weighting procedure is applied to each test location using an estimate of the spatial magnification present in the occipital cortex that divides the test pattern into 5 concentric rings of increasing eccentricity. The 4 test central locations, not including measurement of foveal threshold, are allotted the highest weight, and the weights decrease with increasing eccentricity. The VFI is the mean of all weighted scores in percent.
The VFI scoring system masks early glaucomatous damage by assigning a perfect score to the test locations that are considered normal on the PD plot, but may have decreased total deviation values. The purpose of this study was to compare prospectively the detection of progressive RNFL loss identified using TD OCT with visual field progression measured using standard automated perimetry in glaucoma suspect and preperimetric glaucoma patients and in perimetric glaucoma patients.
Methods
Study Population
This was a prospective, nonrandomized, longitudinal clinical trial. Participants consisted of glaucoma suspect and preperimetric glaucoma patients and perimetric glaucoma patients with 28 months or more of follow-up who were enrolled in Advanced Imaging for Glaucoma Study conducted at the Bascom Palmer, Casey, and Doheny Eye Institutes and the University of Pittsburgh Medical Center Eye Center. Inclusion criteria common to both groups consisted of spherical equivalent refractive error between −7.00 and 3.00 diopters (D) sphere, best-corrected visual acuity of 20/40 or better, age between 40 and 80 years, and no prior history of intraocular surgery except for uncomplicated cataract extraction. Subjects with ocular disease other than glaucoma or cataract, parapapillary atrophy extending to 1.7 mm from the center of the optic disc, unreliable visual field, or poor-quality optic nerve head or RNFL images were excluded.
The glaucoma suspect and preperimetric glaucoma eyes consisted of eyes with ocular hypertension characterized by intraocular pressure of 24 mm Hg or more with normal optic discs and normal standard automated perimetry defined as glaucoma hemifield test results within normal limits and mean deviation (MD) and pattern standard deviation (PSD) within 95% confidence interval limits, or patients with glaucomatous optic neuropathy on funduscopic examination and review of stereoscopic optic disc photographs, but normal visual field. Glaucomatous optic neuropathy was defined as neuroretinal rim narrowing to the optic disc margin, notching, excavation, or RNFL defect. The perimetric glaucoma patients had glaucomatous optic nerve damage and corresponding abnormal visual field defined as abnormal glaucoma hemifield test results and PSD outside normal 95% confidence interval limits. Patients with visual field abnormalities had at least 1 confirmatory visual field examination. All patients underwent a baseline examination consisting of a complete ophthalmic examination including slit-lamp biomicroscopy, gonioscopy, Goldmann applanation tonometry, ultrasound pachymetry, dilated stereoscopic examination and photography of the optic disc, standard automated perimetry, and RNFL imaging. The RNFL imaging was performed using TD OCT (version 5.0.1, Stratus OCT; Carl Zeiss Meditec) every 6 months. During the follow-up period, each patient was treated at the discretion of the attending physician.
Time-Domain Optical Coherence Tomography
The TD OCT was used to measure the RNFL thickness. The software determines the RNFL thickness as the distance between the vitreoretinal interface and a posterior border based on a predefined reflectivity signal level. The calibration was checked annually in accordance with the manufacturer’s guidelines by authorized technicians. At each visit, two images were acquired from each subject. Each image consisted of 3 sets of 256 A-scans along a 3.4-mm diameter circumpapillary scan centered at the optic nerve head. The fast-scanning mode was used, in which all scans are acquired and aligned automatically after initial positioning and acquisition by the operator. The repeat scan option incorporated in TD OCT was used to optimize the alignment of the follow-up scan circle and the baseline image. Peripapillary RNFL thickness parameters evaluated in this study were average thickness (360 degrees), superior quadrant thickness (46 to 135 degrees), and inferior quadrant thickness (226 to 315 degrees). These values were provided in the printout after averaging the results of 3 sequential circular scans captured during acquisition. Poor-quality scans were excluded, including images that were unfocused, poorly centered, obtained during eye movement, or had a scan score less than 6, or those with failure to segment the borders of the RNFL correctly.
Definition of Progression
Standard automated perimetry was performed using the Swedish interactive threshold algorithm (Humphrey Field Analyzer 750 II-i, 24-2 SITA Standard; Carl Zeiss Meditec). Reliable test results, defined as 33% or less fixation losses, false-negative rates, and false-positive rates, were included. All patients were experienced with automated perimetry and had undergone a minimum of 2 visual field tests before study enrollment.
Both eyes of eligible patients enrolled in the Advanced Imaging for Glaucoma Study with 28 months or more of follow-up and reliable visual field were included. TD OCT and standard automated perimetry were measured every 6 months. Progression was defined as a significant ( P < .05) negative slope in the annual rate of change in VFI and RNFL. The occurrence of visual field progression was defined as the first follow-up visit reaching a significant ( P < .05) negative VFI slope over time. Improvement was defined as a significant ( P < .05) positive slope in the annual rate of change in VFI and RNFL. Specificity was defined as the number of eyes with neither progression nor improvement, divided by the number of eyes without progression.
Statistical Analysis
Statistical analysis was performed using SAS software version 9.2 (SAS Inc, Cary, North Carolina, USA) to detect progressive RNFL loss and visual field progression in glaucoma suspect and preperimetric glaucoma patients and in perimetric glaucoma patients. All tests were 2-sided, and a P value of less than .05 was considered significant. The average of 2 high-quality measurements that met the inclusion criteria was used for the statistical analysis. An analysis of variance was used to compare the continuous variables, and the chi-square test was used for the categorical variables. When applicable, the general estimating equation method was used to adjust for correlation between the 2 eyes of the same patient. Univariate and multivariate Cox proportional hazard ratios (HRs) with 95% confidence intervals were calculated using univariate and multivariate models with RNFL loss as a time-dependent covariate to identify the risk factors predictive of visual field progression.
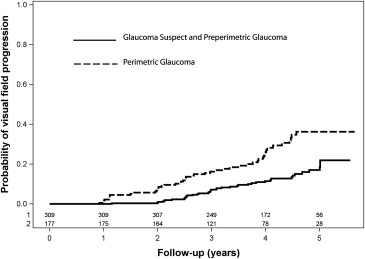
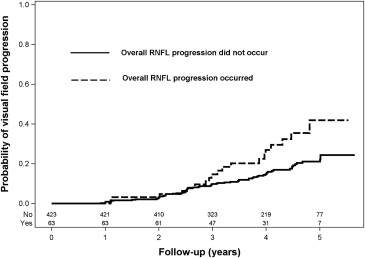
Univariate Cox proportional hazard regression models examined the HRs for the individual parameters and were not adjusted for the presence of other factors. Predictors with a P value of 0.1 or less were evaluated for the multivariate models through stepwise selection. Separate models were constructed for multivariate analyses. Each model included 1 imaging parameter and age and visual field PSD at baseline. For Cox models, a technique called robust sandwich covariance estimate was used in the Wald tests to adjust for correlation between 2 eyes from the same patient. Three types of Kaplan-Meier curves were created to compare the survival times for perimetric glaucoma eyes versus glaucoma suspect and preperimetric glaucoma eyes ( Figure 1 ), the eyes that had significant loss of RNFL versus those that did not ( Figure 2 ), and RNFL loss versus VFI loss (explained in the Results).
Results
Four hundred eighty-seven eyes of 246 patients (310 glaucoma suspect and preperimetric glaucoma patients and 177 perimetric glaucoma patients) were included, of which 131 (53.3%) patients had glaucoma suspect and preperimetric glaucoma in both eyes, 65 (26.4%) patients had perimetric glaucoma in both eyes, and 50 (20.3%) patients had perimetric glaucoma in 1 eye and glaucoma suspect or preperimetric glaucoma in the other eye. Table 1 demonstrates demographics and baseline characteristics of 2 groups of perimetric glaucoma eyes and glaucoma suspect and preperimetric glaucoma eyes. Mean age of the entire study group was 60.3 ± 9.5 years (range, 40 to 80 years). Each eye underwent both visual field and TD OCT examinations at every visit. The average number of visual fields and OCT examinations for each eye was 8.6 ± 2, with a minimum of 4 and a maximum of 12 measurements. Only 2 patients had 4 measurements within a time span of 30 and 36 months. The mean VFI, MD, and PSD were 88.77 ± 13.08%, −3.82 ± 4.28 dB, and 5.37 ± 4.21 dB, respectively, in perimetric glaucoma patients and 99.07 ± 1.14%, −0.23 ± 1.04 dB, and 1.61 ± 0.38 dB in glaucoma suspect or preperimetric glaucoma patients (all P < .001). The average retinal nerve fiber layer thickness (RNFLT) RNFLT was 76.44 ± 13.57 μm in perimetric glaucoma patients and 92.74 ± 12.20 μm in glaucoma suspect or preperimetric glaucoma patients ( P < .001). Mean follow-up time was 36.4 ± 13.8 months in perimetric glaucoma patients and 40.6 ± 11.5 months in glaucoma suspect or preperimetric glaucoma patients ( P < .001). Mean intraocular pressure was 14.7 ± 3.7 mm Hg in perimetric glaucoma patients and 16.8 ± 3.8 mm Hg and glaucoma suspect or preperimetric glaucoma patients ( P < .001).
| Perimetric Glaucoma Eyes (n = 177; Patients, n = 115) | Glaucoma Suspect or Preperimetric Glaucoma Eyes (n = 310; Patients, n = 181) | P Value | |
|---|---|---|---|
| Age (y) a | 62.2 ± 9.4 (40 to 80) | 59.8 ± 9.6 (40 to 79) | .14 b |
| Gender | .75 c | ||
| Male | 46 (40%) | 69 (38.1%) | |
| Female | 69 (60%) | 112 (61.9%) | |
| Ethnicity | .59 c | ||
| White | 62 (62.6%) | 116 (64.1%) | |
| Hispanic | 15 (13.0%) | 20 (11.1%) | |
| Black | 12 (10.4%) | 20 (11.1%) | |
| Others | 16 (13.9%) | 25 (13.8%) | |
| Family history of glaucoma | 56 (48.7%) | 94 (51.9%) | .60 c |
| Follow-up duration (mos) a | 36.4 ± 13.8 (30 to 66) | 40.6 ± 11.5 (30 to 66) | <.001 b |
| Diagnosis | POAG, n = 160 Secondary GL, n = 12 PACG, n = 5 | OHT, n = 88 ONH/RNFL defect, n = 187 OHT + ONH/RNFL, n = 22 Fellow eye with PG, n = 13 | |
| IOP (mm Hg) a | 14.73 ± 3.74 (4.00 to 33.00) | 16.78 ± 3.75 (6.50 to 27.00) | <.0001 b |
| CCT (μm) a | 542.0 ± 35.4 (448 to 697) | 555.4 ± 34.19 (460 to 677) | <.0001 b |
| SAP a | |||
| MD (dB) | −3.82 ± 4.28 (–20.7 to 1.59) | −0.23 ± 1.04 (–7.7 to 3.1) | <.0001 b |
| PSD (dB) | 5.37 ± 4.21 (0 to 16.5) | 1.61 ± 0.38 (0.9 to 4.5) | <.0001 b |
| VFI (%) | 88.77 ± 13.08 (37 to 100) | 99.07 ± 1.14 (93 to 100) | <.0001 b |
| OCT (μm) a | |||
| Average | 76.44 ± 13.57 (35.4 to 121.0) | 92.74 ± 12.20 (52.8 to 127.9) | <.0001 b |
| Temporal quadrant | 59.23 ± 15.15 (24 to 95) | 67.43 ± 14.09 (32 to 113) | <.0001 b |
| Superior quadrant | 91.39 ± 21.01 (33 to 147) | 111.10 ± 20.58 (56 to 168) | <.0001 b |
| Nasal quadrant | 64.39 ± 16.98 (31 to 134) | 74.14 ± 17.35 (34 to 146) | <.0001 b |
| Inferior quadrant | 90.81 ± 23.11 (43 to 154) | 118.20 ± 18.79 (71 to 175) | <.0001 b |
a Data are presented as mean ± standard deviation (minimum to maximum).
b Analysis of variance adjusted for intereye correlation.
Eighty-nine (18%) eyes (41 glaucoma suspect or preperimetric glaucoma eyes and 48 perimetric glaucoma eyes; P < .001) showed visual field progression, and 101 (21%) eyes (56 glaucoma suspect or preperimetric glaucoma eyes and 45 perimetric glaucoma eyes; P = .07) showed RNFL progression, of which 5 (1%) eyes showed visual field and RNFL progression simultaneously, 63 (12.9%) eyes showed visual field progression without RNFL progression, and 7 (1.4%) eyes showed visual field progression preceding RNFL progression. The average time to detect functional loss using visual fields in these 70 eyes was 35.0 ± 13.2 months.
Seventy-five (15.4%) eyes showed RNFL progression without visual field progression, 63 (12.9%) eyes showed VFI progression without RNFL progression, and 26 eyes demonstrated progression using both methods ( P = .35, McNemar test).
Among the 26 eyes that demonstrated progression using both methods, 14 (3%) eyes showed RNFL progression preceding visual field progression, 7 (1.4%) eyes showed visual field progression preceding RNFL progression, and 5 (1.03%) eyes showed simultaneous progression using both methods ( P = .18, McNemar test). The average time to detect structural loss using TD OCT in these 89 eyes was 35.8 ± 13.1 months ( P = .9). Three hundred twenty-three eyes showed no RNFL or visual field progression.
Table 2 demonstrates the number of eyes showing progression by VFI criteria in the glaucoma suspect or preperimetric glaucoma groups and the perimetric glaucoma group. The highest rate of visual field progression was observed in the perimetric glaucoma group (48/177 [27%]). Table 3 demonstrates the annual rates of loss in visual field indices calculated using linear regression analysis over time in the entire cohort accounting for the inclusion of both eyes. The rates of loss were steeper significantly in the perimetric glaucoma group compared with the glaucoma suspect and preperimetric glaucoma group for all 3 visual field indices of VFI, MD, and PSD. Table 4 demonstrates the annual rates of loss in RNFL parameters measured by TD OCT using a linear regression analysis technique. The annual rate of RNFL loss was steeper significantly in the perimetric glaucoma group compared with glaucoma suspect or preperimetric glaucoma group for average, superior, inferior, and temporal RNFL thickness values. Table 5 demonstrates that the rate of VFI loss per year was significantly steeper in the eyes that had significant RNFL loss compared with those that did not have RNFL loss in the perimetric glaucoma group. Table 6 compares baseline visual field and RNFL parameters in 2 groups of eyes that showed progression using significant VFI slope versus the eyes that showed significant RNFL slope. Tables 7, 8 , and 9 demonstrate the results of the univariate and multivariate Cox models for the calculation of proportional HRs to identify the risk factors predictive of visual field progression.
| Patient Group | Visual Field Progression | Total | |
|---|---|---|---|
| PG | Perimetric glaucoma patients | 48 | 177 |
| GS | 1: OHT | 15 | 88 |
| PPG | 2: Abnormality in ONH or RNFL | 23 | 187 |
| PPG | 3: OHT and ONH or RNFL abnormality | 2 | 22 |
| GS | 4: Fellow eye of PG patient | 1 | 13 |
| SAP Parameters | Perimetric Glaucoma | Glaucoma Suspect and Preperimetric Glaucoma | P Value a |
|---|---|---|---|
| VFI (%/y) | −0.44 ± 0.059 | −0.070 ± 0.023 | <.001 |
| MD (dB/y) | −0.18 ± 0.025 | −0.054 ± 0.014 | <.001 |
| PSD (dB/y) | 0.073 ± 0.022 | 0.017 ± 0.0075 | <.001 |
a A random effect for eye was added to the mixed effect model to adjust for the intereye correlation.
| OCT Parameters | Perimetric Glaucoma | Glaucoma Suspect and Preperimetric Glaucoma | P Value a |
|---|---|---|---|
| Average RNFL | −0.75 ± 0.09 | −0.40 ± 0.064 | <.001 |
| Superior RNFL | −1.25 ± 0.17 | −0.66 ± 0.12 | <.001 |
| Inferior RNFL | −0.80 ± 0.14 | −0.38 ± 0.11 | <.001 |
| Temporal RNFL | −0.36 ± 0.13 | 0.073 ± 0.099 | .007 |
| Nasal RNFL | −0.63 ± 0.17 | −0.62 ± 0.14 | .99 |
a A random effect for eye was added to the mixed effect model to adjust for intereye correlation.
| Glaucoma Status | Significant RNFL Progression | VFI (%/y) | P Value a |
|---|---|---|---|
| Perimetric glaucoma | Yes | −0.71 ± 0.13 | .006 |
| No | −0.34 ± 0.065 | ||
| Glaucoma suspect and preperimetric glaucoma | Yes | −0.11 ± 0.050 | .27 |
| No | −0.058 ± 0.026 |
a A random effect for eye was added to the mixed effect model to adjust for the intereye correlation.
| VFI Progression Only a | RNFL Progression Only b | P Value | |
|---|---|---|---|
| No. | 63 | 75 | .35 |
| Age (y) | 61.5 ± 8.6 (40 to 77) | 61.8 ± 8.1 (41 to 80) | .71 |
| Baseline RNFL | 83.3 ± 14.2 (58.0 to 127.9) | 89.1 ± 14.1 (49.1 to 123.6) | .02 c |
| Baseline VFI | 93.6 ± 10.6 (60 to 100) | 94.2 ± 10.2 (47 to 100) | .73 c |
| Baseline MD | −2.96 ± 3.88 (–14.7 to 2.0) | −1.96 ± 2.96 (–15.0 to 1.6) | .09 c |
| Baseline PSD | 4.17 ± 4.33 (1.1 to 16.5) | 3.17 ± 2.90 (1.1 to 14.2) | .11 c |
a Thirty eyes diagnosed as glaucoma suspect or with preperimetric glaucoma and 33 eyes diagnosed with perimetric glaucoma.
b Forty-five eyes diagnosed as glaucoma suspect or with preperimetric glaucoma and 30 eyes diagnosed with perimetric glaucoma.
c General estimating equation method was used to adjust for intereye correlation from the same patient.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


