Purpose
To determine the frequency of peripheral iatrogenic retinal breaks in eyes undergoing small-gauge pars plana vitrectomy.
Design
Prospective, single-center, noncomparative interventional case series.
Methods
A consecutive series of patients that underwent 23- or 25-gauge vitrectomy between July 2010 and the end of October 2010 were included in the study. We excluded patients with retinal detachment, dislocated crystalline lens from complicated cataract surgery, endophthalmitis, and previous history of eye trauma or vitrectomy. We recorded prospectively the frequency of all retinal breaks noted during surgery of patients undergoing 23- or 25-gauge vitrectomy. The indications for vitreoretinal surgery were recorded, as were the location of retinal breaks, the presence or absence of an intact posterior hyaloid, status of lens, method of retinopexy, and use of a tamponade, together with the onset of a rhegmatogenous retinal detachment during the 3-month follow-up interval. Main outcome was rate of entry site breaks in small-gauge vitrectomy.
Results
We included 184 patients in this study. The mean age was 65.6 years (SD 13.2) and 46% were male. Retinal breaks occurred in 29 patients (15.7%) but breaks in only 6 (3.2%) were deemed to be related to the sclerotomies. Entry site breaks were not linked to the gauge of the instruments, but retinal breaks were more common in 23-gauge surgeries, although this was not statistically significant. One rhegmatogenous retinal detachment occurred in the postoperative period.
Conclusions
Entry site retinal breaks are not common in small-gauge vitrectomy.
Wide-angle viewing systems and advancement in micro-incision instrumentation has broadened the range of surgical indications for both macular and peripheral retinal pathologies. The safety profile of small-gauge vitrectomy has also been established, but rhegmatogenous retinal detachment (RRD) secondary to iatrogenic peripheral retinal breaks remains a common intraoperative and postoperative complication. Possible factors contributing to the retinal break include traction at the sclerotomy entry sites from either the insertion or removal of vitreoretinal instruments or as a consequence of incarcerated vitreous. Induction of posterior vitreous detachment (PVD) may also pose a risk for iatrogenic breaks during surgery. Thus far, specific targeted treatment of retinal breaks seems to be the most efficient strategy in minimizing the occurrence of RRD following surgery.
This prospective study was conducted to identify the incidence of retinal breaks associated with 25- and 23-gauge vitrectomy and to determine the risk of RRD in the postoperative period.
Methods
All patients undergoing a primary, small-gauge vitrectomy between July 1, 2010 and October 31, 2010 were eligible for inclusion in this study. Patients with a diagnosis of retinal detachment, endophthalmitis, or ocular trauma or undergoing vitrectomy for a dislocated crystalline lens following complicated cataract surgery were excluded. During the study period no case of 20-gauge vitrectomy was performed.
The operating surgeon completed a pro forma questionnaire at the end of each surgery and the data collated included surgical indication, age of patient, sex, lens status, and gauge of instrumentation. If the patient had undergone previous vitrectomy we excluded the patient from the study. The surgical protocol required a surgical induction of a PVD if the vitreous was still attached at the commencement of surgery. Any retinal break discovered during surgery was noted, as was its location. If applicable, the method of retinopexy and the use of tamponade was recorded.
Those patients undergoing combined cataract vitrectomy surgery had their crystalline lens removed using phacoemulsification techniques. A clear corneal approach was used in all cases and the protocol required insertion of a posterior chamber lens.
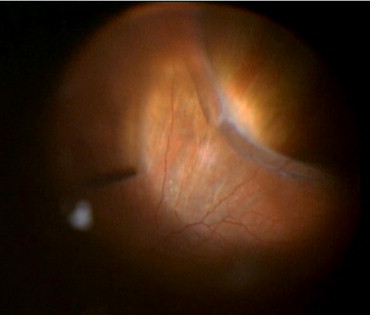
Most of the patients had regional anesthesia and all surgeries were performed using the Accurus Vitreoretinal Surgical System (Alcon Laboratories, Fort Worth, Texas, USA) and the BIOM (Oculus Inc, Wetzlar, Germany) as a wide-angle viewing system. The surgeon could select either 25- or 23-gauge instruments depending on his or her preference. In those cases where a posterior vitreous detachment was induced, the methodology involved the vitrectomy probe in a cutting-off mode, close to the optic nerve, with the aspiration setting at 600 mm Hg. In some cases, according to the preference of the surgeon, the vitreous was visualized with the use of diluted triamcinolone (10 mg/mL) during the induction of the posterior vitreous detachment. In all cases the vitreous was removed up to the far periphery. The vitreous was meticulously removed around the ports and the infusion line. At the completion of the surgery the peripheral retina was examined using scleral depression. This was achieved by illuminating the retina with a light pipe in the vitreous cavity, using the BIOM imaging system ( Figure ). In some cases the infusion pressure was reduced to enable adequate indentation, which was achieved with a standard squint hook. The inactive port was routinely plugged during this maneuver.
The surgeries were performed by 4 surgeons, either an experienced consultant or a fellow in training who had previously performed in excess of 250 supervised vitrectomies. Retinal breaks were considered entry site breaks if they were located within 1 clock hour of the sclerotomy. As for retinal breaks occurring elsewhere, the number and location were noted. All patients were followed for a minimum of 3 months, ensuring that any early postoperative RRD was detected.
Statistical analysis was performed using the SAS 9.1 system (SAS Institute, Inc, Cary, North Carolina, USA). In order to investigate factors associated with the occurrence of a break, logistic regression was used with break or not as the outcome; and age, lens status, type of operation, induction PVD, and gauge as explanatory variables. χ 2 and independent t test were used to compare results between groups. P < .05 was considered statistically significant.
Results
The cohort consisted of 184 consecutive patients undergoing pars plana vitrectomy using small-gauge vitrectomy. The mean age of the patients was 65.6 years (standard deviation [SD] 13.2). Eighty-five of the patients (46.2%) were male and 99 (53.8%) were female. The mean time of surgery was 60.9 minutes (30−120 minutes, SD 16.08). The indications for surgery were epiretinal membrane in 74 patients (40.2%), macular hole in 32 patients (17.4%), vitreous hemorrhage in 35 patients (18.9%), traction retinal detachment attributable to proliferative diabetic retinopathy in 17 patients (9.2%), vitreomacular traction in 9 patients (4.9%), floaters in 10 patients (5.4%), and others in 7 patients (4%). Ninety-eight patients (53.2%) had 23-gauge vitrectomy. In 80 patients (43.5%) a PVD was induced. We did not find any difference in the mean age of those patients undergoing surgical induction of a vitreous detachment and those that had PVD present at time of surgery (63.7 years [SD 13.4] vs 67.1 years [SD 13] respectively; P = .98). In 29 eyes (15.7%) a retinal tear was identified. Two eyes had more than one break. Fourteen of the 29 eyes with retinal breaks (48%) had posterior breaks or breaks related to diabetic traction membranes. Eleven of those breaks occurred in eyes that underwent a surgical induction of a PVD, whereas 18 breaks developed in eyes that had undergone a spontaneous PVD prior to surgery ( P = .51). Six of 184 the retinal breaks (3.2%) were deemed entry site related, all of which had a PVD prior to surgery. All retinal breaks found were treated with either endolaser photocoagulation or cryotherapy. In a logistic regression analysis the only variable that could be demonstrated to be related to break formation was the gauge of vitrectomy. Retinal breaks were more likely to be associated with 23-gauge vitrectomy ( P = .007) (odds ratio 5.8; 95% confidence interval [CI] 1.6−20.8). In all, retinal breaks were found in 25 eyes undergoing 23-gauge vitrectomy, whereas only 4 eyes developed breaks with 25-gauge surgery ( P < .001). Conversely, only 2 entry site breaks occurred with 23-gauge vitrectomy, whereas 4 such breaks were seen with the 25-gauge approach. This difference did not reach statistical significance ( P = .32). No correlation was found between time of surgery and retinal breaks ( P = .3).
There was no preference with respect to instrument gauge for either macular hole or epiretinal membrane surgeries. However, for diabetic vitrectomy 23-gauge vitrectomy was favored. A nonlogistic regression analysis demonstrated that the absolute numbers of retinal breaks were related to the surgical indication ( P = .011). The distribution of retinal breaks and entry site breaks according to indication for surgery are presented in the Table . The incidence of retinal break was 8.1% in epiretinal membrane peel, 12.5% in macular hole surgery, 28.5% in vitreous hemorrhage, and 41.1% in diabetic traction retinal detachment.
| Indication For Surgery | Overall Breaks, n (%) | Entry Site Breaks, n (%) |
|---|---|---|
| Epiretinal membrane | 6 (20.7) | 1 (16.6) |
| Macular hole | 4 (13.8) | 1 (16.6) |
| Vitreous hemorrhage | 10 (34.4) | 3 (50) |
| Traction retinal detachment in proliferative diabetic retinopathy | 7 (24.1) | 0 |
| Vitreomacular traction | 1 (3.5) | 0 |
| Floaters | 0 | 0 |
| Other | 1 (3.5) | 1 (16.6) |
Eighty-four of the 184 patients in this series (45.6%) were phakic; in 15 patients a break was found, and in 3 patients the break was identified as an entry site break. Forty-nine patients (26.6%) were pseudophakic; in 3 patients a break was found, and in 1 patient it was identified as an entry site break. Fifty patients (27.1%) underwent combined cataract vitrectomy surgery; in 10 patients a break was found, and in 2 patients the break was identified as an entry site break. More breaks were found in patients with phakic eyes and those undergoing combined surgeries than in pseudophakic patients. However, the risk of entry site breaks in these 3 groups was not found to be statistically significantly different ( P = .94). As to the risk of RRD, only 1 eye (0.5%) developed this complication within 3 months of surgery, and that was in a patient who underwent an epiretinal membrane peel.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


