Purpose
To investigate the responses to photodynamic therapy (PDT) in patients with polypoidal choroidal vasculopathy (PCV) that show large aneurysmal dilation with internal angio-architecture consisting of diverse patterns of curvilinear vessels and polyps resembling grape clusters.
Design
Retrospective, interventional case series.
Methods
Twenty-two eyes of 22 patients were included. All patients initially received PDT monotreatment. The main outcome measures were the rates of complete polyp regression on indocyanine green angiography and initial favorable responses observed clinically. Also, the rates of recurrent exudative changes were evaluated at the 2-year follow-up. We focused on changes in the vascular features and their clinical association.
Results
Complete regression of polypoidal lesions was observed in 21 eyes (95%) after a mean of 1.7 PDTs. However, favorable clinical responses were achieved in only 9 eyes (41%), and 6 of them had recurrent exudation. Main vessels, previously consisting of the polypoidal lesion frame, persisted. Additionally, aberrant vessels with a thin radiating or tortuous configuration were observed in the area where large aneurysmal dilation was present. Leakage from this vascular complex or an expanded vascular complex was observed in a total of 14 eyes (64%) during the 2-year follow-up, contributing to persistent (8 eyes) or recurrent (6 eyes) exudation. This seemed to represent secondary choroidal neovascularization (CNV). In another 4 eyes (18%), fibrous changes developed immediately after PDT. Polyps recurred in 8 eyes (38%).
Conclusions
This PCV pattern frequently evolved into typical CNV after PDT, resulting in persistent or recurrent exudation despite the disappearance of polypoidal structures.
It is generally accepted that polypoidal choroidal vasculopathy (PCV) has a better visual prognosis than does typical neovascular age-related macular degeneration (AMD), as progression is slow and subretinal fibrous proliferation is unusual. Abnormal vasculature in patients with PCV consists of a branching vascular network with polypoidal lesions at the lesion borders. However, marked variability is observed in the size, morphology, and pattern of the abnormal vasculature. Uyama and associates noted that a cluster of grape-like polypoidal lesions was active and tended to bleed or leak. They concluded that development of such lesions indicates a high risk for severe visual loss. Sho and associates reported that this pattern of polypoidal lesions was observed in 10 of 110 eyes with PCV (9%) and was closely associated with development of typical choroidal neovascularization (CNV) and fibrous proliferation. Additionally, in a series of 12 eyes, Tateiwa and associates reported that clustered polypoidal dilations formed at the end of large vascular networks expanding across the retinal vascular arcade and caused large serous and/or hemorrhagic pigment epithelial detachments (PEDs). They suggested that this type of PCV lesion had the characteristics of CNV observed in exudative AMD.
Many reports have demonstrated excellent short-term efficacy of photodynamic therapy (PDT) for treating PCV. Complete polyp regression was achieved in 80% to 95% of cases, which was well translated into resolution of the exudative changes and stabilization or improvement of the vision at the 1-year follow-up. Persistence of the branching vascular network and polyp recurrence remain key limitations of PDT, and the visual outcomes at 3 or even 2 years are not as good as those at 1 year. Small vascular lesions, better initial vision, less hemorrhage, and the absence of subfoveal polyps have been suggested as pretreatment factors favoring better visual outcomes.
However, no study has investigated the treatment response to PDT in patients with clustered polyps. Furthermore, no widely recognized criteria have been reported for clustered polyps. We investigated the responses to PDT in a subset group of patients with PCV showing characteristic features on indocyanine green angiography (ICGA): large aneurysmal dilation in the late phase of ICGA, with internal angio-architecture consisting of diverse patterns of curvilinear vessels and polyps resembling grape clusters in the earlier phase.
Methods
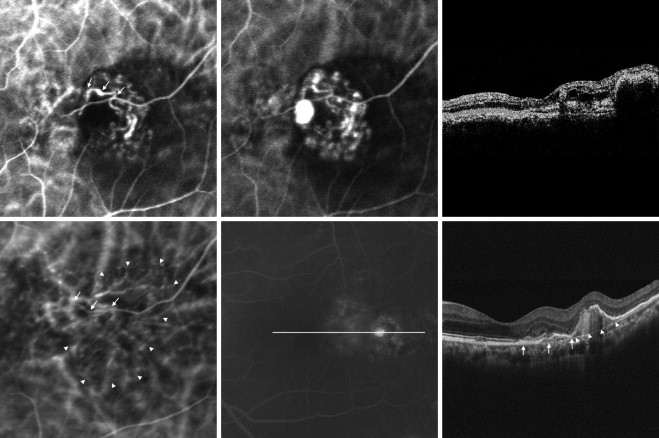
A total of 180 patients (205 eyes) newly diagnosed with PCV underwent PDT with verteporfin (Visudyne, Novartis Pharma AG, Basel, Switzerland) monotherapy as an initial treatment between December 2003 and March 2008 at Seoul St. Mary’s Hospital (known as Kangnam St. Mary’s Hospital before May 2009), The Catholic University of Korea. The diagnosis of PCV was based on ICGA findings of polypoidal dilations with or without branching vascular network. According to the observation by Yuzawa and associates, a cluster of grape-like polypoidal lesions in this study was defined as follows: 1) large reddish-orange aneurysmal dilation with the longest axis of 1500 μm or longer on a fundus photograph; 2) a hyperfluorescence corresponding to the aneurysmal dilation on late-phase ICGA; 3) appearance of curvilinear, tortuous, or looped vessels branching into smaller vessels first, followed by sprouting of numerous polyps of diverse size from these vessels showing an appearance similar to grapes in the earlier phase of ICGA ( Figure 1 ) . Patients with symptomatic lesions involving the macula and recent-onset (within the last 6 months) visual symptoms were selected for study, to include 22 patients (22 eyes) with at least 24 months of follow-up. Although 26 consecutive patients (27 eyes) were eligible, 4 patients (5 eyes) were excluded for lack of follow-up. Patients with progressed PCV, showing a cluster of polypoidal dilations at the margin of widespread retinal pigment epithelial (RPE) atrophy in the posterior pole, were excluded, as were patients with previous treatment for PCV. Lesions with coexisting typical CNV were also excluded.

PDT was administered in a full-fluence dose according to the standard protocols of the Treatment of Age-Related Macular Degeneration with Photodynamic Therapy Study after obtaining informed consent. However, the laser-spot size was chosen according to ICGA findings to cover all polyps and the branching vascular network plus an extra margin of 1 mm. Retreatment was applied at 3- to 4-month intervals, and the endpoint of the treatment was complete regression of the polypoidal lesions on ICGA. However, additional PDT was not performed consecutively if complete polyp regression was not achieved after 3 consecutive PDTs, or if there were persistent exudative changes despite polyp regression. Additional PDT was not performed when fibrous scarring developed. We defined initial favorable responses to PDT as complete regression of polyps on ICGA, a decrease or flattening of PED, resolution of macular exudative changes confirmed by optical coherence tomography (OCT) and/or cessation of leakage on fluorescein angiography (FA), maintenance or improvement of visual acuity, and a quiescent period of at least 6 months with no treatment. For the eyes not showing initial favorable responses and eyes showing recurrent serous changes after initial favorable responses, further treatments were performed using PDT, laser, intravitreal injection of 4 mg triamcinolone acetonide (Dongkwang Pharmaceutical, Seoul, South Korea), or an intravitreal injection of 1.25 mg of bevacizumab (Avastin, Genentech, Inc, San Francisco, California, USA). However, these treatments were not performed according to a uniformly designed protocol.
All patients received a comprehensive ocular examination including measurement of best-corrected Snellen visual acuity (BCVA) and dilated fundus examination with slit-lamp biomicroscopy at baseline and at each follow-up visit. During the period in which PDT monotreatments were used, all patients were regularly followed up at 3- to 4-month intervals, and FA, ICGA, and OCT were performed at each visit as well as at baseline. After this period, follow-up intervals were 1 to 4 months depending on lesion activity and/or switched treatment modality, and FA, ICGA, and OCT were performed at times determined on a patient-by-patient basis. ICGA was performed with a confocal scanning laser ophthalmoscope (SLO) (Heidelberg Retina Angiograph, Heidelberg Engineering, Heidelberg, Germany). For the OCT examination, Stratus OCT (Carl Zeiss Meditec, Dublin, California, USA) was used primarily, and spectral-domain OCT (Cirrus OCT, Carl Zeiss Meditec) was also used once it became available.
The main outcome measures were the rates of complete polyp regression on ICGA after PDT and the initial favorable responses observed clinically. The rates of recurrent exudative changes were evaluated in eyes with initial favorable responses at 2 years. Additionally, the changes in vascular features on ICGA and their association with clinical features were evaluated.
Results
Baseline Characteristics
The Table summarizes patient characteristics and their treatment results. We studied 22 eyes in 22 patients, 9 of whom were women. The mean age of the patients was 66 years (range, 55–83 years). The mean follow-up period was 43.8 months (range, 24–94 months). Location of the polypoidal lesions was subfoveal or juxtafoveal in 19 eyes and extrafoveal in 3 eyes. The mean length of the longest axis of aneurysmal dilation was 1678 μm (range, 1500–2230 μm), and the mean greatest linear dimension of the entire PCV lesion was 3040 μm (range, 1810–4560 μm). Twenty-one eyes (95%) presented with PED larger than 1 disc diameter in size (range, 1–4 disc diameters): serous PED in 12 eyes and hemorrhagic PED in 9 eyes. Fellow eye findings were a disciform scar in 4 eyes and PCV in 2 eyes. No abnormalities were observed in 16 fellow eyes. The median baseline BCVA was 20/63 (range, 20/200–20/32).
| Case | Sex/Age | Location of Polypoidal Lesion | Initial Major Fundus Findings | Polyp Regression/Required No. of PDT | Post-PDT Hm | Initial Clinical Response to PDT | Recurrence/Time of Recurrence (mo) | Origin of Recurrent or Persistent Fluid | No. of Additional Tx During 2 Years of FU | Final Major Fundus Findings | BCVA | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| PDT | IVTA | IVB | Laser | Initial | At Time of Stopping PDT | 24 Months | ||||||||||
| 1 | F/74 | Subfoveal | Hemorrhagic PED | Yes/3 | Early disciform scarring | Disciform scar | 20/100 | 20/200 | 20/334 | |||||||
| 2 | F/70 | Subfoveal | Hemorrhagic PED | Yes/1 | Yes | Early disciform scarring | Disciform scar | 20/100 | 20/200 | CF | ||||||
| 3 | F/66 | Subfoveal | Serous PED | Yes/2 | Favorable | Yes/6 | AVC, a later recurrent extrafoveal polyp | 2 | 1 | 3 | 1 | Mild fibrous change No macular fluid | 20/50 | 20/50 | 20/63 | |
| 4 | F/71 | Subfoveal | Hemorrhagic PED | Yes/1 | Early disciform scarring | Disciform scar | 20/200 | 20/500 | 20/1000 | |||||||
| 5 | M/67 | Subfoveal | Serous PED | Yes/2 | Yes | Persistent SSRD | AVC, a later recurrent juxtafoveal polyp | 1 | 2 | Disciform scar | 20/63 | 20/200 | 20/500 | |||
| 6 | M/63 | Subfoveal | Serous PED | Yes/2 | Yes | Favorable | Yes/9 | AVC, a later recurrent subfoveal polyp | 2 | 1 | 5 | Mild fibrous change Macular fluid | 20/32 | 20/40 | 20/200 | |
| 7 | M/61 | Subfoveal | Serous PED | Yes/2 | Favorable | Yes/9 | Recurrent subfoveal polyp, later AVC a | 1 | 6 | Disciform scar | 20/100 | 20/32 | 20/1000 | |||
| 8 | F/57 | Subfoveal | Serous PED | Yes/3 | Yes | Persistent SSRD | AVC a | 1 | 1 | 9 | Disciform scar | 20/125 | 20/50 | 20/500 | ||
| 9 | M/64 | Extrafoveal | Serous PED | Yes/1 | Favorable | Yes/9 | AVC a of mesh-like aberrant vessels | 1 | 1 | 8 | Large PED | 20/63 | 20/25 | 20/63 | ||
| 10 | M/66 | Subfoveal | Hemorrhagic PED | Yes/3 | Early disciform scarring | Disciform scar | 20/50 | 20/125 | 20/500 | |||||||
| 11 | F/70 | Subfoveal | Hemorrhagic PED | Yes/1 | Persistent SSRD | AVC a | 4 | Disciform scar | 20/32 | 20/32 | 20/500 | |||||
| 12 | F/65 | Subfoveal | Serous PED | Yes/2 | Favorable | No | No macular fluid RPE atrophy | 20/100 | 20/50 | 20/40 | ||||||
| 13 | F/75 | Subfoveal | Serous PED | Yes/2 | Persistent SSRD | AVC a | 9 | Macular fluid | 20/200 | 20/125 | 20/160 | |||||
| 14 | M/60 | Subfoveal | Hemorrhagic PED | Yes/1 | Favorable | Yes/11 | AVC a | 5 | Mild fibrous change Macular fluid | 20/40 | 20/25 | 20/500 | ||||
| 15 | F/57 | Juxtafoveal | SSRD | Yes/3 | Persistent SSRD | AVC a | 6 | Macular fluid | 20/25 | 20/25 | 20/40 | |||||
| 16 | M/66 | Extrafoveal | Hemorrhagic PED | Yes/1 | Yes | Persistent PED | AVC a of mesh-like aberrant vessels, later recurrent juxtafoveal polyp | 2 | 13 | Large PED | 20/32 | 20/40 | 20/100 | |||
| 17 | M/71 | Subfoveal | Serous PED | Yes/1 | Favorable | No | No macular fluid RPE atrophy | 20/200 | 20/125 | 20/160 | ||||||
| 18 | M/64 | Subfoveal | Hemorrhagic PED | Yes/1 | Favorable | Yes/9 | AVC, a later recurrent extrafoveal polyp | 4 | 1 | No macular fluid RPE atrophy | 20/160 | 20/63 | 20/63 | |||
| 19 | M/62 | Subfoveal | Serous PED | Yes/1 | Persistent SSRD | AVC, a later recurrent subfoveal polyp | 2 | 14 | Macular fluid | 20/80 | 20/40 | 20/40 | ||||
| 20 | M/55 | Subfoveal | Serous PED | Yes/2 | Yes | Persistent SSRD | AVC, a later recurrent subfoveal polyp | 1 | 12 | Large PED | 20/40 | 20/50 | 20/125 | |||
| 21 | M/69 | Subfoveal | Serous PED | No/3 | Persistent SSRD | Remaining polyps and AVC a | 10 | Large PED | 20/50 | 20/50 | 20/100 | |||||
| 22 | M/83 | Extrafoveal | Hemorrhagic PED | Yes/1 | Favorable | No | No macular fluid | 20/50 | 20/32 | 20/32 | ||||||
a Abnormal vascular complex: a complex of aberrant vessels of diverse configuration, such as linear, tortuous, looping, or branching pattern, observed at the area where large polypoidal lesion was previously located with or without the persistent vessels of branching vascular network, or expansion of this vascular complex.
Polyp Regression, Favorable Clinical Responses, and Changes in Vascular Features After Photodynamic Therapy
Polypoidal lesions resembling grape clusters regressed completely on ICGA in 21 of 22 eyes (95%) after a mean of 1.7 PDT (range, 1–3): 10 eyes after a single PDT, 7 eyes after 2 PDTs, and 4 after 3 PDTs. However, favorable clinical responses as defined in our study were achieved in 9 eyes (41%).
All eyes with discernible branching vascular network on pre-PDT ICGA showed persistence of the branching vascular network after PDT. Besides a persistent branching vascular network, aberrant vessels of diverse configuration, such as linear, tortuous, radiating, or a branching pattern, were observed where large polypoidal lesions had been located in all 21 eyes achieving complete regression of polyps. Dot-like hyperfluorescences accompanied some cases. Irregular elevation of the RPE layer was observed on OCT at the corresponding area. Spectral-domain OCT in selected cases showed an irregularly elevated RPE line and a thin, straight, highly reflective line representing the Bruch membrane beneath the RPE line. Between these 2 lines, aberrant vessels were observed as materials of moderate reflectivity. We compared the running course and branching pattern of these aberrant vessels on post-PDT ICGA with those of the main vessels consisting of the frame of polypoidal dilation on pre-PDT ICGA in 10 selected eyes showing clearly definable vasculature. In all eyes, similar configurations were detected between them, at least in part ( Figure 2 ) . The vessels were connected and intermingled with the persistent branching vascular network, when present, and formed an abnormal vascular complex. The abnormal vascular complex had extended beyond the boundary of the pretreatment PCV lesion in 15 eyes. Leakage from this vascular complex was observed on FA, resulting in persistent exudation despite polyp regression in 8 of 22 eyes (36%): persistent PED in 2 eyes and persistent serous sensory retinal detachment in 6 eyes despite a decrease or flattening of PED. Fibrous changes developed in 4 of 22 eyes (18%) ( Figure 3 ) . Post-PDT hemorrhage (hemorrhage within 1 month after PDT) developed in 6 of 22 eyes (27%). In 1 eye, the hemorrhage extended to the temporal vascular arcade, so tissue plasminogen activator and gas were injected to disperse the blood from the fovea.

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


