Purpose
To assess refractive error after cataract surgery combined with Descemet stripping automated endothelial keratoplasty using adjusted keratometric (K) readings to calculate intraocular lens (IOL) power.
Design
Prospective, interventional case series.
Methods
One eye of 39 consecutive patients with Fuchs endothelial dystrophy and cataract were included. To calculate IOL power before surgery, the Javal steep and flat K readings (Haag-Streeit) were adjusted by reducing their value by −1.19 diopters (D); the axial length was measured by immersion biometry, and the standard A-constant was used. Surgery included phacoemulsification, IOL (Acrysof SN60AT; Alcon) implantation within the capsular bag, and Descemet stripping automated endothelial keratoplasty using posterior lamella prepared with a 300-μm head microkeratome (Moria). The absolute prediction error (absolute difference between predicted and achieved refraction) was assessed 6 months after surgery.
Results
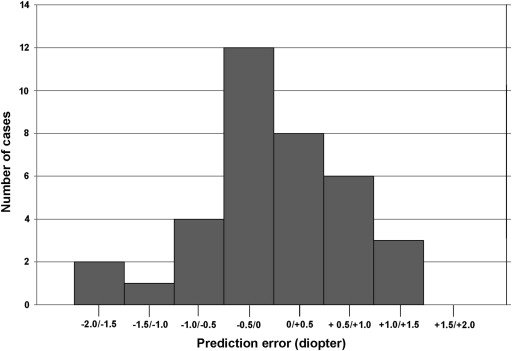
The mean power of the implanted IOL was 23.22 ± 2.90 D. The mean predicted and achieved refractions were −0.27 ± 0.26 D and −0.23 ± 0.73 D, respectively. The mean absolute prediction error was 0.59 ± 0.42 D (range, 0.05 to −1.52 D). The postoperative spherical equivalent fell within ±0.50 D, ±1.00 D, and ±2.00 D of the predicted refraction in 55.5%, 83.3%, and 100% of cases, respectively. Had the IOL power been calculated without adjusting the K readings, the mean absolute prediction error would have been significantly higher (0.86 ± 0.62 D; P = .04).
Conclusions
In this study, in which posterior lamellae were prepared using a 300-μm head microkeratome, adjusting preoperative K readings by −1.19 D led to accurate IOL power calculation and highly predictable refractive error after cataract surgery combined with Descemet stripping automated endothelial keratoplasty.
Endothelial diseases of the cornea are the leading indication for corneal graft and frequently are associated with cataract. In recent years, the combined intervention comprising phacoemulsification, intraocular lens (IOL) implantation, and Descemet stripping automated endothelial keratoplasty (DSAEK) has emerged as the preferred surgical technique for treating these cases. What has been called the new triple procedure offers numerous advantages over the standard technique, comprising penetrating keratoplasty and cataract extraction. The main advantages of the new procedure are that surgery is performed through a small incision, corneal innervation and biomechanical strength are preserved, the change in corneal refractive power is moderate, and visual recovery is faster.
Patients scheduled for the new triple procedure have high expectations of visual recovery. However, accurate IOL power calculation, and consequently predictable refractive results, can be difficult to achieve in these patients because the posterior lamellar graft alters the corneal power that was computed before surgery in the IOL calculation formula. A number of studies have shown that microkeratome-prepared posterior lamellas lead to a reduction of corneal power. To compensate for this change, the keratometric (K) readings used in the IOL calculation formula may be adjusted to take the expected reduction into account. This method was applied in this study in candidates for the new triple procedure, with the aim of assessing the accuracy of IOL power calculation and postoperative refractive error.
Methods
The study was registered at the Department of Clinical Physiopathology, University of Turin (reference 04-med30-2009). It was performed with the approval of the Institutional Review Board of Turin Eye Hospital and was conducted in accordance with the tenets of the Declaration of Helsinki. The aims of the study and the study design were explained clearly to patients, and if in agreement, they then signed an informed consent form. All included patients consented to participation.
This prospective, interventional case series included consecutive eyes with Fuchs endothelial dystrophy and cataract scheduled for phacoemulsification, IOL implantation, and DSAEK at the Ophthalmology Institute of Turin University between March 2009 and April 2011. Patient eligibility was determined by a clinical examination that included slit-lamp examination, specular microscopy, Pentacam tomography (Oculus, Wetzlar, Germany), and ultrasound pachymetry. A patient was invited to participate in the study if the primary investigator (U.d.S.) judged that both Fuchs endothelial dystrophy and cataract reduced the patient’s Snellen corrected distance visual acuity (CDVA) to less than 0.5, and thus both conditions required surgical intervention. Key exclusion criteria included a history of ocular surgery or trauma, irregular astigmatism, scarring or severe edema of the corneal stroma, and capsular or zonular anomalies of the lens. If a patient was scheduled for surgery in both eyes during the study period, only the first eye entered the study.
Preoperative data, surgical details, and postoperative results were recorded on a standardized form, and then were transferred to a computerized database. Preoperative data included patient age and gender, Snellen uncorrected distance visual acuity and CDVA, refraction, ocular comorbidities expected to reduce CDVA to less than 0.5, K readings, and axial length. Surgical details included intraoperative complications and dioptric power and predicted refraction of the implanted IOL. Postoperative data included refraction, Snellen uncorrected distance visual acuity and CDVA, and any complications.
Intraocular Lens Power Calculation
The dioptric power of the steep and flat corneal meridians was measured using the Javal-Schiotz keratometer (Haag-Streit, Koeniz, Switzerland). The 2 values then were reduced by −1.19 diopter (D) to obtain what, for the purposes of this study, were termed adjusted K readings . The adjustment factor applied was the average reduction of corneal power that had been found in post-DSAEK corneas in a previous study. The adjusted K readings then were used in the IOL calculation formula.
The axial length was measured using an immersion technique with the Ocuscan (Alcon, Inc, Fort Worth, Texas, USA) A-scan biometer. The ultrasound speed was set at 1532 m/second for the anterior chamber and vitreous and 1641 m/second for the lens. After administration of topical anesthesia, the patient assumed a reclined position, and the Prager scleral shell, with a 10-MHz A-scan probe in place, was introduced into the palpebral fissure. The scleral shell was filled with sterile saline solution as a coupling medium. The patient was instructed to fixate the target light, and 10 consecutive measurements were obtained. If the standard deviation of these measurements was less than 0.05 mm, the average value was recorded.
The IOL used in this study was the 1-piece foldable acrylic AcrySof SN60SAT (Alcon, Inc). The required IOL power was calculated using the standard A-constant of 118.4 and the formulas built into the A-scan biometer. The Sanders-Retzlaff-Kraff (SRK)/T formula was used in eyes with an axial length of more than 21 mm, and the Hoffer Q formula was used in eyes with an axial length of less than 21 mm.
Surgical Technique and Postoperative Management
All operations were performed by the same surgeon (U.d.S.) using a standardized procedure. First, the posterior lamella was prepared from sclerocorneal tissue preserved in organ-culture medium and selected by the Piedmont Cornea Bank, following European Eye Bank Association guidelines. The sclerocorneal tissue was mounted onto the artificial anterior chamber, and the epithelium was removed with a cellulose sponge. The pressure in the anterior chamber was raised to 70 to 80 mm Hg by injecting balanced salt solution with a 20-mL syringe. The tissue was sectioned using a microkeratome (CBM-ALTK; Moria, Antony, France) equipped with a 300-μm head, passing the microkeratome slowly through the tissue in 4 to 5 seconds. The posterior lamella then was cut onto the Hanna punch block (Moria) using an 8.00- to 9.00-mm trephine.
All recipients were operated on under monitored care using peribulbar anesthesia. Phacoemulsification was performed through a 2.75-mm clear corneal temporal incision, and the IOL was placed within the capsular bag using a Monarch III injector. A 20-gauge anterior chamber maintainer was introduced through a limbal paracentesis, and the Descemet membrane and endothelium were stripped. The posterior lamella was introduced through a 4.1-mm wide corneal incision on the nasal side using the pull-through technique with a Busin glide (Moria). The corneal incisions were closed with 2 interrupted 10-0 nylon sutures. An air bubble was injected to fill the anterior chamber for 10 minutes; approximately 30% of the air bubble then was removed and replaced with balanced salt solution. At the end of the procedure, the eye received 1 drop each of homatropine 5%, tobramycin 0.3%, and dexamethasone 1% solutions. The eye was patched and the patient was instructed to lie face-up for 2 hours in the recovery room to allow the remaining air bubble to push the donor tissue against the recipient cornea.
Patients received topical tobramycin 0.3% 4 times daily for 1 week and topical dexamethasone 0.1% 5 times daily for the first month, 4 times daily for the second month, and then 3 times daily until the sixth month. Postoperative examinations were scheduled 1, 7, 30, 90, and 180 days after surgery. In the case of posterior lamella detachment, the patient was taken to a minor operating room where, under sterile conditions, the donor tissue was repositioned, injecting air into the anterior chamber through a limbal paracentesis. Corneal sutures were removed 30 days after surgery. Supplementary examinations were arranged according to the needs of individual cases.
Outcome Measures and Statistical Analysis
The end point of the study was to assess the mean absolute prediction error. It was calculated in each eye as the absolute value of the difference between predicted and achieved refraction. Predicted refraction was taken from the biometry reading of the IOL selected. Achieved refraction was the spheroequivalent value of the spherical and astigmatic subjective manifest refraction, which was measured by a single expert examiner (U.d.S.) 6 months after surgery.
The absolute prediction error also was assessed retrospectively using the true K readings to calculate the IOL power; the true K readings were introduced into the calculation formula, whereas the predicted refraction of the implanted IOL was extracted from the biometry reading. The absolute difference versus the achieved refraction then was calculated.
Statistical analysis was performed using SPSS for Windows, version 17.0 (SPSS, Inc, Chicago, Illinois, USA). Before comparison between groups, the Shapiro-Wilk test was used to check the normality of data distribution. The paired t test was used to compare normally distributed variables; the nonparametric Mann–Whitney rank-sum test was used to compare nonnormally distributed variables. The χ 2 or the Fisher exact test were used to investigate differences in the proportion of eyes in which achieved refraction fell within ±0.50 D, ±1.00 D, and ±2.00 D of predicted refraction. Differences were considered statistically significant when the P value was less than .05.
Results
One eye of 39 patients (24 women and 15 men) with endothelial Fuchs dystrophy and cataract who were scheduled for the combined intervention was included in the series. Mean patient age was 68.3 ± 9.9 years (range, 52 to 84 years). Before surgery, mean Javal steep and flat K readings were 44.06 ± 1.62 D and 43.32 ± 1.32 D, respectively. Mean axial length was 23.07 ± 0.95 mm (range, 21.44 to 25.68 mm).
Three eyes were excluded from the analysis. These cases included 2 eyes lost to follow-up (5.13%) and 1 eye in which a 3-piece foldable IOL was implanted in the ciliary sulcus because of posterior capsule rupture (2.56%). In all other cases, the AcrySof SN60SAT was implanted regularly within the capsular bag. The mean IOL power was 23.22 ± 2.90 D (range, 16.00 to 28.50 D). Six months after surgery, mean predicted and achieved refraction were −0.27 ± 0.26 D (range, 0.21 to −0.81 D) and −0.23 ± 0.73 D (range, 1.37 to −1.5 D), respectively. The mean absolute prediction error was 0.59 ± 0.42 D (range, 0.05 to 1.52 D). The difference between achieved and predicted refraction had a positive value in 17 eyes and a negative value in 19 eyes ( Figure 1 ). The achieved refraction fell within ±0.50 D, ±1.00 D, and ±2.00 D of the predicted refraction in 55.5%, 83.3%, and 100% of cases, respectively ( Table ).

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


