Purpose
To prove the hypothesis that during cataract surgery, repeated irrigation of the operative field with povidone–iodine of 0.25% reduces the anterior chamber bacterial contamination rate at completion of operation.
Design
Prospective, interventional case series.
Methods
In 404 consecutive eyes, the operative field was irrigated with infusion fluid in 202 eyes (group A) and with 0.25% povidone–iodine in 202 eyes (group B). Bacteriologic culture was performed using the following samples: ocular surface fluid after lid speculum placement and anterior chamber fluid at the completion of surgery. Anterior chamber fluid samples were collected at the beginning and completion of surgery for iodide ion concentration measurement. Corneal endothelial cell density was measured using a specular microscope before surgery and on day 7 after surgery.
Results
Bacterial detection rate in ocular surface fluid was not significantly different between group A (5.5%) and group B (6.0%), but the rate in anterior chamber fluid was significantly ( P = .0017) reduced in group B (0%) compared with group A (5.0%). Iodide ion concentrations at the start and end of surgery were 7.5 ± 0.7 μg/mL and 3.5 ± 0.7 μg/mL, respectively, in group B and less than 0.1 μg/mL both at the start and end of surgery in group A. Corneal endothelial cell densities were not significantly difference between groups A and B before surgery (2614 ± 233/mm 2 vs 2534 ± 173/mm 2 ; P = .2254) and 7 days after surgery (2463 ± 269/mm 2 vs 2338 ± 204/mm 2 ; P = .4044).
Conclusions
In cataract surgery, repeated irrigation of the operative field with povidone–iodine at a concentration of 0.25% achieved an extremely low bacterial contamination rate in the anterior chamber at the completion of surgery.
The incidence of endophthalmitis after cataract surgery has been reported to be 0.048% (109 of 225 471 eyes) in a 2007 Swedish study and 0.052% (52 of 100 539 eyes) in a 2007 Japanese study. In the Swedish study, the incidence of endophthalmitis was 0.053% for clear corneal incisions and 0.036% for sclerocorneal incisions ( P = .14), as well as 0.040% for superior incisions and 0.055% for temporal incisions ( P = .14). In the Japanese study, the incidence was 0.049% for scleral incision and 0.043% for clear corneal incision, with no significant difference. Endophthalmitis is a serious surgical complication. Even with appropriate treatments, the final visual acuity is unfavorable and is reported to be less than 20/200 (35.7%) or 20/200 to 20/40 (36.7%). Because many patients with endophthalmitis worldwide are at risk of blindness, prevention of this complication is an important issue.
Investigations of the species and genetics of the bacteria causing endophthalmitis after cataract surgery revealed that endophthalmitis is caused by the bacterial flora inhabiting the eyelid and conjunctiva, which gain access to the eye. The addition of antibiotics to the infusion fluid has been reported to reduce the anterior chamber bacterial contamination rate significantly from 21.1% to 6.8% in one study and from 21.1% to 7.7% in another study. These results raise the question of why the anterior chamber remains contaminated by bacteria at the rates of 6.8% and 7.7% even after the addition of antibiotics. One of the reasons is that a safe concentration of vancomycin (20 μg/mL) or gentamicin (8 μg/mL) in the irrigation fluid requires more than 140 minutes to exhibit bactericidal effect, whereas the half-life of antibiotics in the anterior chamber is only 51 minutes. Another concern about using vancomycin is an increased incidence of cystoid macular edema after cataract surgery with intraocular vancomycin. Finally, because vancomycin is reserved for the treatment of endophthalmitis, the United States Centers for Disease Control and Prevention guidelines prohibits the addition of vancomycin to infusion fluids.
Ciulla and associates rated the evidence level of different cataract surgery bacterial endophthalmitis prophylaxis techniques and reported that preoperative irrigation with povidone–iodine has a higher clinical recommendation than antibiotic-containing irrigation solutions. Povidone–iodine has the advantages of low cost, broad-spectrum activity, fast bactericidal rate, and absence of resistance to bactericidal effects. Studies after 2000 including more than 100 eyes showed that with preoperative povidone–iodine irrigation alone, the bacterial detection rates were 5.5% to 26% from the conjunctiva at the beginning of surgery, 18% from the conjunctiva at the end of surgery, and 11.0% to 21.1% from the anterior chamber at the end of surgery. Hence, there is as yet no established aseptic technique that achieves an extremely low bacterial contamination at the end of surgery. Currently, 5% or 10% povidone–iodine is used worldwide for disinfection of the surgical field. The bactericidal effect of povidone–iodine has been observed over a wide range, from 0.005% to 10%. The time taken for povidone–iodine to kill bacteria was shorter at 0.1% to 1.0% (15 seconds) compared with 2.5% to 10% (30 to 120 seconds). Although higher dilution facilitates the release of free iodine and hence increases the bactericidal effect, the effect does not last. To obtain a sustained bactericidal effect, repeated irrigation of the operative field with a dilute solution may be efficacious. Trost and associates reported that povidone–iodine concentrations from 0.05% to 0.5% are safe for ocular tissues and at the same time highly bactericidal. In the present study, by repeatedly irrigating the operative field with 0.25% povidone–iodine during cataract surgery, we achieved an extremely low bacterial contamination rate in the anterior chamber at the end of surgery.
Methods
A total of 404 eyes of 310 patients who underwent cataract surgery at the Surugadai Hospital of Nihon University between January 2007 and February 2010 were studied. The mean patient age ± standard deviation was 65.4 ± 9.6 years (range, 48 to 92 years). All surgeries in bacterial contamination studies were performed by one of the authors (H.S.).
Preoperative antisepsis by ocular instillation of topical antibiotics (levofloxacin) 6 times daily was started the day before surgery. During surgery, flomoxef sodium was infused intravenously. All patients were draped in the usual sterile fashion, everting lashes from the operative field. Before all surgeries, the skin was scrubbed with 10% povidone–iodine (Meiji Seika, Tokyo, Japan), and the conjunctiva and cornea within the operative field were disinfected with 0.25% povidone–iodine. Before surgery, 10% povidone–iodine was diluted with physiologic saline to obtain a 0.25% solution and was used only on the day of preparation. Under topical anesthesia, 2 operative field irrigation methods were used. In group A, which consisted of 202 consecutive eyes operated between January 2007 and December 2008, the operative field was irrigated with infusion fluid (BSS PLUS; Alcon Surgical, Fort Worth, Texas, USA). In group B, which consisted of 202 eyes operated between January 2009 and February 2010, the operative field was irrigated with 0.25% povidone–iodine. Irrigation of the operative field with infusion fluid or 0.25% povidone–iodine was conducted before and after operation (2 mL, 30-second exposure) and repeated every 20 seconds during operation (0.5 mL).
After lid speculum placement, ocular surface fluid was collected (n = 400) using a 2.5-mL syringe with a 27-gauge needle. The operative field was irrigated for 30 seconds as described above. A side port incision was made while some irrigation fluid remained in the conjunctival sac. Then, an anterior chamber sample was collected (n = 4) using a 1.0-mL syringe with a 27-gauge needle. Using 2 types of viscoelastic materials, Viscoat (Alcon Surgical) and Healon (AMO, Uppsala, Sweden), phacoemulsification (20 000 Legacy; Alcon Surgical) was performed through an incision in the superior cornea. A foldable intraocular lens (SN60WF; Alcon Surgical) was inserted inside the capsule. At the completion of surgery, anterior chamber samples were collected (n = 404) using a 1.0-mL syringe with a 27-gauge needle. Subsequently, the operative field was irrigated again for 30 seconds.
For bacteriologic study, the samples were inoculated into Kenkipota II (Clinical Supply; Kakamigahara, Gifu, Japan) for enrichment and then plated on blood agar, chocolate agar, CHROMagar (Cosmo Bio, Tokyo, Japan), and MacConkey agar (Nihon Pharmaceutical, Tokyo, Japan) for isolation.
Iodine ion concentrations in the anterior chamber were measured in 4 eyes in February 2010 using anterior chamber fluid samples collected at the beginning of surgery (n = 4) and at the end of surgery (n = 4). High-performance liquid chromatography (LC-2010C HT; Shimadzu, Kyoto, Japan) was used for quantitative measurements.
Corneal endothelial cell density was determined in 400 eyes between January 2007 and February 2010 before surgery (n = 200) and on day 7 after surgery (n = 200). A specular microscope (SP 3000; Topcon, Tokyo, Japan) was used for measurements.
Statistical analysis of the data was performed using Stat View software (SAS Institute, Inc, Cary, North Carolina, USA). The Fisher exact probability test and Mann–Whitney U test were used to compare the bacterial detection rate and endothelial cell density. A P value less than .05 was considered to be statistically significant.
Results
Study 1
At the beginning of surgery, coagulase-negative Staphylococcus species (7 eyes), Micrococcus species (1 eye), Enterococcus faecalis (1 eye), Staphylococcus aureus (1 eye), and Corynebacterium species (1 eye) were isolated from the ocular surface fluid samples in group A ( Table 1 ). The bacterial detection rate was 11 in 200 (5.5%) eyes. Coagulase-negative Staphylococcus species (8 eyes), Staphylococcus aureus (2 eyes), Micrococcu s species (1 eye), and Klebsiella species (1 eye) were isolated from the ocular surface fluid samples in group B. The bacterial detection rate was 12 in 200 (6.0%) eyes. There was no significant difference in the rate of bacterial detection between groups A and B ( P > .9999).
| Group | Microbial Contamination (%): Group A (n = 200) and Group B (n = 200) | Corneal Endothelial Cell Density (/mm 2 ): Group A (n = 200) and Group B (n = 200) | Anterior Chamber Iodide Ion Concentration (μg/ml): Group A (n = 2) and Group B (n = 2) | |||
|---|---|---|---|---|---|---|
| Start of Surgery: Ocular Surface Fluid | End of Surgery: Anterior Chamber Fluid | Before Surgery | Day 7 after Surgery | Start of Surgery | End of Surgery | |
| A | 11/200 (5.5%) a : CNS (n = 7), Micrococcus species (n = 1); Enterococcus faecalis (n = 1); Staphylococcus aureus (n = 1); Corynebacterium species (n = 1) | 10/200 (5.0%) b : CNS (n = 6); Enterococcus species (n = 1); Enterococcus faecalis (n = 1); Staphylococcus aureus (n = 1); Klebsiella pneumoniae (n = 1) | 2614 ± 233 c | 2463 ± 269 d | <1 | <1 |
| B | 12/200 (6.0%) a : CNS (n = 8); Staphylococcus aureus (n = 2); Micrococcus species (n = 1); Klebsiella species (n = 1) | 0/200 (0%) b | 2534 ± 173 c | 2338 ± 204 d | 7.5 ± 0.7 | 3.5 ± 0.7 |
| P values | >.99 | .0017 | .2254 | .4044 | — | — |
a,b Fisher exact probability test, group A versus group B.
At the completion of surgery, coagulase-negative Staphylococcus species (6 eyes), Enterococcus species (1 eye), Enterococcus faecalis (1 eye), Staphylococcus aureus (1 eye), and Klebsiella pneumoniae (1 eye) were isolated from the anterior chamber fluid samples in group A. In contrast, no bacteria were detected from all the anterior chamber fluid samples in group B (0/200 eyes; 0%). The contamination rate was significantly lower in group B ( P = .0017, Fisher exact probability test).
Study 2
The iodide ion concentrations in anterior chamber fluid samples at the beginning of surgery were less than 0. 1 μg/mL in group A and 7.5 ± 0.7 μg/mL (range, 7.0 to 8.0 μg/mL) in group B, and the concentrations at the completion of surgery were less than 0.1 μg/mL in group A and 3.5 ± 0.7 μg/mL (range, 3.0 to 4.0) in group B ( Table 1 ). The concentrations were low in all the samples.
Study 3
Corneal endothelial cell densities before surgery were 2614 ± 233 cells/mm 2 (range, 2358 to 2863 cells/mm 2 ) in group A and 2534 ± 173 cells/mm 2 (range, 2318 to 2818 cells/mm 2 ) in group B, with no significant difference ( P = .2254). The cell densities at day 7 after surgery were 2463 ± 269 cells/mm 2 (range, 2188 to 2981) in group A and 2338 ± 204 cells/mm 2 (range, 2003 to 2660 cells/mm 2 ) in group B, also with no significant difference between the 2 groups ( P = .4044). Intraoperative posterior capsule damage or postoperative endophthalmitis were not observed in any of the patients.
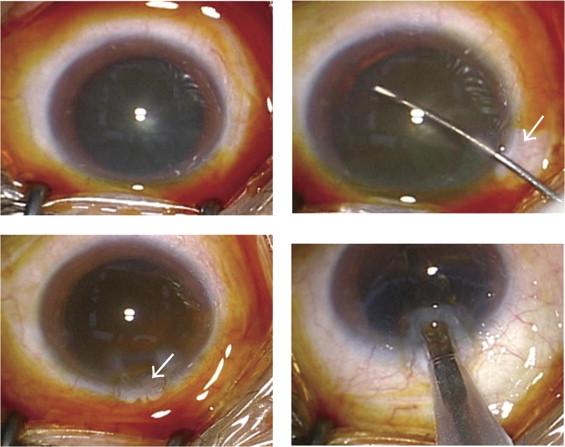
When 0.25% povidone–iodine was used to irrigate the operative field during cataract surgery, we observed that the viscoelastic material injected into the anterior chamber during continuous curvilinear capsulorrhexis prolapsed from the side port ( Figure ). The viscoelastic material also prolapsed from the corneal wound. The prolapse was readily observable because of the contrast of the transparent viscoelastic substance against the brown color of iodine on the conjunctiva surface. Thus, the use of povidone–iodine irrigation also facilitates the observation of prolapse of transparent intraocular substance from the wound, which otherwise would be missed. A part of the prolapsed material was pressed back into the eye with an injector during foldable intraocular lens implantation.